Vol. 23 - Num. 90
Original Papers
Plans for the prevention of noncommunicable chronic diseases in children and adolescents
Beatriz Flores Oteroa, Jesús Aceituno Duqueb
aFisioterapeuta. Colegio de Educación Especial ATEMPACE. Madrid . España.
bCiencias de la Actividad Física y el Deporte. Facultad de Formación del Profesorado. Universidad Autónoma de Madrid. Madrid. España.
Correspondence: J Aceituno . E-mail: jesus.aceituno@uam.es
Reference of this article: Flores Otero B, Aceituno Duque J. Plans for the prevention of noncommunicable chronic diseases in children and adolescents. Rev Pediatr Aten Primaria. 2021;23:143-53.
Published in Internet: 18-06-2021 - Visits: 20497
Abstract
Introduction: plans for the prevention of noncommunicable diseases in children and adolescents constitute an important area in the health care research field.
Material and methods: we conducted a systematic review of evidence obtained from major databases such as PubMed, WoS and the Cochrane Library. Many studies have analysed the design, implementation and outcomes of strategies in different segments of the population.
Results: the review of the literature showed that most studies were developed by the public health system and related to or implemented through the public school system. We analysed 11 systematic reviews, of which 5 focused on diet and nutrition and 3 on overweight, obesity and physical activity, which were the most frequently topics.
Discussion: the detailed analysis of the literature on this subject revealed commonalities in the studies in terms of the implementation of the preventive strategies, the analysis of outcomes and the duration of the interventions. Further efforts must be devoted by government authorities to the design and implementation of multidisciplinary prevention strategies.
Keywords
● Adolescents ● Children ● Non-communicable diseases ● PreventionINTRODUCTION
Health is a state of adequate adaptation, growth and development, and disease the loss of this adaptation or else a crisis of the human organism in the attempt to maintain an adaptive equilibrium. The development of health promotion is a key step in the construction of a human and healthy world,1 involving, on one hand, the promotion of healthy lifestyles and, on the other, the reduction of factors leading to disease.2 The World Health Organization (WHO) considers that the involvement and commitment of communities is essential for the development of their health and that delivery of community- and family-centred primary care is one of the key strategies to achieve these objectives.3
According to the WHO, noncommunicable diseases (NCDs) are responsible for 71% of deaths globally each year, killing approximately 41 million people as of 2018, a percentage that increased to 85% of the total deaths in low- and middle-income countries in 2020. The subject of this report is also of vital importance, as NCDs largely affect individuals aged less than 60 years.4 In this fact file, the WHO concludes that the elimination of the main modifiable risk factors would allow the prevention of most NCDs, including cardiovascular diseases,5 strokes, 40% of cancers,6 type 2 diabetes7 and overweight and obesity.8 At the same time, the prevalence of overweight and obesity is increasing worldwide, a phenomenon with an important impact on the health of the population and health care expenditure.9
Traditionally, programmes for the prevention of chronic diseases were developed and implemented by health care institutions or government agencies. For example, there are programmes with a high impact at the global level, such as the Healthy Babies, Healthy Children programme in Ontario, Canada (2018), Action Group B3 Action Plan (2017), a programme for the prevention of chronic respiratory diseases at the European level, the Sport-2-Stay-Fit Study (2015), focused on the treatment of children with chronic diseases, or the Global Forum on Chronic Disease Prevention and Control of the WHO, a plan to ensure the continuity of strategies for the prevention of chronic diseases at the global level.
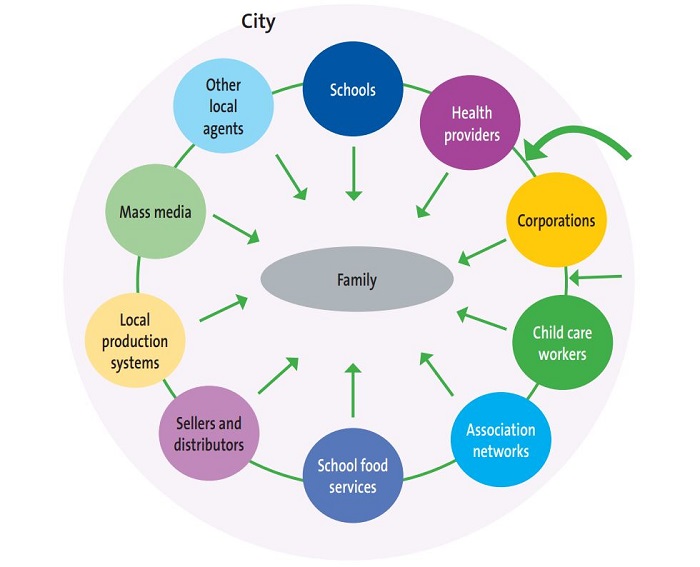
When it comes to the public health system in Spain, there is the THAO programme, an initiative for the promotion of healthy nutrition and the prevention of obesity with participation of 3 autonomous communities (Andalusia, Community of Madrid and Catalonia). This programme aims to promote changes through different institutions (schools, businesses, corporations, health care organizations, etc) in the lifestyles of children and families by means of school-based educational interventions and the organization of sports events and healthy cooking workshops. The THAO programme is yet another example of the broad range of tools available to society to pursue relevant behavioural changes in children and families.10 Figure 1 presents an example of the agents of behavioural change defined by THAO.
The family as an agent of prevention
Thus, aside from the attitudes found in government administration, health care and educational institutions, we believe that the attitude and behaviour of families in response to a chronic condition in a family member, whether congenital or acquired, is crucial to the wellbeing and quality of life of the individual living with the disease.11 Other studies have analysed attitudes and behaviours related to diet and physical activity and the perception of the risk of developing diseases. Thus, assessing the risk involved in the family history of disease may motivate families to adopt health promotion strategies.12
Society as an agent of prevention
The global supply of low-cost, energy-rich products has increased in the past 4 decades, contributing to the increase in obesity in the United States, which has reached a prevalence of 35% in adults and 17% in children. When it comes to Spain, the WHO estimates that 14.9% of children are overweight or obese.
In low-resource communities, fresh, unprocessed foods are often expensive or of poor quality. One study analysed the correlation between the prevalence of childhood obesity and the frequency of visits to grocery stores and other food sources in one such community.13 Some of these studies may not seem quite feasible from a social perspective, but the interventions in the framework of the B’More Healthy Communities for Kids14,15 were very well designed, and the authors gathered information on purchases, doses delivered and fidelity of children to these businesses. Participants received guidance and information regarding alternative food choices, low-sugar and low-sodium drinks and even the serving sizes recommended for children. The outcomes of this intervention demonstrated that it is possible to influence nutrition in children in a direct and relatively inexpensive manner through local policy and campaigns to promote healthy foods by providing discounts and informational brochures, among other strategies. There are other interesting programmes that use innovative approaches, such as a project that seeks to promote emotional wellbeing through virtual reality.17-23
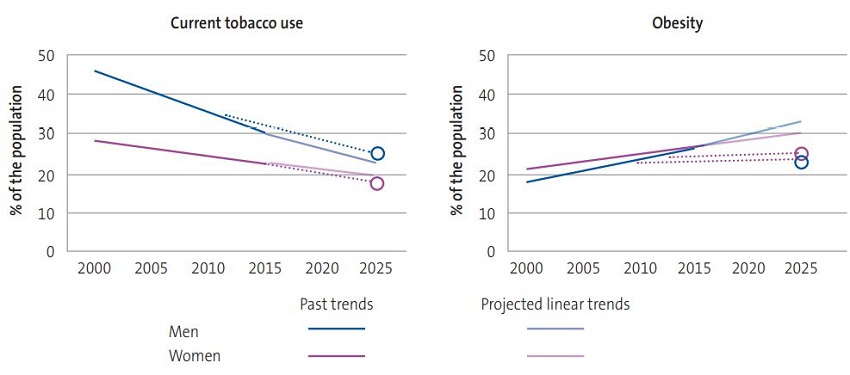
Numerous works have addressed the prevention of NCDs in the general population,23,24 a matter of international importance.8 Table 1 lists the risk factors identified by the WHO.25 These research projects illustrate the current interest in the reduction of specific social risk factors, including tobacco use and the prevalence of overweight and obesity (Figure 2).
| Table 1. Risk factors for noncommunicable diseases25 |
|---|
| 1. Harmful use of alcohol |
| 2. Physical inactivity |
| 3. Excess salt/sodium intake |
| 4. Tobacco use |
| 5. Elevated blood pressure |
| 6. Diabetes |
| 7. Obesity |
| 8. Outdoor air pollution |
| 9. Indoor air pollution |

The aim of our review was to describe from a critical and practical perspective the strategies that have proven effective at the national and international levels that could serve as the foundation to develop a national plan to address NCDs in children and adolescents.
MATERIAL AND METHODS
We performed a literature search between May and July of 2019. We used databases in the health field, including Medline, PubMed, Web of Science (WoS) and the Cochrane Library of systematic reviews. We used the following search queries: “health promotion chronic disease AND children” and “health promotion chronic disease programme”. We selected the full text criterion for both searches. We used the UNESCO Thesaurus to select the terms. We used different terms to identify publications related to the subject of interest: strategy, policies, preventive.
Inclusion and exclusion criteria
We included articles published between January 2014 and June 2019 on the prevention of noncommunicable chronic diseases in children and adolescents.
We applied the classification published by Cerdá et al26 to present the works of highest scientific calibre (Table 2). For the purpose of our project, we selected review articles in high-impact journals that met the aforementioned inclusion criteria.
| Table 2. Levels of evidence26 | |
|---|---|
| Level I |
|
| Level II |
|
| Level III | All other controlled studies in a representative sample in which the outcomes are independent of the intervention performed on participants |
| Level IV | Studies without a control group, case series, case report or expert opinion |

We excluded articles that did not meet the inclusion criteria: studies on communicable or acute diseases, studies focused on the adult or geriatric population. We also excluded editorials, experimental studies, videos and books.
Analysis of the literature review
We analysed the selected articles based on the following variables and the criteria specified above: article characteristics (year of publication, journal, field, research institution, number of studies included in the review), population (group of individuals included in the analysis), organization that sponsored the research (dichotomous variable: educational institution or health care institution); location (countries where the studies took place); subject (diet/nutrition; alcohol, drugs and other substances; violence; hygiene; oral health; cancer; overweight, obesity and physical activity; mental health; respiratory diseases; cardiovascular diseases).
We did not analyse the quantitative data of the studies included in the review.
RESULTS
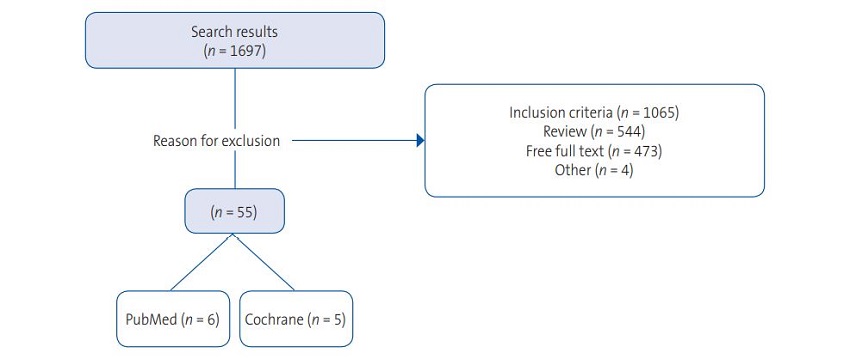
The initial search yielded 1697 works, of which we considered 55 systematic reviews. Out of this total, we selected 11 reviews, excluding the others for failing to meet the established inclusion criteria (Figure 3). In the sample of selected articles, the most frequent subject was diet/nutrition, addressed in 5 articles (45.4%),27-33 followed by the intimately related subject of overweight, obesity and physical activity, addressed in 3 articles (27.7%).9,30,33 Two articles each were devoted to the subjects of alcohol, drugs and other substances and of oral health (18.1%).30,33-35 Lastly, we identified 2 articles devoted to cardiovascular diseases and cancer (9% each).32,33 All the selected articles were written in English.
Most of the research was conducted in universities. We also found articles produced by national associations of specific diseases, like the study conducted by Steinberger et al. in 201627 for the American Heart Association (AHA).
When it came to the institution that sponsored the selected studies, 9 of the total 11 were performed in the context of programmes implemented through the health care system. In 2 instances,28,29 the studies were carried out by Spanish government agencies. Only 1 review30 involved the mixed participation of the public health and education systems. Lastly, most of the reviews analysed experimental studies performed in the United States (72.7%), followed by studies conducted in the United Kingdom (27.2%), with only 1 study each conducted in Chile, South Africa, Australia and Mexico.
We now proceed to a detailed analysis of the selected studies (Table 3).
| Table 3. Summary of selected and reviewed articles | |||||
|---|---|---|---|---|---|
| Study | Number of studies | Population | Implementing institution | Geographical setting | Area of interest |
| Mann KD (2017) | 11 studies | General population | Health care system | United Kingdom, Italy, France, USA, Singapore, Australia, Ireland, Norway, Sweden and Denmark | 1 |
| Corvalán C (2019) | - | General population | Public administration | Chile | 1 |
| Singh P (2015) | 18 studies | General population | Health care system | South Africa | 6 |
| Steinberger J (2016) | Guideline | Children | Health care system | USA: American Heart Association | 10 |
| Flodgren G (2017) | 12 studies | Health professionals | Health care system | United Kingdom, USA, Australia | 7 |
| Cohen JE (2016) | 3 studies | <21 years | Health care system | USA | 6 |
| Wolfenden L (2017) | 27 studies | General population | Health care and school systems | USA | 1, 2, 7 |
| Gray-Burrows K (2017) | 111 studies | 0-5 years | Health care system | United Kingdom | 5 |
| De Silva. (2016) | 38 studies | 0-18 years | Health care system | USA | 5 |
| Singh A (2017) | 27 studies | 6-18 years | School system | USA | 1, 2, 7 |
| Gittelsohn J (2017) | 10 | General population | Public administration | USA, México, Pacific Islands | 1 |

The study published by Mann et al. in 201731 analysed nutritional statistics from different countries in the European Union and the United States. The main aspect we would like to highlight is its substantial scope, which allowed it to support several recommendations regarding the prevention of overweight and obesity in children through increasing the intake of whole grains. The study also provides recommendations on the nutrient composition of the weekly diet, proposing consumption of high amounts of whole grains combined with fruits and vegetables.
The study conducted in Chile,28 the country with the highest prevalence of obesity in the world (24.6% in children aged 6-7 years) stands out because it focuses on the enactment of a law that seeks to promote healthy nutrition. The authors predict that policies aimed at reducing consumption of sugars and increasing consumption of healthy foods will achieve a decrease in the prevalence of obesity in upcoming years.
Another review9 focuses on the change in the attitudes and behaviours of health professionals in relation the prevention of chronic diseases in children and adults. Thus, health professionals, along with teachers, are considered the primary agents of change in the early stages of life. Two studies assessed the impact of multidisciplinary teams. Weight loss programmes led by a dietitian or a physician in collaboration with a dietitian can achieve greater losses in adult patients compared with standard care. Shared care (between family physicians, hospital-based physicians and dieticians) seems to achieve little to no change in the body mass index (BMI, a measure of the relationship of height and weight) in children with obesity compared to standard care.
Several articles advocate for training health professionals and the development of guidelines for the prevention of overweight and obesity in children.9,14 Dietary recommendations for the prevention of chronic diseases are also developed from within the health care system, as is the case of a study included in this review focused on the prevention of childhood cancer.32
In 2017, Wolfenden et al. published a review of the evidence on the impact of programmes based on dietary interventions, daily physical activity, obesity and tobacco and alcohol use.30 The impact of these programs was reflected, for instance, in the increase in the minutes devoted to preventive practices (ranging from 26.6 to 54.9 minutes/week). The authors concluded that the evidence on school-based preventive services was of very poor quality and that it was uncertain whether they were effective in promoting healthy behaviours and changing the attitudes of school staff. They also suggested that these interventions may have a high cost-benefit ratio.
Along the same lines, we also ought to mention the review published by Singh et al. in 2017 of the evidence on the impact of school policies on risk factors for NCDs.33 School policies are effective in preventing specific risk factors. The authors highlighted the reduction in sugar intake, although they did not find changes in behaviour or biological markers. None of the studies in this review provided data on long-term outcomes.
Another study that deserves attention is a 10-year review of high-impact articles on the effects of social policies for the prevention of obesity and diabetes.29 This review included a detailed analysis of food consumption, the most frequently purchased foods and even analysed evidence on cooking methods and diet. The authors concluded the review with alarming data regarding the increase of obesity in regions with poor resources or frequent changes in government, such as Mexico. This suggests that the observed increase is related to the unsustainability of healthy lifestyle changes and the lack of access to healthy foods in these areas.
Studies in the field of oral health focused on interventions at 2 levels: intergenerational interventions, from parents to children, and social interventions.34,35 Some of the recommendations were, for instance, to establish stricter sanctions in relation to child restraint systems for road safety or child abuse, as well as appropriate protocols for the management of oral trauma in children. In relation to future goals, the studies were clear on the need of increasing the taxes imposed on sugary drinks, limiting advertising of sugary foods to children and adolescents and providing simplified dietary guidelines, including recommendations on sugar intake.
DISCUSSION
Research on the implementation of school-based interventions for the prevention of chronic diseases is no longer in the early stages.36 The subject that predominates in this field in the prevention of noncommunicable diseases, especially those that are most prevalent, with performance of randomised controlled clinical trials in search of effective interventions for the prevention of childhood overweight and obesity, followed in frequency by studies on oral health. Some of the studies included in the analysed reviews described alternative approaches to the treatment of certain diseases, such as the use of virtual reality or videogames.37
Schools can improve the health and academic performance of students by creating opportunities to practice healthy behaviours and creating a safe and healthy environment inclusive of the family and the community.38 Several studies conducted in Chile and Spain have analysed the impact of chronic diseases on the health-related quality of life of children, evincing significant discrepancies in the perceptions of patients and clinicians, especially in socio-affective aspects.39,40
The development of any disease in a child poses a significant challenge. If the disease is severe enough to require hospitalization, the challenge grows exponentially, as the child is introduced in a new system, which is a new source of stressors and struggles to add to the already existing ones. In the case of chronic diseases, there are significant changes in the daily life of patients that affect wellbeing and quality of life and require coping skills to adjust to the new situation. Anxiety, depression and other forms of negative affect are commonly observed in patients with chronic diseases. The way that these negative emotions are handled has an impact on the adjustment to the disease.
There are two general patterns of emotion regulation. One involves avoidance and inhibition of the emotion, a maladaptive pattern that may result in poorer outcomes. In contrast, awareness and expression of emotions may help adjust well to a new situation. However, the experience of disease may also affect emotion regulation. As survival improves and medical knowledge progresses, the prevalence of chronic diseases also increases. In these cases, psychological adjustment to the new situation is essential. Although most of the research on the adjustment to chronic diseases have focused on the psychological difficulties experienced by patients, there are also studies that describe how patients manage to maintain positive lifestyle habits.41 Many patients adjust successfully to the changes imposed by a chronic condition.
Understanding the need for long-term adjustment helps patients cope with limitations to activity. This adaptation makes it possible to acknowledge and manage the development of negative emotions elicited by the disease and to use coping skills to improve quality of life. Overcoming the negative consequences of the disease may reap additional benefits.
Thus, in addition to the approach at the school level, as we noted early in this article, the development of disease is intimately tied to family behaviour and the culture where the child grows up. There is evidence that factors at different levels (family attitudes, ethnicity, legal framework, local policies, etc) can contribute to achieving substantial outcomes in the prevention of overweight and obesity in the paediatric population.13 These studies suggest that this methodology could be applied to other diseases that affect children and adolescents, such as alcohol, tobacco or drug use.
On the subject of diseases that are the target of prevention programmes in children and adolescents, the main area of interest is the prevention and management of overweight and obesity, the topic studied most frequently in Spain and abroad. This is an important finding in comparison to the study published by Davó et al. in 200836 that analysed interventions for the prevention of chronic diseases in school-age children implemented in Spain between 1995 and 2005. Their study showed that most prevention efforts at the time were aimed at decreasing tobacco use in youth. This is also evidence of the sharp increasing trends observed in BMI, blood lipid levels and physical inactivity in children and adolescents in the past decade.
Closing this subject, the WHO, in its indefatigable work for the recognition, prevention and treatment of NCDs, developed a Global Action Plan for 2013-202042 that considered the need for adaptations taking into account the situation and public health priorities of each region, and proposing measures framed in six interconnected and mutually reinforcing objectives: i) international cooperation; ii) country-led response; iii) risk factors; iv) health care systems; v) research and vi) surveillance. Based on data of the highest possible quality and the available scientific evidence, the Action Plan offers member states a menu of options to prevent and monitor NCDs that must be adapted and integrated into existing public health and social welfare plans in consideration of the legal framework, priorities and specific circumstances of each country.
To obtain more information on the development of different programmes for the prevention of NCDs in children and adolescents, it would be necessary to carry out a broader investigation of programmes implemented by regional and local authorities as well as private initiatives using additional sources besides scientific journals. We believe that a constellation of interventions, as opposed to isolated interventions, are required to achieve significant changes in awareness in the general population. An appropriate initial step would be to establish measures for direct evaluation in the school and primary care settings.
In conclusion, the implementation of direct and effective strategies stems from government institutions and reaches the target population, in this case children and adolescents, through the health care and education systems. Science helps us determine which ways are efficient to produce changes in habits and behaviours for the prevention of NCDs at the population level, and thus it is of vital importance to develop plans in which interventions on the paediatric population are tangible and immediate, given the magnitude of the problem.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
BMI: body mass index · NCD: noncommunicable disease · WHO: World Health Organization.
REFERENCES
- Terán GJ, Montenegro BL, Bastidas JL, Realpe IA, Villarreal FJ, Fernández A. Análisis crítico de la responsabilidad social en entidades de salud. Rev Cubana Inv Biomed. 2017;36:1-8.
- Tercedor P, Jiménez MJ, López B. La promoción de la actividad física orientada hacia la salud. Un camino por hacer. Eur J Hum Mov. 1998;4:203-17.
- Borrell C, Artazcoz L. Las políticas para disminuir las desigualdades en salud. Gac Sanit. 2008;22:465-73.
- 10 datos sobre las enfermedades no transmisibles. In: World Health Organization [online] [accessed 09/06/2021]. Available at www.who.int/features/factfiles/noncommunicable_diseases/es/
- Bahekar AA, Singh S, Saha S, Molnar J, Arora R. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J. 2007;154:830-7.
- Söder B, Yakob M, Meurman JH, Andersson LC, Klinge B, Söder PÖ. Periodontal disease may associate with breast cancer. Breast Cancer Res Treat. 2011;127:497-502.
- Kinane D, Bouchard P; Group E of European Workshop on Periodontology. Periodontal diseases and health: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35:333-7.
- Romero-Velarde E, Campollo-Rivas O, de la Rosa AC, Vásquez-Garibay EM, Castro-Hernández J F, Cruz-Osorio RM. Factores de riesgo de dislipidemia en niños y adolescentes con obesidad. Salud Pública Méx. 2007;49:103-18.
- Flodgren G, Gonçalves-Bradley DC, Summerbell CD. Interventions to change the behaviour of health professionals and the organisation of care to promote weight reduction in children and adults with overweight or obesity. Cochrane Database Syst Rev. 2017;1:CD000984.
- Gómez Santos SF, Estévez Santiago R, Palacios Gil-Antuñano N, Leis Trabazo MR, Tojo Sierra R, Cuadrado Vives C, et al. Programa THAO-salud infantil: intervención de base comunitaria de promoción de estilos de vida saludables en la población infantil y las familias: resultados de un estudio de cohorte. Nutr Hosp. 2015;32:2584-7.
- Serrano Patten AC. Estudio de casos sobre afrontamiento familiar ante enfermedades crónicas en niños y adolescentes.Rev Elec Psic Izt. 2017;18:706-32.
- Wilson CJ, de la Haye K, Coveney J, Hughes DL, Hutchinson A, Miller C, et al. Protocol for a randomized controlled trial testing the impact of feedback on familial risk of chronic diseases on family-level intentions to participate in preventive lifestyle behaviors. BMC Public Health. 2016;16:965.
- Schwendler T, Shipley C, Budd N, Trude A, Surkan PJ, Anderson Steeves E, et al. Development and Implementation: B'More Healthy Communities for Kid's Store and Wholesaler Intervention. Health Promot Pract. 2017;18:822-32.
- Lobos Fernández LL, Leyton Dinamarca B, Kain Bercovich J, Vio del Río F. Evaluación de una intervención educativa para la prevención de la obesidad infantil en escuelas básicas de Chile. Nutr Hosp. 2013; 28:1156-64.
- Finch M, Yoong SL, Thomson RJ, Seward K, Cooney M, Jones J, et al. A pragmatic randomised controlled trial of an implementation intervention to increase healthy eating and physical activity-promoting policies, and practices in centre-based childcare services: study protocol. BMJ Open. 2015;5:e006706.
- Del Rey R, Ortega R. Programas para la prevención de la violencia escolar en España: la respuesta de las comunidades autónomas. Rev Inter Form Prof. 2001;41:133-45.
- Flujas-Contreras JM, Ruiz-Castañeda D, Botella C, Gómez I. Un programa de bienestar emocional basado en Realidad Virtual y Terapia Online para enfermedades crónicas en infancia y adolescencia: la Academia Espacial. RPCNA. 2017;3:17-25.
- Althabe F, Alemán A, Berrueta M, Morello P, Gibbons L, Colomar M, et al. A multifaceted strategy to implement brief smoking cessation counseling during antenatal care in Argentina and Uruguay: a cluster randomized trial. Nicotine Tob Res. 2016;18:1083-92.
- Albright CL, Saiki K, Steffen AD, Woekel E. What barriers thwart postpartum women's physical activity goals during a 12-month intervention? A process evaluation of the Nā Mikimiki Project. Women Health. 2015;55:1-21.
- Shenkman E, Muller K, Vogel B, Nixon SJ, Wagenaar AC, Case K, et al. The wellness incentives and navigation project: design and methods. BMC Health Serv Res. 2015;15:579.
- WHO. SDIT. Dieta, nutrición y prevención de enfermedades crónicas. In: World Health Organization [online] [accessed 09/06/2021]. Available at www.who.int/nutrition/publications/obesity/WHO_TRS_916_spa.pdf
- Wong R, Espinoza M, Palloni A. Adultos mayores mexicanos en contexto socioeconómico amplio: salud y envejecimiento. Salud Pública Méx. 2007;49:S436-47.
- Calonge Pascual S, Casajús Mallén JA, González-Gross M. La actividad física en el currículo universitario español de los grados de Medicina y Ciencias de la Actividad Física y del Deporte como recurso en la prevención y tratamiento de las enfermedades crónicas. Nutr Hosp. 2017;34:961-8.
- McKenzie TL, Lounsbery MA. Physical education teacher effectiveness in a public health context. Res Q Exerc Sport. 2013;84:419-30.
- Enfermedades no transmisibles: perfiles de países. In: World Health Organization [online] [accessed 09/06/2021]. Available at www.who.int/nmh/countries/esp_es.pdf?ua=1
- Cerdá JM, Argani MT, Llerda JM, González FL, Puig XS, Rieger JS. Guía oficial de la Sociedad Española de Neurología de práctica clínica en epilepsia. Neurología. 2016;31:121-9.
- Steinberger J, Daniels SR, Hagberg N, Isasi CR, Kelly AS, Lloyd-Jones D, et al. Cardiovascular Health Promotion in Children: Challenges and Opportunities for 2020 and Beyond: A Scientific Statement From the American Heart Association. Circulation. 2016;134:e236-55.
- Corvalán C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: Update on the Chilean law of food labelling and advertising. Obes Rev. 2019;20:367-74.
- Gittelsohn J, Trude A. Diabetes and obesity prevention: changing the food environment in low-income settings. Nutr Rev. 2017;75:S62-9.
- Wolfenden L, Nathan NK, Sutherland R, Yoong SL, Hodder RK, Wyse RJ, et al. Strategies for enhancing the implementation of school-based policies or practices targeting risk factors for chronic disease. Cochrane Database Syst Rev. 2017;11:CD011677.
- Mann KD, Pearce MS, Seal CJ. Providing evidence to support the development of whole grain dietary recommendations in the United Kingdom. Proc Nutr Soc. 2017;76:369-77.
- Cohen JE, Wakefield CE, Cohn RJ. Nutritional interventions for survivors of childhood cancer. Cochrane Database Syst Rev. 2016;2016:CD009678.
- Singh A, Bassi S, Nazar GP, Saluja K, Park M, Kinra S, et al. Impact of school policies on non-communicable disease risk factors - a systematic review. BMC Public Health. 2017;17:292.
- Gray-Burrows KA, Owen J, Day PF. Learning from good practice: a review of current oral health promotion materials for parents of young children. Br Dent J. 2017;222:937-43.
- De Silva AM, Hegde S, Akudo Nwagbara B, Calache H, Gussy MG, Nasser M, et al. Community-based population-level interventions for promoting child oral health. Cochrane Database Syst Rev. 2016;9:CD009837.
- Davó MC, Gil-González D, Vives-Cases C, Álvarez-Dardet C, La Parra D. Las investigaciones sobre promoción y educación para la salud en las etapas de infantil y primaria de la escuela española: una revisión de los estudios publicados entre 1995 y 2005. Gac Sanit. 2008;22:58-64.
- Nigg CR, Mateo DJ, An J. Pokémon GO may increase physical activity and decrease sedentary behaviors. Am J Public Health. 2017;107:37-8.
- Michael SL, Merlo CL, Basch CE, Wentzel KR, Wechsler H. Critical connections: health and academics. J Sch Health. 2015;85:740-58.
- Avendaño Monje MJ, Barra Almagiá E. Autoeficacia, apoyo social y calidad de vida en adolescentes con enfermedades crónicas. Ter psicol. 2008;26:165-72.
- Roizen M, Figueroa C, Salvia L. Calidad de vida relacionada con la salud en niños con enfermedades crónicas: comparación de la visión de los niños, sus padres y sus médicos. Arch Argent Pediatr. 2007;105:305-13.
- Cruz Martín O, León MM, Machado Machado Y. Caracterización emocional de niños escolares hospitalizados con enfermedades crónicas. Rev Cubana de Pediatr. 2014;86:462-69.
- Plan de acción mundial para la prevención y el control de las enfermedades no transmisibles 2013-2020. In: World Health Organization [online] [accessed 09/06/2021]. Available at www.who.int/cardiovascular_diseases/15032013_updated_revised_draft_action_plan_spanish.pdf