Vol. 23 - Num. 91
Original Papers
Twenty years after: prevalence and evolution of burnout in pediatrics, from 1998-1999 to 2018-2019
Martí Peiraua, Montse Esquerda Aresteb, Carme Gabarrellc, Josep Pifarred
aFacultad de Medicina. Universidad de Lleida. Lleida. España.
bFacultad de Medicina. Universidad de Lleida. Instituto Borja de Bioètica. Universidad Ramon Llull. Barcelona. Hospital Sant Joan de Déu Terres de Lleida. Lleida. España.
cPediatra ICS. Lleida. España.
dFacultad de Medicina. Universidad de Lleida. Hospital Sant Joan de Déu Terres de Lleida. Hospital Universitario Santa María-GSS. Lleida. España.
Correspondence: M Esquerda. E-mail: mesquerda@ibb.url.edu
Reference of this article: Peirau M, Esquerda Areste M, Gabarrell C, Pifarre J. Twenty years after: prevalence and evolution of burnout in pediatrics, from 1998-1999 to 2018-2019. Rev Pediatr Aten Primaria. 2021;23:253-60.
Published in Internet: 01-09-2021 - Visits: 12693
Abstract
Introduction: burnout is a chronic stress syndrome, described as a process of emotional exhaustion, depersonalization, and reduced personal accomplishment. It has a high impact both on a personal level and on healthcare quality and safety, and its prevalence is high. The present study aimed to determine the prevalence of this syndrome in paediatricians in Lleida, analyse its association with different variables and compare current results with the results of a previous study conducted in 1998.
Method: we conducted a descriptive, cross-sectional observational study analysing sociodemographic data and Maslach burn-out questionnaire scores. We compared these data to the results of the 1998 study, in which the same information was collected.
Results: a total of 42 paediatricians (64%) participated in the survey, 66% were female, and the mean age was 42.1 years. Thirty-six percent had scores suggestive of burnout syndrome with emotional exhaustion. There were no differences associated with the number of hours worked, sex, marital status, or the work setting. The paediatricians with the highest level of burnout were more likely to express disappointment and depression in relation to work and or have physical and/or mental illness. On the other hand, respondents who perceived their work as a calling and felt recognised by their organizations had higher scores in the dimension of personal accomplishment. We compared the data of this sample to the data of the 1998 study.
Conclusions: We found a high level of burnout in 36% of respondents. The data confirmed that approximately one third of paediatricians have significant levels of burnout, which is a structural problem and therefore must be addressed with strategies not only at the individual level, but also at the level of the team and the institution.
Keywords
● Emotional distress ● Medical professionalism ● Occupational stress ● Professional burnoutINTRODUCTION
Burnout (BO) is a disorder resulting from chronic workplace stress in individuals working in helping professions with a significant emotional involvement, including medicine. It is defined as exhaustion and progressive disillusionment resulting in cynicism and loss of purpose.
This is not a novel concept, as burnout was already described in the 1970s by Freudenberger1 and later defined by Maslach2, who identified 3 dimensions of burnout and developed the Maslach Burnout Inventory (MBI). These three dimensions are:
- Emotional exhaustion (EE), or feelings of being psychologically drained. There are different predictors of EE, including high levels of perceived stress, lack of acknowledgment in the job, pressure due to a lack of time or lack of incentives.2,3
- Depersonalization and cynicism (DP), which start out as a coping mechanism and progress to an unfeeling and impersonal response toward patients and colleagues.
- Personal Accomplishment (PA), involving a loss of feelings of personal achievement and the perception of reduced professional efficacy.
Maslach describes the development of BO as a continuum traversing these dimensions, starting with the emotional and physical exhaustion of the individual in relation to work. Depersonalization develops as a result of protracted emotional exhaustion, with negative attitudes towards work and the workplace. The third component, PA, develops later, with emergence of feelings of incompetence, powerlessness and decreased productivity, even when positive results are being accomplished.3-5
Traditionally, emotional exhaustion has been perceived as the most characteristic feature of burnout, but depersonalization is the dimension that has the most detrimental effect.3
Burnout is considered a silent global health care predicament6 due to its substantial impact both at the individual and health care level, and a global crisis7 due to its high prevalence. The consequences of a high level of BO are significant8,9; BO has been associated with decreased empathy,10,11 poorer quality of life, job dissatisfaction, increased depression symptoms and conflicts in the household,12 and an increased overall risk of mental health disorders.13
When it comes to clinical practice, a higher BO score correlates to decreased health care quality,14-16 an increased frequency of medical errors (mainly associated with DP),17 poorer vital sign monitoring,10,18 poorer attitude towards patients,19 and a poorer learning environment in teaching hospitals20 and in medical residencies.21
Maslach and Leiter22 defined seven risk factor categories for BO:
- Work overload, not primarily in terms of work hours but of an excessive work demand and uncertainty.23,24
- Having no control in the workplace, no agency to organise workflow, lack of participation in organizational decision-making or lack of clear expectations leading to role conflict.
- Lack of recognition for performed work.
- Lack of community or social support for the individual.
- Perceived unfairness of the management.
- Conflict between individual and organizational or professional values.
- Personal factors that do not fit with workplace expectations and hinder coping.
The prevalence of BO in the health care field is high, and BO is found in every medical speciality with a frequency that ranges from 20 to 80%.25,26 In paediatrics, several studies have found a high prevalence ranging from 25 to 70%, depending in part on the specific setting (for instance, BO is more prevalent in paediatric intensive care units), in every case with a clear impact on health care quality.27-30 Burnout is not associated with sociodemographic characteristics, ethnicity or race, and the results on its association with sex are heterogeneous.3,5,9,26
Interventions on occupational and psychosocial factors seeking to improve workloads, autonomy or the management of personal factors have been shown to improve BO.31-33
Twenty years ago, a pioneering study on BO in paediatrics practice was conducted in the population of paediatricians working in inpatient and outpatient settings in the Lleida health care area.34 In the 1998-1999 period, the overall prevalence of BO in paediatricians was 26%, and the salient findings were the association of BO with the number of worked hours and the higher prevalence of BO in paediatricians working in primary care compared to those working in hospitals. The aim of our study was to determine the current prevalence of BO in the same area and analyse changes in comparison to the 1998-1999 period.
MATERIAL AND METHODS
The study universe encompassed all paediatricians practicing in the province of Lleida. We obtained their contact information through the PediatresdePonent platform. We contacted paediatricians by sending a form through electronic mail in which we explained the study and requested their participation. We obtained written informed consent from participants. Of the 66 paediatricians registered in the platform, 42 participated in the survey.
The form had different sections: sociodemographic data, work data and the Maslach Burn Out Inventory (MBI). We classified MBI scores as low between 1 and 33 points, medium between 34 and 66 points and high between 67 and 99 points. At the scale level, we considered results abnormal if the EE score exceeded 31 points, the DP score 13 points and the PA score 30 points (based on ranges established for Spanish paediatricians)3; with higher burnout corresponding to higher levels of EE and DP and lower levels of PA.
We compared the data obtained in the survey to the data from the study by Esquerda et al., who analysed the same variables in a cohort of paediatricians in the same province in the 1998-99 period.34
The data from both studies were anonymised and entered in a spreadsheet and analysed with the SPSS software. In the analysis of quantitative data, we compared means with the Student t test after verifying the assumptions of normality (Kolmogorov-Smirnov test) and homogeneity of variance (Levene test). For comparisons of more than 2 groups, we used one-way analysis of variance (ANOVA) with the Bonferroni correction. We analysed the association between 2 quantitative variables with the Pearson correlation coefficient and the association between two or more qualitative variables with the chi square test. All tests were two-tailed with an alpha level of 5%.
RESULTS
The mean MBI score was 65.3, indicative of a medium-high level of BO. The percentage of paediatricians with high BO was 36%, compared to 26% in the 1998-99 period. This increase was not statistically significant.
Table 1 summarises the sociodemographic characteristics of the sample and Table 2 the BO scores by subscale (EE, DP and PA) in addition to the responses to the work self-evaluation questionnaire, comparing the 1998-1999 and 2018-2019 samples.
| Table 1. Sociodemographic characteristics | ||||
|---|---|---|---|---|
| 2018-19 | 1998-99 | |||
| n | % | n | % | |
|
Sex Male Female |
14 28 |
33.3 66.7 |
13 21 |
38.2 61.8 |
|
Residential setting City of Lleida Other |
29 13 |
69.7 30.3 |
25 9 |
73.5 26.5 |
| Mean age | 42.1 years | 42.15 years | ||
| Private practice | 9 | 21.4 | 12 | 35.3 |
|
Marital status Single Married/domestic partnership Divorced, widowed |
8.19 32.8 3.9 |
11.8 79.4 8.8 |
||
|
Work setting Hospital Primary care Other |
10 30 2 |
24 71 5 |
8 24 2 |
23.5 70.6 5.9 |
| Presence of disabling disease | 9 | 21.4 | 6 | 17.6 |
|
Considers pay: Very low or low Adequate High or very high |
22 12 8 |
52.4 28.6 19.1 |
27 6 1 |
79.4 17.7 2.9 |

| Table 2. Results of the Maslach Burnout Inventory (MBI) and the work self-evaluation questionnaire. Comparison of 1998-1999 and 2018-2019 samples | |||
|---|---|---|---|
| Survey period | 2018-19 | 1998-99 | Statistical significance |
| MBI, emotional exhaustion (EE), mean MBI EE >31 (burnout) (%) |
26 35.7 |
23 26.5 |
NS NS |
| MBI, depersonalization (DP), mean MBI DP >13 (burnout) (%) |
7 14.3 |
8 17.6 |
NS NS |
| MBI, personal accomplishment (PA), mean MBI PA <30 (burnout) (%) |
35.4 23.8 |
34.3 23.5 |
NS NS |
| Fulfilling work (%) | 92.9 | 73.5 | p = 0.029 |
| Considers profession a vocation (%) | 81.0 | 70.6 | NS |
| Recognition from the organization (%) | 19 | 26.5 | NS |
| Promotion opportunities (%) | 33.3 | 47.1 | NS |
| Would choose the same profession again (%) | 83.3 | 85.3 | NS |
| Would change profession (%) | 23.8 | 23.5 | NS |
| Has tried stress relief techniques (%) | 73.8 | 44.1 | p = 0.008 |
| Work-related physical or psychological disorder (%) | 63.4 | 44.1 | NS |

We found a statistically significant association between sex and the EE subscale, as EE scores were higher in female compared to male paediatricians (26.6 vs. 20.3; t = 2.28; p = 0.025). There were no significant differences between the sexes in the DP or PA subscales. We also did not find significant differences in the association of BO levels with marital status, work setting, care setting, private practice or work hours.
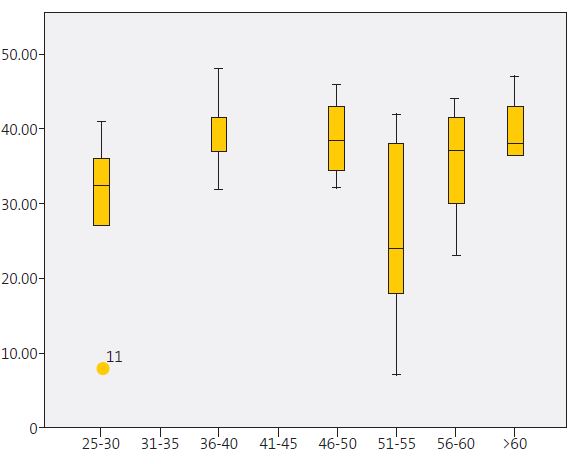
Paediatricians aged 51-55 years were more likely to have low PA compared to all other age groups (Figure 1). On the other hand, the variables associated with higher levels of PA were perceiving work as a vocation (t = 2.299; p = 0.02) rather than a source of income, and perceiving recognition from the organization for the work performed (t = 2.06; p = 0.04).
The perceived opportunity for promotion was inversely and independently associated with EE (t = -2.305; p = 0.026). Other variables associated with higher EE and DP scores were: wanting to change professions (t = 2.5; p = 0.016), having disabling disease (t = 2.14; p = 0.039) or having experienced some form of physical or psychological impairment in recent years (t = 4.18, p <0.0001). When it came to remuneration, participants that perceived remuneration as low had lower PA scores compared to participants that perceived their pay as adequate or high (t = 2.3; p = 0.024).
Table 3 presents the variables significantly associated with every dimension of BO. We ought to highlight that engagement in stress relief activities was significantly associated with a higher level of DP (t = 3.171; p = 0.003).
| Table 3. Variables significantly associated with emotional exhaustion, depersonalization and low personal accomplishment | ||||||
|---|---|---|---|---|---|---|
| Emotional exhaustion | Depersonalization | Low personal accomplishment | ||||
| t | p | t | p | t | p | |
| Unfulfilling work | 10.76 | 0.002 | 2.349 | 0.024 | 2.612 | 0.013 |
| r | p | r | p | r | p | |
| Disenchanted with work | 0.652 | <0.0001 | 0.355 | 0.021 | -0.422 | 0.005 |
| Depression | 0.537 | <0.0001 | 0.381 | 0.013 | -0.569 | <0.0001 |

DISCUSSION
The response rate for the survey was 64%, which is considered high for this type of sample and was equivalent to the participation in the previous study (of 75%). One third of the paediatricians (36%) had scores indicative of BO, a result consistent with other studies,7,8 and greater compared to the 26% reported in 1998 in the same geographical area.34 Although the raw scores in our sample were higher, the difference was not statistically significant. Nevertheless, we must take into account that the prevalence 20 years ago was already high and that it continues to be high, which suggests that BO is a structural problem.
We found a significant association between BO and sex in the EE subscale, in which female paediatricians had higher scores. This was consistent with several previous studies that show that in female physicians, work overload is compounded by the demands of family and housework.35,36
The age interval most strongly associated with BO was 51-55 years, corresponding to the mid-career period, an inflection point that could be interpreted as a paediatrics mid-life crisis. Older participants may have been able to adjust and reduce their strain.
We found a higher increase in BO scores in hospital-based paediatricians, both in the EE and DP subscales, compared to those working in primary care. A possible explanation is that in 1998, adequate working conditions in hospitals were maintained so that BO levels in hospital-based paediatricians were lower, whereas nowadays the work overload also affects hospital settings, which may have resulted in an increase in BO.
Higher levels of BO are associated with a higher prevalence of disabling disease and physical or mental health impairments, in addition to an increased frequency of sick leaves in recent years. It is possible that BO makes physicians more vulnerable to disease or, conversely, that physicians with diseases are more vulnerable to BO. Future studies could explore the direction of this association.
The perception of the medical profession as a calling had a protective effect, as described in previous studies,3,12 with a gradual decline in PA scores associated with the perception of inadequate pay or poor working conditions. The perception of inadequate remuneration was associated with lower PA scores, and therefore with the development of BO. In contrast, the perception of being recognised by the organization was associated with higher PA scores.
Surprisingly, participants that engaged in stress relief activities were more likely to have BO. A possible explanation is that stress relief activities were not pursued preventively, but rather reactively, once clinicians experienced difficulties, in an attempt to alleviate them.
Thus, we have found a high and sustained prevalence of BO over time (one third of paediatricians, in both hospital and primary care settings), which confirms that this is a structural problem.
Thus, it ought to be recognised as such and strategies should be implemented to address it. Individual strategies have exhibited highly variable outcomes, and the interventions used and studied most extensively involve mindfulness, stress management and small support groups.31-33,37,38 Some studies have found that these interventions have a greater impact on the EE and DP dimensions. Strategies combining individual and structural/organizational interventions seem to achieve better outcomes.38
Its persistence through time, high prevalence and known impact on both patient care and health providers themselves make BO a systemic problem as opposed to a personal one. Thus, burnout could be understood as a poor fit between the practice of medicine and the health care system and a loss of autonomy for physicians in the provision of care. Most health care systems have been shifting towards target-oriented management models, with an increasing organizational dehumanization, a high administrative and bureaucratic burden and very high expectations of clinicians.6
In comparing the aviation and health systems, Samra concluded that strategies for addressing BO should include interventions to manage work complexity at the individual, team, and organizational levels.39 This requires a comprehensive approach adaptable to the limitations of both individual providers and the health system to meet the demands of the population. Participation in decision-making and in work structuring have also been identified as important factors in the management of BO.
As Lemaire and Wallace remarked,40 BO is “a system level problem requiring a system level response.” These authors proposed, firstly, tackling all toxic aspects of medical practice that cause and sustain burnout, fostering clinical leadership and a supportive organizational culture. Secondly, that the medical profession and healthcare organizations should view the wellbeing of doctors as integral to professionalism and as central to patient care, as BO has been clearly linked to patient safety concerns and suboptimal patient care. Thirdly, that the wellbeing of doctors should be recognised as a quality indicator for all healthcare systems. Lastly, the authors stated the need for an internationally coordinated research effort to identify evidence-based strategies to reverse the rising tide of burnout globally.
CONCLUSION AND LIMITATIONS OF THE STUDY
The current prevalence of BO in paediatricians practicing in Lleida is 36%, higher compared to 1998 (26%). Scores indicative of job burnout were significantly associated with the perception of clinicians of their work environment, and not with the type of practice, care setting or work hours.
Further research is required to test this hypothesis and develop strategies to improve the current situation.
The possible limitations of the study include selection bias due to the paediatricians that did not participate in the survey, which also entails a risk that the sample may not be representative of all paediatricians in the region. In addition, the sample was obtained from a specific population, which precludes extrapolation of the results to other populations, which would require performance of additional studies.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
BO: burnout · DP: depersonalization and cynicism · EE: emotional exhaustion · MBI: Maslach Burnout Inventory · PA: personal accomplishment.
ACKNOWLEDGMENTS
We thank all the paediatricians that participated in the study.
REFERENCES
- Freudenberger HJ. Staff burnout. J Soc Issues. 1974;30:159-65.
- Maslach C, Jackson SE. Maslach Burn-out Inventory Manual. 2nd edition. Palo Alto, CA: Consulting Psychologist Press; 1986.
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516-29.
- Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15:103-11.
- Leiter MP, Maslach C. Latent burnout profiles: a new approach to understanding the burnout experience. Burn Res. 2016;3:89-100.
- The Lancet. Physician burnout: the need to rehumanise health systems. Lancet. 2019;394:1591.
- Song PP, Walline JH. Physician burnout. Lancet. 2020;395:333.
- Khoo EJ, Aldubai S, Ganasegeran K, Lee BX, Zakaria NA, Tan KK. El agotamiento emocional está asociado con factores estresantes relacionados con el trabajo: estudio multicéntrico y transversal en hospitales públicos de Malasia. Arch Argent Pediatr. 2017;115:212-9.
- Lee RT, Seo B, Hladkyj S, Lovell BL, Schwartzmann L. Correlates of physician burnout across regions and specialities: a meta-analysis. Hum Resour Health. 2013;11:48.
- Yuguero O, Marsal JR, Esquerda M, Soler-González J. Occupational burnout and empathy influence blood pressure control in primary care physicians. BMC Fam Pract. 2017;18:63.
- Yuguero O, Forné C, Esquerda M, Pifarré J, Abadías MJ, Viñas J. Empathy and burnout of emergency professionals of a health region. A cross-sectional study. Medicine (Baltimore). 2017;96:e8030.
- Shanafelt D, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377-85.
- Adsarias R, de Frutos E, Baranda L, Moraga-Llop FA, Enrubia M, Mitjans A. Salut, estils de vida i condicions laborals dels pediatres a Espanya. Pediatr Catalana. 2017;77:9-14.
- Klein J, Grosse Frie K, Blum K, von dem Knesebeck O. Burnout and perceived quality of care among German clinicians in surgery. Int J Qual Health Care. 2010;22:525-30.
- Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017-22.
- Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358-67.
- Tsiga E, Panagopoulou E, Montgomery A. Examining the link between burnout and medical error: a checklist approach. Burn Res. 2017;6:18-29.
- Yuguero O, Marsal JR, Buti M, Esquerda M, Soler-González J. Descriptive study of association between quality of care and empathy and burnout in primary care. BMC Med Ethics. 2017;18:54.
- Baer TE, Feraco AM, Tuysuzoglu Salagowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes towards patients. Pediatrics. 2017;139:e20162163.
- Llera J, Durante E. Correlación entre el clima educacional y el síndrome de desgaste profesional en los programas de residencia de un hospital universitario. Arch Argent Pediatr. 2014;112:e6-11.
- Pantaleoni JL, Augustine EM, Sourkes BM, Bachrach LK. Burnout in pediatric residents over a 2-year period: a longitudinal study. Acad Pediatr. 2014;14:167-72.
- Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93:498-512.
- Wright JG, Khetani N, Stephens D. Burnout among faculty physicians in an academic health science centre. Paediatr Child Health. 2011;16:409-13.
- Navarro-González D, Ayechu-Díaz A, Huarte-Labiano I. Prevalencia del síndrome del burnout y factores asociados a dicho síndrome en los profesionales sanitarios de Atención Primaria. Semergen. 2015;41:191-8.
- Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131-50.
- Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int. 2009;14:204-20.
- Weigl M, Schneider A, Hoffmann F, Angerer P. Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. Eur J Pediatr. 2015;174:1237-46.
- García TT, García PCR, Molon ME, Piva JP, Tasker RC, Branco RG, et al. Prevalence of burnout in pediatric intensivists: an observational comparison with general pediatricians. Pediatr Crit Care Med. 2014;15:e347-53.
- López M, Rodríguez A, Fernández M, Marcos S, Martinón F, Martinón JM. Síndrome de desgaste profesional en el personal asistencial pediátrico. An Pediatr (Barc). 2005;62:248-51.
- Bustinza A, López-Herce J, Carrillo A, Vigil MD, De Lucas García N, Panadero E. Situación de burnout de los pediatras intensivistas españoles. An Pediatr (Barc). 2000;52:418-23.
- West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, et al. Intervention to promote physician well-being, job satisfaction and professionalism: a randomized clinical trial. JAMA Intern Med. 2014:174:527-33.
- Bourbonnais R, Brisson C, Vézina M. Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occup Environ Med. 2011;68:479-86.
- Dyrbye LN, Shanafelt TD, Gill PR, Satele, DV, West CP. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Intern Med. 2019;179:1406-14.
- Esquerda M, Prado S, Solé E, Pifarré J, Gomà AR. La síndrome burn-out (desgast professional) entre els pediatres de Lleida. Pediatr Catalana. 2000;60:12-9.
- Guille C, Frank E, Zhao Z, Kalmbach DA, Nietert PJ, Mata DA, et al. Work-family conflict and the sex difference in depression among training physicians. JAMA Intern Med. 2017;177:1766-72.
- Rabinowitz LG. Recognizing blind spots - A remedy for gender bias in medicine? N Engl J Med. 2018;378:2253-5.
- Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:195-205.
- West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:195-205.
- Samra R. Brief history of burnout. BMJ. 2018;363:k5268.
- Lemaire JB, Wallace JE. Burnout among doctors. BMJ. 2017;358:j3360.