Vol. 23 - Num. 90
Original Papers
Prevalence and characteristics of breastfeeding pain. Prospective multicentric study in Primary Care
Marta Carrera Polancoa, Ana M.ª Lorente García-Mauriñob, Begoña Domínguez Aurrecoecheac, Red de Investigación en Pediatría de Atención Primaria (PAPenRED)
aPediatra. CS Silvano. Madrid. España.
bPediatra. CS Juan de la Cierva. Getafe. Madrid. España.
cPediatra. Red de Investigación en Pediatría de Atención Primaria (PAPenRed). AEPap. España.
Correspondence: M Carrera. E-mail: marta.carrera@salud.madrid.org
Reference of this article: Carrera Polanco M, Lorente García-Mauriño AM, Domínguez Aurrecoechea B, Red de Investigación en Pediatría de Atención Primaria (PAPenRED). Prevalence and characteristics of breastfeeding pain. Prospective multicentric study in Primary Care . Rev Pediatr Aten Primaria. 2021;23:163-73.
Published in Internet: 24-06-2021 - Visits: 17763
Abstract
Introduction: painful breastfeeding (BF) has a very negative impact on the establishment of BF and is one of the main causes of BF cessation, and is therefore considered an important public health problem. Unfortunately, this problem is underestimated by the health care community and few studies have been devoted to its prevalence, characteristics and the attitude of the mothers that experience it.
Sample and methods: the study was conducted in the framework of the Breastfeeding and Child Development study (LAyDI) and focused on BF pain in the first 4 months post birth in a cohort of 203 lactating women managed in primary care centres of the Community of Madrid (Spain).
Results: we found a high incidence of pain in BF women (68.5%), most frequently with onset in the first days post birth, although in 13% of cases it developed after several weeks. In 44% of cases, the pain resolved within 15 days, but in 46% it lasted longer (in 17%, longer than 2 months). We found that 30.9% of mothers contemplated BF cessation at some point due to severe or sustained pain. However, despite having access to professional support, mostly provided by midwives, nearly half of the women who considered weaning did not seek help.
Conclusions: current efforts in different fields of study need to converge urgently to explore the aetiology and pathogenesis of pain and safe and effective approaches to its management in a nonjudgmental and unbiased environment.
Keywords
● Breastfeeding pain ● Dysbiosis ● Milk culture ● Primary care ● Public HealthINTRODUCTION
The benefits that breastfeeding (BF) offers mothers, children, society and the environment are well known worldwide, so BF is considered a key component in public health and not merely a lifestyle choice.1 Notwithstanding, the frequency of early discontinuation of BF is high across the world and depart from the target set by the World Health Organization (WHO) of achieving exclusive breastfeeding (EBF) for the first 6 months of life in 50% of infants at the global level.2
In Spain, nationwide data on the prevalence of BF are obtained through the National Health Survey (Encuesta Nacional de Salud, ENS), although this information is not up to date and is not estimated based on the indicators or methods recommended by the WHO. Based on the most recent data available, from the 2017 survey, the prevalence of EBF was 73.9% at 6 weeks, 63.9% at 3 months and 39% at 6 months post birth.3
The nationwide prospective and multicentre Lactancia Materna y Desarrollo Infantil study (Breastfeeding and Child Development, LAyDI) was designed to study the characteristics of BF in Spain and factors associated with its initiation and duration, among other aspects.4 The study collected data in a cohort of 2066 children born between April 2017 and May 2018 included in the caseloads of 202 primary care paediatricians, selected in proportion to the size of the population of each autonomous community in Spain to ensure that the results would be representative of the entire Spanish population. The study found a prevalence of EBF of 67.23% at 2 weeks post birth and only 39.2% at 6 months post birth, although there was substantial variation between autonomous communities.5
Although it is common to conceive of BF as a pleasant and simple process, the fact is that many mothers experience difficulties that result in frustration and early discontinuation of BF.6 Among them, pain is one of the factors that has the most deleterious impact on the enjoyment of BF and the most frequently reported reason to discontinue BF along with the perception of an insufficient milk supply.7-9
Breastfeeding pain is a challenge for mothers, who often experience feedings as stressful events, undermining their self-esteem and interfering with mother-child bonding.10,11 Despite its relevance, this problem seems to be underestimated by a good part of the health care community, as many studies that analyse the prevalence of BF and the degree of maternal satisfaction do not include or clearly define this variable. On the other hand, the lack of evidence on the severity of BF pain and the characteristics of BF mothers may lead some physicians to question the pain threshold of women that experience persistent pain.11
Primary care is the ideal setting for the direct observation of the experiences and outcomes of mothers in relation to BF and can provide adaptable and accessible support if problems emerge. In this context, the study we present here was conducted in the framework of the LAyDI study and focuses on the analysis of aspects related to pain while BF and the attitude of mothers toward this problem.
PATIENTS AND METHODS
We conducted a prospective, longitudinal, observational and descriptive study with the aim of obtaining detailed information on the characteristics, factors and experiences related to painful BF in a cohort of lactating mothers that visited their assigned primary care centre in the Autonomous Community of Madrid for the first checkup of their babies, born between April 2017 and May 2018.
We named this study Anexo-LAyDI, as it supplemented the information obtained in the LAyDI study, carried out by paediatricians in the Primary Care Paediatrics Research Network (PAPenRed) of the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics, AEPap).4 The study was restricted geographically to the Community of Madrid and focused on the analysis of risk factors associated with painful BF and the attitudes of women in response to this problem. The inclusion criteria for mothers, who were also part of the LAyDI cohort, were determined by the larger nationwide study, and we offered mothers who had given birth in the past 15 days to a healthy infant that was being partially or exclusively breastfeed to participate in the study on a voluntary basis. The exclusion criteria were: preterm birth, multiple birth, length of stay of mother or infant greater than 5 days and severe malformation or disease in the mother or infant.
We collected data through personal interviews conducted by the paediatrician or nurse after participants were informed about the study protocol. Each BF mother included in the study was interviewed within 15 days of childbirth with administration of an anonymised questionnaire that was administered again at 1 month (at least 7 days apart from the initial interview), 2 months and 4 months post birth.
To identify the factors that may be involved in the development of pain, all participants completed the questionnaire developed for the LAyDI study, which includes items with predefined answer choices and items with free-text answers to collect data on the variables presented in Table 1. To complete the information, we asked participants whether they experienced pain during BF beyond what would be considered “mild discomfort in the breast/nipple” at each time point.
| Table 1. Bivariate analysis of risk factors for pain during breastfeeding related to socioeconomic and clinical characteristics, pregnancy, delivery, postpartum and breastfeeding | |||||||
|---|---|---|---|---|---|---|---|
| Variables | BF mothers without pain, n* (%) | BF mothers with pain, n* (%) | OR | 95 CI | p | ||
| Demographic and clinical | Age | <years and >40 years | 19 (30.2%) | 52 (37.4%) | 1.38 | 0.13-2.62 | 0.317 |
| 30-40 years | 44 (69.8%) | 87 (62.6%) | Reference | ||||
| Nationality | Spanish | 49 (76.56%) | 100 (71.94%) | 0.78 | 0.40-1.56 | 0.488 | |
| Other | 15 (23.42%) | 39 (28.05%) | Reference | ||||
| Educational attainment | Primary/secondary | 29 (46.03%) | 49 (35.25%) | 0.64 | 0.35-1.17 | 0.145 | |
| University-level | 34 (53.96%) | 90 (72.58%) | Reference | ||||
| Employment prior to pregnancy | Employed | 52 (82.53%) | 109 (78.41%) | Reference | 0.60-2.80 | 0.499 | |
| Self-employed and other | 11 (17.46%) | 30 (21.58%) | 1.30 | ||||
| Body mass index (BMI) | Overweight/obesity | 20 (33.33%) | 36 (27.69%) | 0.77 | 0.40- 1.98 | 0.428 | |
| Normal weight | 40 (66.67%) | 94 (72.31%) | Reference | ||||
| Pregnancy, childbirth, postpartum and breastfeeding | Parity | Primiparous | 21 (33.3%) | 62 (44.6%) | 1.61 | 0.87-3.00 | 0.132 |
| Multiparous | 42 (66.7%) | 77 (55.4%) | Reference | ||||
| Informed on the benefits of breastfeeding during pregnancy | Yes | 48 (75.0%) | 107 (77.0%) | Reference | 0.45-1.79 | 0.758 | |
| No | 16 (25.0%) | 32 (23.0%) | 0.90 | ||||
| Received practical training on breastfeeding during pregnancy | Yes | 33 (51.6%) | 70 (50.4%) | Reference | 0.58-1.90 | 0.874 | |
| No | 31 (48.4%) | 69 (49.6%) | 1.05 | ||||
| Antibiotherapy during pregnancy and/or delivery | Yes | 20 (31.25%) | 50 (35.98%) | 1.24 | 0.66-2.33 | 0.511 | |
| No | 44 (68.75%) | 89 (64.02%) | Reference | ||||
| Type of delivery | Caesarean | 15 (23.4%) | 24 (17.3%) | 0.68 | 0.33-1.41 | 0.299 | |
| Vaginal | 49 (76.6%) | 115 (82.7%) | Reference | ||||
| Mother-infant separation after birth | Yes | 14 (21.9%) | 31 (22.3%) | 1.03 | 0.50-2.09 | 0.946 | |
| No | 50 (78.1%) | 108 (77.7%) | Reference | ||||
| Time until baby was first put to breast for feeding | <1 hour | 49 (76.56%) | 106 (77.37%) | Reference | |||
| ≥1 hour | 15 (23.44%) | 31 (22.63%) | 0.96 | 0.47-1.93 | 0.890 | ||
| Anatomical nipple problems | Yes | 4 (6.3%) | 15 (10.8%) | 1.81 | 0.58-5.70 | 0.302 | |
| No | 60 (93.8%) | 124 (89.2%) | Reference | ||||
| Use of pacifier/binky in the first 15 days post birth | Yes | 20 (31.3%) | 35 (25.2%) | 0.75 | 0.39-1.45 | 0.398 | |
| No | 44 (68.8%) | 102 (73.4%) | Reference | ||||
| Duration of breastfeeding in previous children | 0-3 months | 9 (22.5%) | 19 (25.7%) | 1.19 | 0.48-2.95 | 0.707 | |
| More than 3 months | 31 (77.5%) | 55 (74.3%) | Reference | ||||
| Weaning/mixed feeding in previous children due to painful breastfeeding | Yes | 1 (2.6%) | 6 (8.2%) | 3.40 | 0.39-29.34 | 0.239 | |
| No | 38 (97.4%) | 67 (91.8%) | Reference | ||||

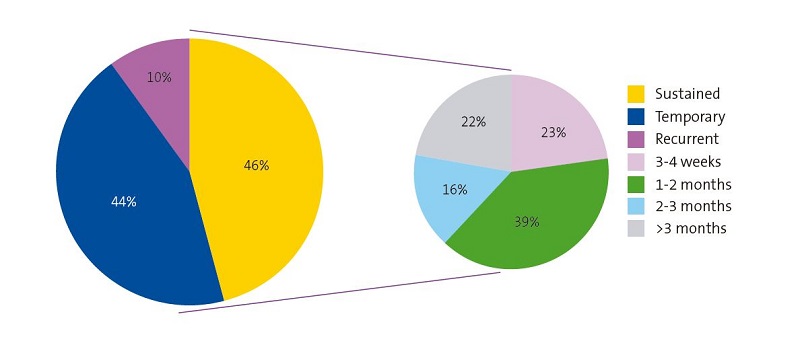
For mothers that reported pain, we included questions about their particular experience (location of pain, whether they contemplated weaning, duration of pain, whether they sought support to manage the pain, etc.). When it came to the duration of pain, we considered it “temporary” if it resolved within 2 weeks, “sustained” if it persisted for more than 2 weeks, and “recurrent” if pain was reported again in a non-consecutive visit.
Statistical analysis
We described the potential risk factors for BF pain as categorical variables. To assess the association between the presence of pain during BF and each risk factor, we compared the values of each of these categorical variables in cases and controls using the χ2 test. To compare exposure to each of these variables in the 2 groups of women, we calculated the odds ratio (OR) with the corresponding 95% confidence interval (95 CI) for each risk factor, considering the association significant for tests with a p-value of less than 0.05.
Ethical considerations
The LAyDI study was approved by the Research Ethics Committee of the Principality of Asturias (file no. 213/16) on December 29, 2016.
RESULTS
A total of 24 primary care paediatricians employed in different health districts in the Community of Madrid collected data for 203 mother-infant dyads. The initial sample included 215 women, but 12 dyads were lost to followup due to changes in address.
Most women (68.5%; n = 139) experienced pain associated with BF at some point in the first 4 months post birth. Of the mothers that experienced pain, 82.01% (n = 114) reported pain in both breasts.
A breast milk culture was only ordered in 5 of the 139 cases of BF pain, and was positive in all, leading to diagnosis of mastitis based on the criteria proposed by the Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (Spanish Society of Infectious Diseases and Clinical Microbiology, SEIMC).12 However, 11.3% (n = 23) of participants received a diagnosis of mastitis by health care professionals based on heterogeneous criteria that did not fit the SEIMC guidelines. There was a single case of breast abscess.
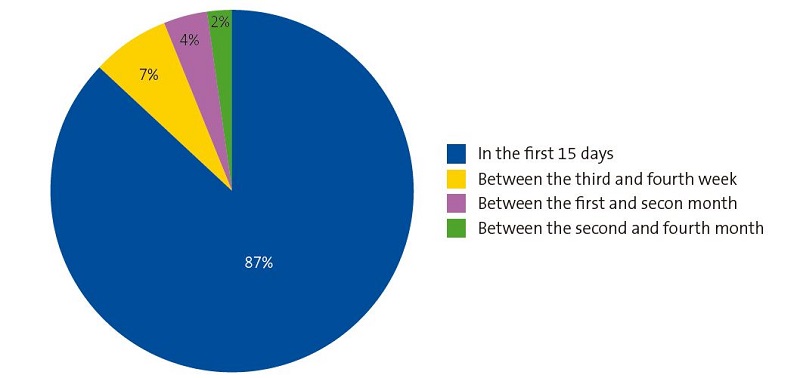
As can be seen in Figure 1, most participants (87%; n = 121) developed pain in the first 15 days of BF, but 13% (n = 18) started experiencing pain after a few weeks and a few mothers after having breastfeed for 2 months (2.2%; n = 3).
Figure 2 represents the duration of pain, showing that 44% (n = 61) of cases resolved for good in the first 15 days, but in 10% (n = 14) of cases, pain recurred at a later time point. We ought to highlight that pain persisted in approximately half of mothers that experienced pain (46%; n = 64), even lasting longer than 2 months in 17 cases, which amounted to 17.3% of all mothers that experienced pain with BF.
When it came to the attitude of mothers in response to pain, many participants, despite the negative impact of pain during BF, only acknowledged feeling pain when directly asked about it. Barely 45% (n = 63) of mothers that reported pain during BF took the initiative of seeking support; the rest believed that they did not need it and that “pain would probably go away on its own”.
For 30.9% (n = 43) of women that experienced pain, the pain was so intense or persistent that they considered discontinuing BF at some point, in spite of which only 26 of them sought help (60.5%).
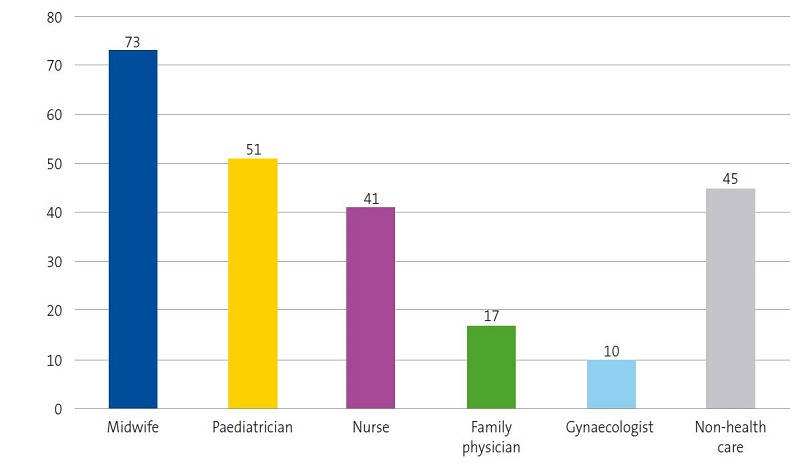
The midwife was the health care worker to whom mothers reached out most frequently to seek support, with family physicians and gynaecologists being by far the least frequently involved in BF problems, as can be seen in Figure 3.
At the end of the 4-month followup, only 64.04% (n = 130) of participants was practicing EBF and, of these mothers, 23.8% (n = 31) had experienced sustained pain lasting more than 1 month. Only 12.3% (n = 16) of mothers that maintained EBF at 4 months reported not having experienced pain at any point during the followup.
During the followup, 22.2% (n = 45) of participants stopped BF for a variety of reasons. Of these mothers, 29 (64.4%) reported experiencing pain at some point during the followup, which was categorised as sustained in 33.3% (n = 15) of these cases.
Bivariate analysis of risk factors for pain during breastfeeding and breastfeeding cessation
Table 1 presents the results of the bivariate analysis of the qualitative variables (risk factors) potentially associated with pain during BF.
Contrary to the findings of other studies,9,13-15 none of the factors under investigation was significantly associated with the development of pain on BF.
However, when the analysed the association between the same qualitative variables and BF cessation, we found significant associations with maternal age (<30 or >40 years), the use of a pacifier/binky in the first 15 days post birth and, notably, with a previous history of BF cessation before 3 months post birth, as can be seen in Table 2. Interestingly, the pain experienced by participants in association with BF during the followup was not associated with an increased current risk of BF cessation.
| Table 2. Bivariate analysis of risk factors for BF cessation before 4 months post birth related to socioeconomic and clinical characteristics, pregnancy, delivery, postpartum and breastfeeding | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Breastfeeding at 4 months (mixed or exclusive) n* (%) | Weaning before 4 months post partum, n* (%) | OR | 95 IC | p | ||
| Demographic and clinical | Age | <years and >40 years | 48 (30.57%) | 23 (51.11%) | 2.37 | 1.21-4.67 | 0.011 |
| 30-40 years | 109 (69.43%) | 22 (48.89%) | Reference | ||||
| Nationality | Spanish | 114 (72.15%) | 35 (77.78%) | 1.35 | 0.62-2.96 | 0.451 | |
| Other | 44 (27.85%) | 10 (22.22%) | Reference | ||||
| Educational attainment | Primary/secondary | 56 (35.67%) | 22 (48.89%) | 1.73 | 0.88-3.37 | 0.108 | |
| University-level | 101 (64.33%) | 23 (51.11%) | Reference | ||||
| Employment prior to pregnancy | Employed | 126 (80.25%) | 35 (77.78%) | Reference | |||
| Self-employed and other | 31 (19.75%) | 10 (22.22%) | 1.16 | 0.52-2.60 | 0.71 | ||
| Body mass index (BMI) | Overweight/obesity | 44 (29.14%) | 12 (30.77%) | 1.08 | 0.50-2.32 | 0.84 | |
| Normal weight | 107 (70.86%) | 27 (69.23%) | Reference | ||||
| Pregnancy, childbirth, postpartum and breastfeeding | Parity | Primiparous | 69 (43.95%) | 14 (31.11%) | 0.58 | 0.28-1.17 | 0.12 |
| Multiparous | 88 (56.05%) | 31 (68.89%) | Reference | ||||
| Informed on the benefits of breastfeeding during pregnancy | Yes | 121 (76.58%) | 34 (75.56%) | Reference | |||
| No | 37 (23.42%) | 11 (24.44%) | 1.06 | 0.49-2.29 | 0.886 | ||
| Received practical training on breastfeeding during pregnancy | Yes | 83 (52.53%) | 20 (44.44%) | Reference | |||
| No | 75 (47.47%) | 25 (55.56%) | 1.38 | 0.71-2.89 | 0.338 | ||
| Antibiotherapy during pregnancy and/or delivery | Yes | 65 (41.14%) | 22 (48.89%) | 1.37 | 0.70-2.60 | 0.35 | |
| No | 93 (58.86%) | 23 (51.11%) | Reference | ||||
| Type of delivery | Caesarean | 28 (17.72%) | 11 (24.44%) | 1.50 | 0.68-3.32 | 0.31 | |
| Vaginal | 130 (82.28%) | 34 (75.56%) | Reference | ||||
| Mother-infant separation after birth | Yes | 39 (24.68%) | 6 (13.33%) | 0.47 | 0.18-1.14 | 0.10 | |
| No | 119 (75.32%) | 39 (86.87%) | Reference | ||||
| Time until baby was first put to breast for feeding | <1 hour | 125 (79.11%) | 30 (69.77%) | Reference | |||
| ≥1 hour | 33 (20.89%) | 13 (30.23%) | 1.64 | 0.77-3.49 | 0.19 | ||
| Anatomical nipple problems | Yes | 12 (7.59%) | 7 (15.56%) | 2.24 | 0.83-6.08 | 0.1 | |
| No | 146 (92.41%) | 38 (84.44%) | Reference | ||||
| Use of pacifier/binky in the first 15 days post birth | Yes | 32 (20.51%) | 23 (51.11%) | 4.05 | 2.01-8.17 | <0.0001 | |
| No | 124 (79.49%) | 22 (48.89%) | Reference | ||||
| Duration of breastfeeding in previous children | 0-3 months | 7 (8.33%) | 21 (70.0%) | 25.67 | 8.55-77.05 | <0.0001 | |
| More than 3 months | 77 (91.67%) | 9 (30.0%) | Reference | ||||
| Pain during breastfeeding | Yes | 110 (69.62%) | 29 (64.44%) | 0.79 | 0.34-1.59 | 0.59 | |
| No | 48 (30.38%) | 16 (35.56%) | Reference | ||||

DISCUSSION
In the primary care setting, painful BF is a frequent issue for women, who face the dilemma whether to continue BF or give up.
The high percentage of women that reported pain on BF in our study (68.5%) was similar to the percentage found by a prospective study conducted at the primary care level that analysed this experience in detail.15. Other studies have found even higher frequencies,16,17 which shows that pain is a frequent problem and most likely underdiagnosed.
The evidence on painful BF is consistent in its development, most frequently, in the first 15 days post birth,15,16,18 as was the case in our study. However, we ought to highlight that 13% of participants first felt pain after several weeks of having none, of which 6% developed pain after 1 month of painless BF, a slightly smaller proportion compared to the 9.7% observed in another prospective study.15 There are barriers to comparing these findings to those of other studies on painful BF, as the followup does not usually extend past the first 2 weeks post birth.
Nevertheless, the substantial proportion of women that experience sustained pain on BF is alarming. Based on various studies, between 17% and 29% of BF mothers suffer pain consistently for 2 or more months,15,16 which was corroborated by our data (17.3%).
Pain on BF can be intense and cause significant anxiety in many cases.8 Previous evidence suggests that it may be more intense in the early stages of BF11,18 and gradually subside in a few days,16,19 although nearly 10% of women may continue to suffer intense pain (scores > 7 in the visual analogue scale) at 1 month of BF.15 In our study, we found that nearly one third of participants considered BF cessation due to the intensity or duration of the pain. Still, it is worth mentioning that women that had experienced pain with BF for more than 1 month were more likely to maintain EBF at 4 months compared to mothers that had not experienced pain.
We also ought to highlight that despite access to professional support, nearly half of women that considering cessation of BF did not seek help. This attitude may be heavily influenced by the widely accepted belief in society that suffering and self-denial are intrinsic to being a good mother.20 Studying the reasons that lead mothers to behave this way would be relevant in order to identify the most effective way to help. On the other hand, it is important to remember that women do not always seek support to maintain BF, but may also need support to be able to discontinue BF without feeling guilty due to social pressure.21
Based on the results of our study, midwives are the providers that manage most consultations regarding pain in BF, followed, with a substantially smaller frequency, by paediatricians and nurses. Since early BF cessation is a public health matter, it is crucial that every health professional involved in the care of mothers have up-to-date knowledge of BF, in addition to establishing an environment conducive for mothers to voice their questions and concerns to be able to provide effective support should barriers to BF emerge. A first step towards this goal would be to generate interest in future clinicians by including BF as a subject in the medical school curriculum.
It is important to know that there is no widely accepted and effective approach to the management of pain in BF,18 but there is strong evidence on the low efficacy of help offered once pain has already developed.22 Barely half of affected mothers succeeds in resolving persistent pain on BF, despite their motivation and the support received,19 and therefore the priority should be to make a concerted effort to thoroughly research the aetiology and pathogenesis of pain to be able to identify effective solutions, achieve higher rates of EBF and ensure that women can experience BF and reap all the benefits without associated stress.
It has been generally believed that poor BF technique is the main cause of BF pain,7 despite the lack of conclusive evidence in support of this hypothesis,15,19,23 as this factor has not been widely studied in dyads that enjoy a positive BF experience. On one hand, there are mothers that breastfeed without problems despite the use of what could be considered poor technique, and on the other there are mothers that experience pain in spite of adequate dyad positioning and latching.11,22,24 While in some cases painful BF may be managed successfully with changes in maternal positioning and infant latching, the poor technique hypothesis does not explain cases with onset following several weeks of uncomplicated BF or of recurrent pain.
Another aspect that has been subject to extensive debate is the role of certain anatomical characteristics of maternal nipples of infant mouths in the development of pain, especially ankyloglossia, but the existing evidence in support of this factor is insufficient.25,26 Nevertheless, routine assessment of anatomical features is important, as they could exacerbate other problems and affect the severity of pain.
In the past decade, numerous scientific publications have provided robust evidence on imbalances in the human milk microbiota as the main cause of painful BF.15,27-29 In fact, since the SEIMC published their clinical microbiology guideline for diagnosis of bacterial infections associated with childbirth and the postpartum period (“Diagnóstico microbiológico de la infección bacteriana asociada al parto y puerperio”),12 human milk culture has been widely introduced in clinical microbiology laboratories, and many primary care centres in the Community of Madrid have had the option of officially requesting these cultures from the 15 referral hospitals in the region since 2013, but orders are still few and far between, as can be gleaned from the results of our study. Paradoxically, the clinical practice guideline on BF published by the Ministry of Health of Spain in 2017 all but restricts the ordering of human milk cultures to cases with suspected or high risk of resistance to broad-spectrum antibiotics,30 despite the lack of evidence supporting the effectiveness of empiric antibiotherapy,31 whereas milk cultures should be performed routinely along with antimicrobial susceptibility testing in every case of painful BF, as recommended by the SEIMC.12 As declared by the WHO, the increase in the prevalence of drug-resistant bacteria caused by the irrational use of antibiotics is one of the main global health problems.32 This has motivated a growing interest in recent years in bacterial therapy, an approach that uses commensal or probiotic bacteria to prevent or treat colonization of the host by pathogenic microorganisms. This approach is based on the principle of competitive exclusion by which certain nonpathogenic bacteria overcome pathogenic bacteria when both are competing to inhabit the same niche. The use of specific probiotics to modulate imbalances in the bacterial population of the mammary gland is a promising strategy, as suggested by the results from a few studies,33-36 and it would be useful to establish their effectiveness through the development of well-designed trials.
CONCLUSION
Pain on BF is a much more frequent phenomenon than it would be expected based on the literature on the prevalence of BF, and in some cases, it is underestimated by women themselves.
All health care professionals engaged in the care of breastfeeding women need to become more involved in detecting pain in BF and capable of addressing it effectively, avoiding the use of antibiotics and being particularly mindful of women that had previous negative experiences with BF and women BF for the first time.
Current efforts in different fields of study need to converge urgently to explore safe and effective alternatives, such as bacterial therapy, to prevent and treat BF pain and therefore avoid unwanted early BF cessation and contribute to a greater duration of BF.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
AEPap: Asociación de Pediatría de Atención Primaria · BF: breastfeeding · EBF: exclusive breastfeeding · ENS: National Health Survey of Spain · LAyDI: estudio Lactancia Materna y Desarrollo Infantil · OR: odds ratio · PAPenRed: Primary Care Paediatrics Research Network · SEIMC: Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica · WHO: World Health Organization · 95 CI: 95% confidence interval.
LIST OF PAEDIATRICIANS THAT COLLABORATED IN THE RESEARCH
Elia Acitores Suz, Celina Arana Cañedo-Argüelles, María Isabel Astiz Blanco, Dora Bejarano López, María Rosario Benítez Rubio, Juan Manuel Bombín Granado, Belén Botella Serrano, María Laura Casado Sánchez, Mar Duelo Marcos, María Jesús Escribano Romero, Óscar Espinazo Ramos, Blanca Espínola Docio, Carmen A. García Rebollar, Macarena García Santiago, Paloma Hernando Helguero, Blanca Juanes de Toledo, Guillermo Martín Carballo, Victoria Martínez Rubio, Carmen Mustieles Moreno, Consuelo Rey del Castillo, Esther Ruiz Chércoles, Isabel Sánchez-Prieto Emmanuel and Olga Velasco Guijarro.
REFERENCES
- Bagci Bosi AT, Eriksen KG, Sobko T, Wijnhoven TM, Breda J. Breastfeeding practices and policies in WHO European Region Member States. Public Health Nutr. 2016;19:753-64.
- Metas mundiales de nutrición 2025: documento normativo sobre lactancia materna 2017 (WHO/NMH/NHD/14.7). In: World Health Organization [online] [accessed 14/06/2021]. Available at www.who.int/nutrition/publications/globaltargets2025_policybrief_breastfeeding/es
- ENSE Encuesta Nacional de Salud España 2017; 2018. In: Ministerio de Sanidad, Consumo y Bienestar Social [online] [accessed 14/06/2021]. Available at www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_pres_web.pdf
- Lactancia Materna y Desarrollo Infantil. Influencia de factores socioeconómicos, culturales e individuales en el inicio y en la duración de la lactancia materna ESTUDIO LAYDI. Asociación Española de Pediatría en Atención Primaria (AEPap) [online] [accessed 14/06/2021]. Available at www.aepap.org/sites/default/files/noticia/archivos-adjuntos/memoria_estudio_laydi_reducida.pdf
- García Vera C, Viar Urieta M, Fernández León A, Surribas Murillo C, del Toro Calero C, Rodríguez-López Márquez GA, et al. Prevalencia global y por comunidades autónomas de los distintos tipos de lactancia durante el primer año de vida, a partir del seguimiento de una cohorte de 2066 niños. Rev Pediatr Aten Primaria Supl. 2020;22:20-1.
- Wall G. Moral constructions of motherhood in breastfeeding discourse. Gender & Society 2001;15:592-610.
- Amir LH. Managing common breastfeeding problems in the community. BMJ. 2014;348:g2954.
- Jackson KT, O’Keefe-McCarthy S, Mantler T. Moving toward a better understanding of the experience and measurement of breastfeeding-related pain. J Psychosom Obstet Gynaecol. 2019;40:318-25.
- Cabedo R, Manresa JM, Cambredó MV, Montero L, Reyes A, Gol R, et al. Tipos de lactancia materna y factores que influyen en su abandono hasta los 6 meses. Estudio LACTEM. Matronas Prof. 2019;20:54-61.
- Amir LH, Dennerstein L, Garland SM, Fisher J, Farish SJ. Psychological aspects of nipple pain in lactating women. J Psychosom Obstet Gynecol. 1996;17:53-8.
- McClellan HL, Hepworth AR, Garbin CP, Rowan MK, Deacon J, Hartmann PE, et al. Nipple pain during breastfeeding with or without visible trauma. J Hum Lact. 2012;28:511-21.
- Delgado S, García-Garrote F, Padilla B, Rodríguez Gómez JM, Romero B. Diagnóstico microbiológico de la infección bacteriana asociada al parto y al puerperio. In: Cercenado Mansilla E, Cantón Moreno R, eds. Procedimientos en microbiología clínica, n.º 54. In: Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC) [online] [accessed 14/06/2021]. Available at www.seimc.org/contenidos/documentoscientificos/procedimientosmicrobiologia/seimc-procedimientomicrobiologia54.pdf
- Mediano P, Fernández L, Rodríguez JM, Marín M. Case-control study of risk factors for infectious mastitis in Spanish breastfeeding women. BMC Pregnancy Childbirth. 2014;14:195.
- Ramiro González MD, Ortiz Marrón H, Arana Cañedo-Argüelles C, Esparza Olcina MJ, Cortés Rico O, Terol Claramonte M, et al. Prevalencia de la lactancia materna y factores asociados con el inicio y la duración de la lactancia materna exclusiva en la Comunidad de Madrid entre los participantes en el estudio ELOIN. An Pediatr (Barc). 2018;89:32-43.
- Marín M, Villanueva I, Domínguez A, Carrera M. Incidencia y factores de riesgo del dolor durante la lactancia: estudio prospectivo en una consulta de Pediatría en Atención Primaria. Acta Pediatr Esp. 2019;77:e158-1e68.
- Buck ML, Amir LH, Cullinane M, Donath SM. Nipple pain, damage, and vasospasm in the first 8 weeks postpartum. Breastfeed Med. 2014;9:56-62.
- Jiménez-Gómez MI, Meneses-Monroy A, Corrillero-Martín J, Santana-Gutiérrez S, Rodríguez-Martín R, Girón-Daviña PR. Prevalence of nipple soreness at 48 hours postpartum. Breastfeed Med. 2021 [in press].
- Dennis CL, Jackson K, Watson J. Interventions for treating painful nipples among breastfeeding women. Cochrane Database Syst Rev. 2014;15:CD007366.
- Kent JC, Ashton E, Hardwick CM, Rowan MK, Chia ES, Fairclough KA, et al. Nipple pain in breastfeeding mothers: incidence, causes and treatments. Int J Environ Res Public Health. 2015;12:12247-63.
- Martínez-Plascencia U, Rangel-Flores YY, Rodríguez-Martínez ME. ¿Lactancia materna o en pareja? Un estudio sobre las experiencias de reconfiguración de cuerpos, roles y cotidianeidades en madres y padres mexicanos. Cad Saúde Pública. 2017;33:e00109616.
- Díez-Sampedro A, Flowers M, Olenick M, Maltseva T, Valdés G. Women’s choice regarding breastfeeding and its effect on well-being. Nurs Womens Health. 2019;23:383-9.
- Abordaje de las dificultades más frecuentes en lactancia materna; 2016. In: Federación de Asociaciones de Matronas de España (FAME) [online] [accessed 14/06/2021]. Available at www.federacion-matronas.org/wp-content/uploads/2016/06/lactancia-materna-2-6-16.pdf
- Blair A, Cadwell K, Turner-Maffei C, Brimdyr K. The relationship between positioning, the breastfeeding dynamic, the latching process and pain in breastfeeding mothers with sore nipples. Breastfeed Rev. 2003;11:5-10.
- Bourdillon K, McCausland T, Jones S. Latch-related nipple pain in breastfeeding women: the impact on breastfeeding outcomes. Br J Midwifery, 2020;28:406-14.
- O’Shea JE, Foster JP, O’Donnell CP, Breathnach D, Jacobs SE, Todd DA, et al. Frenotomy for tongue-tie in newborn infants. Cochrane Database Syst Rev. 2017;3:CD011065.
- Bin-Nun A, Kasirer YM, Mimouni FB. A dramatic increase in tongue tie-related articles: a 67 years systematic review. Breastfeed Med. 2017;12:410-4.
- Mediano P, Fernández L, Jiménez E, Arroyo R, Espinosa-Martos I, Rodríguez JM, et al. Microbial diversity in milk of women with mastitis: potential role of coagulase-negative staphylococci, viridans group streptococci, and corynebacteria. J Hum Lact. 2017;33:309-18.
- Rodríguez JM, Fernández L. Infectious mastitis during lactation: a mammary dysbiosis model. In: Prebiotics and probiotics in human milk. San Diego: Academic Press, 2017. p. 401-28.
- Angelopoulou A, Field D, Ryan CA, Stanton C, Hill C, Ross RP. The microbiology and treatment of human mastitis. Med Microbiol Immunol. 2018;207:83-94.
- Guía de Práctica Clínica sobre lactancia materna. Ministerio de Sanidad, Servicios Sociales e Igualdad; Agencia de Evaluación de Tecnologías Sanitarias del País Vasco-OSTEBA; 2017. In: Grupo de trabajo de la Guía de Práctica Clínica sobre lactancia materna [online] [accessed 14/06/2021]. Available at www.aeped.es/sites/default/files/guia_de_lactancia_materna.pdf
- Jahanfar S, Ng CJ, Teng CL. Antibiotics for mastitis in breastfeeding women. Cochrane Database Syst Rev. 2013;2:CD005458.
- Antimicrobial resistance. Fact sheet, October 13, 2020. In: World Health Organization [online] [accessed 15/4/2021]. Available at www.who.int/es/news-room/fact-sheets/detail/antimicrobial-resistance
- Fernández L, Arroyo R, Espinosa I, Marín M, Jiménez E, Rodríguez JM. Probiotics for human lactational mastitis. Benef Microbes. 2014;5:169-83.
- Maldonado-Lobón JA, Díaz-López MA, Carputo R, Duarte P, DíazRopero MP, Valero AD, et al. Lactobacillus fermentum CECT 5716 reduces staphylococcus load in the breastmilk of lactating mothers suffering breast pain: a randomized controlled trial. Breastfeed Med. 2015;10:425‑32.
- Hurtado JA, Maldonado Lobón JA, Díaz Ropero MP, Flores Rojas K, Uberos J, Leante JL, et al. Oral administration to nursing women of Lactobacillus fermentum CECT 5716 prevents lactational mastitis development: a randomized controlled trial. Breastfeed Med. 2017;12:202-9.
- Barker M, Adelson P, Peters MDJ, Steen M. Probiotics and human lactational mastitis: A scoping review. Women Birth. 2020;33:e483-91.