Vol. 22 - Num. 88
Original Papers
Prescription of antibiotics in children in primary care. Study in an administrative area of Osakidetza-Basque Health Service
José M.ª Arginzoniz Marzanaa, Ane Antón Ladislaob, Nekane Jaio Atelac, María Armendáriz Cuñadoc
aPediatra. CS de Iurreta. Vizcaya. España.
bUnidad de Investigación. Hospital Galdakao-Usansolo. Red de Investigación en Servicios de Salud en Enfermedades Crónicas (REDISSEC). Vizcaya. España.
cFarmaceútica de Atención Primaria. OSI Barrualde-Galdakao. Osakidetza-Servicio Vasco de Salud. Vizcaya. España.
Correspondence: JM Arginzoniz. E-mail: txemarginzoniz@gmail.com
Reference of this article: Arginzoniz Marzana JM, Antón Ladislao A, Jaio Atela N, Armendáriz Cuñado M. Prescription of antibiotics in children in primary care. Study in an administrative area of Osakidetza-Basque Health Service. Rev Pediatr Aten Primaria. 2020;22:363-70.
Published in Internet: 23-11-2020 - Visits: 11932
Abstract
Introduction: based on the current literature, the consumption of antibiotics in children is high in Spain. However, there may be large differences even between small geographic areas. The objective of the study was to establish the frequency of antibiotic prescription in the paediatric age group and describe the characteristics of these prescriptions in the in the Barrualde-Galdakao integrated health care area of the Osakidetza-Basque Health System.
Methods: we made a retrospective analysis of antibiotic prescriptions made to children aged 0 to 13 years in years 2015, 2016 and 2017. We retrieved the data from the Presbide database of the Osakidetza-Basque Health System. We calculated rates of antibiotic-treated episodes and the prevalence of antibiotic use, and analysed the distribution by type of antibiotic.
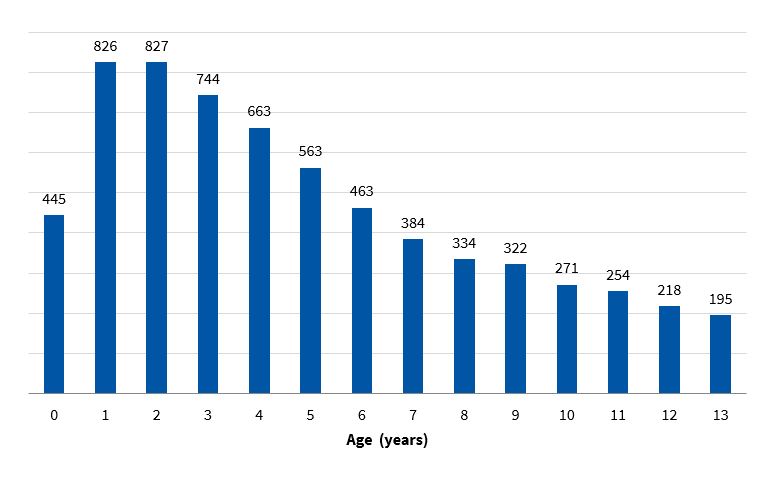
Results: we analysed 56 974 antibiotic prescriptions dispensed to 40 824 children over a 3-year period. The number of antibiotic-treated episodes per 1000 children/year was 465.20. The percentage of children who received at least one antibiotic per year was 30.72. The highest rates of antibiotic use occurred in children aged 1 and 2 years (826 and 827 episodes treated/1000 children/year respectively), and 64.61% of the dispensed prescriptions were for amoxicillin
Conclusion: The frequency of antibiotic use in children found in our study was high compared to countries with a low frequency of antibiotic prescription in Europe and significantly lower compared to the results of other studies conducted in Spain and other Mediterranean countries.
Keywords
● Antibiotics ● Children ● Pharmacoepidemiology ● Prescription ● Primary careINTRODUCTION
Inappropriate antibiotic use not only causes individual harm and increases health care expenditure, but may also contribute to the development of drug-resistant bacteria,1 which leads to serious public health problems.2 Most antibiotics are prescribed at the primary care level,3 with the highest frequency of prescriptions corresponding to the 0-4 years age group.3,4
In up to 60% of cases, antibiotics are used for treatment of respiratory infections,5 most of which are viral, and some authors estimate that antibiotic use may be inappropriate in up to 50% of cases.6
Spain, along with other countries in the Mediterranean region, is one of the greatest consumers of antibiotics in Europe,7 and the few studies conducted on the subject in children have identified the same trend.8 However, there may be significant differences in the use of antibiotics in children not only between countries,8,9 but also between regions in the same country10 and between prescribers in smaller geographical areas.11,12
Overall, antibiotic use in the Basque Country is high, with figures that are very similar to those of other regions in Spain,13 but we are not aware of any studies of antibiotic prescription in children in this autonomous community.
The aim of our study was to describe antibiotic prescription in the paediatric age group and its characteristics in the Barrualde-Galdakao integrated health care area (IHCA) of the public health system of the Basque Country (Osakidetza).
MATERIAL AND METHODS
We conducted a retrospective cohort study in the Barrualde-Galdakao IHCA, making a descriptive analysis of antibiotic prescription in children. The Barrualde-Galdakao IHCA of the Osakidetza-Basque Health System includes 17 primary care units (PCUs) serving a catchment population of 313 000 inhabitants. We included children aged 0 to 13 years that received prescriptions in 2015, 2016 and 2017.
We obtained the data from the outpatient prescription database of the Osakidetza-Basque Health System (Presbide). This database includes information on the type of antibiotic prescribed using Anatomical, Therapeutic, Chemical (ATC) classification system codes, the date of prescription and dispensation, the patient identification code and the age, sex and PCU of the patient. We analysed with ATC code J01 (antibacterials for systemic use); thus excluding drugs for treating tuberculosis, antifungal and antiparasitic drugs and topical antibacterials. We excluded prescriptions that were not dispensed by the pharmacy system. If we found records of the same antibiotic being dispensed 2 or more times within a period of up to 14 days, we counted it a single instance of dispensation (1 treated episode).
We analysed the following variables: number of antibiotic dispensations or episodes treated with antibiotics per 1000 children per year (rate of antibiotic-treated episodes) and the distribution of antibiotic prescription by age, month of year and PCU, the percentage of children that received at least 1 antibiotic dispensation per year (prevalence of antibiotherapy) and the distribution by age group and sex. We also analysed the type of antibiotics used and corresponding proportions, and the distribution by subgroups, for which we established the categories of first- and second-line penicillins, first- and second-generation macrolides, cephalosporins and other (Table 1).
| Table 1. Classification of antibiotics | |
|---|---|
| First-line penicillins | Amoxicillin, ampicillin, dicloxacillin, oxacillin, penicillin V potassium |
| Second-line penicillins | Amoxicillin-clavulanic acid |
| First-generation macrolides | Erythromycin, josamycin |
| Second-generation macrolides | Azitromicina, clarithromycin, roxithromycin |
| Cephalosporins | Cefaclor, cefadroxil, cefixime, cefuroxime, ceftibuten, cefalexin, ceftibuten, cefditoren, cefpodoxime, cefprozil |
| Others | Quinolones, clindamycin, doxycycline, minocycline, nitrofurantoin, vancomycin, linezolid, trimethoprim-sulfamethoxazole |

To perform this analysis, we used absolute frequency and percent distributions and compared them between groups by means of the χ2 test.
We obtained data regarding the population from the Osabide database of the Osakidetza-Basque Health System.
All the analyses were made with the statistical software SAS 9.4.
RESULTS
The study population consisted of 40 901 children in 2015, 41 059 in 2016 and 40 512 in 2017, of which 48.12% were girls.
We analysed a total of 56 974 dispensed antibiotic prescriptions corresponding to the period under study. There were 7814 prescriptions (12.06%) that were never dispensed through the pharmacy system. We did not include 6375 dispensations (10.06%) in the count because they were instances of repeated dispensation of the same antibiotic to the same patient within a 14-day window.
In the period under study, the rate of antibiotic-treated episodes was of 465.20/1000 children/year and the percentage of children with at least 1 treated episode/year was 30.72%.
The age distribution of antibiotic-treated episodes (Figure 1) shows that the incidence peaked at ages 1 and 2 years (826 and 827 treated episodes per 1000 children/year, respectively), with a fairly even decrease at later ages.
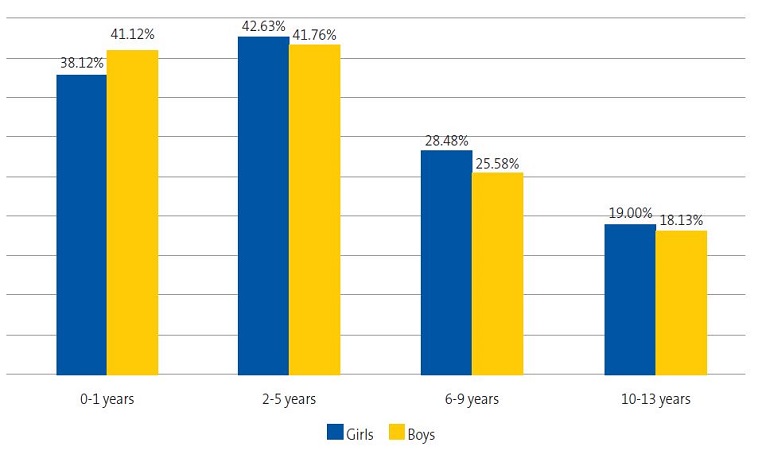
Figure 2 shows that early childhood (ages 2-5 years) was the age range corresponded to the highest frequency of antibiotic use (p <0.0001). The prevalence was also greater in male infants compared to female infants (0-1 years; p <0.0001), but this predominance inverted starting at preschool age, when prescription became more frequent in girls.
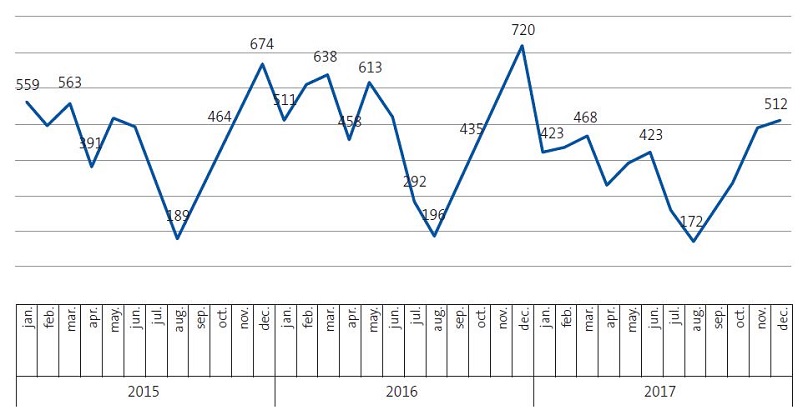
In the years under study, 59.43% of antibiotic treatments took place in the first and last trimesters of the year, with an incidence of treated episodes of 553/1000 children/year, higher compared to the April-September semester, in which the incidence was 378/1000 children/year. In the aforementioned trimesters, antibiotic prescriptions exceeded prescriptions made the rest of the year by 32%. Figure 3 shows the differences between months in the frequency of antibiotic-treated episodes in the years under study.
| Figure 3. Rate of antibiotic-treated episodes (per 1000 children/year) per month and year under study |
|---|
 |

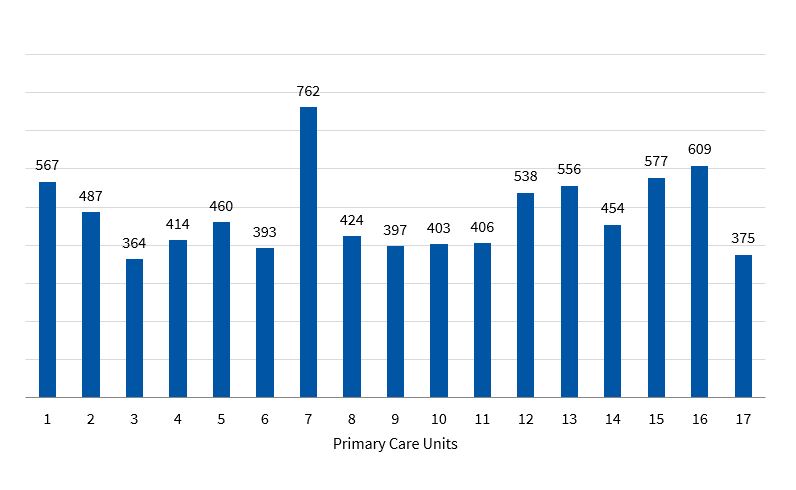
The frequency of antibiotic-treated episodes in the different PCUs ranged from 364/1000/children/year to 762/1000 children/year, and many of these were statistically significant (p <0.0001). Figure 4 presents the figures for the 17 PCUs.
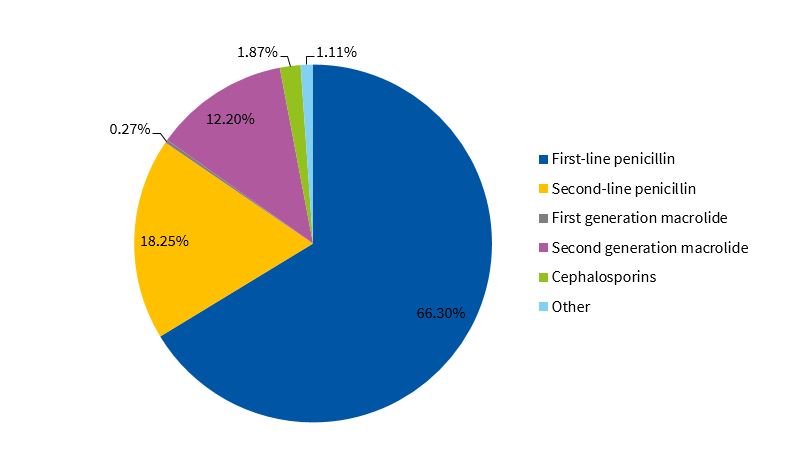
Table 2 shows the most frequently used antibiotics. Three antibiotics accounted for more than 90% of the total dispensations: amoxicillin, amoxicillin-clavulanic acid and azithromycin. This was also the case in 15 of the 17 PCUs included in the study. We ought to highlight the infrequent use of cephalosporins (1.87%) penicillin V (1.62%), erythromycin (0.24%) and cloxacillin (0.07%).
| Table 2. Antibiotics prescribed most frequently | ||
|---|---|---|
| Antibiotic | Dispensations (n) | % |
| Amoxicillin | 36 811 | 64.61 |
| Amoxicillin-clavulanic acid | 10 401 | 18.25 |
| Azithromycin | 5927 | 10.40 |
| Other | 3835 | 6.73 |

Figure 5 presents the distribution of the dispensed antibiotics by subgroup. We found that 66.3% of prescriptions corresponded to first-line penicillins, with amoxicillin accounting for nearly all of these prescriptions (97%). Azithromycin accounted for 91% of the macrolides.
DISCUSSION
The rate of 465.34 antibiotic-treated episodes per 1000 children/year and an annual antibiotic use prevalence of 30.72% indicates that in our region, antibiotic prescription in children is higher compared to countries that with historically low rates of antibiotic prescription, such as the Netherlands9,14,15 and Norway8, but also substantially lower, based on the available data, to the frequency in other areas of Spain4,8,16 and other countries in the Mediterranean region.8,10,17. The antibiotic dispensation figures we found were also lower compared to those reported in studies conducted in Germany8,9,18 and similar to those reported in the United Kingdom.9,14,19
The seasonal variation in dispensation in our catchment area reflects the high antibiotic prescription pattern associated with winter outbreaks of disease, which are known to be caused by viruses. Seasonal peaks have been found to be most pronounced in countries with high antibiotic utilisation,9 but we did not find any studies that measured these variations in the paediatric population, which in our study was of 32%.
We found significant homogeneity in the antibiotics selected by clinicians, which may be indicative of adherence to protocols or clinical guidelines.
Although 66.3% of antibiotic treatments were done with first-line penicillins, our data show a very infrequent use of narrow-spectrum antibiotics such as penicillin V and antistaphylococcal penicillins. Difficulties with the administration of oral dosage forms of these antibiotics (interactions with food, bad taste) are probably the main reason why they are displaced by other broader-spectrum drugs. The use of amoxicillin-clavulanic acid and cephalosporins in our study was much lower compared to previous studies of national scope.8,20
The significant differences in prescription observed between PCUs corroborated the findings of other studies10,12 on the variability of antibiotic use, even in very small geographical areas. The prescription practices in clinicians are often influenced by how clinicians handle diagnostic uncertainty and parental expectations, and this aspect is probably one of the greatest contributors to the observed variability.12. We agree with other authors10,21 that an awareness of clinicians of the characteristics of their prescribing practices and a more local approach to the development of antibiotic stewardship strategies are a necessary complement to strategies of a more general scope.
In conclusion, we present the first study of antibiotic prescription in children in the Basque Country. The antibiotic dispensation figures obtained in this study fell between those observed in high-prescription and low-prescription countries in Europe. We found substantial homogeneity in the selection of the antibiotics to use, and substantial variability in the frequency of prescription between PCUs. Most antibiotic treatments involved use of first-line penicillins, with infrequent use of narrow-spectrum antibiotics. We ought to mention some of the limitations of the study: our results underestimate the antibiotics given to children, as we did not have access to data from the private sector, and we did not know the diagnoses that motivated the prescriptions, which limited our ability to assess whether the use of antibiotics was appropriate.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
ATC: Anatomical, Therapeutic, Chemical Classification System · IHCA: Integrated Health Care Area · PCU: primary care unit.
ACKNOWLEDGMENTS
Lehen Arreta Pediatrikoa Miatzen (LAPM) Group: Iñaki Ávalos Román (paediatrician, CS de Ermua), Nahia Arantzamendi Artola (paediatrician, CS de Ermua), Itziar Fernández Repaldiza (paediatrician, CS de Durango), Esther Gorostiza Garai (paediatrician, CS de Matiena), Isabel Molina Zelaia (paediatrician, CS de Durango), Nekane Morato Rodríguez (paediatrician, CS de Durango), Amaia San Sebastián Ruiz (family physician, CS de Elorrio), M. Jesús Sarrionandia Uribelarrea (paediatrician, CS de Abadiño), Aranzazu Lorena Tajada Zabalbeitia (paediatrician, CS de Durango) and Oihane Zubiaur Alonso (CS Berriz-Zaldibar). Vizcaya, Spain.
REFERENCES
- Costelloe C, Metcalfe C, Lovering A, Mant D, Hay A. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096-3006.
- Chung A, Perera R, Brueggemann AB, Elamin AE, Harnden A, Mayn-White R. Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: Prospective cohort study BMJ. 2007;335:429-33.
- Blix HS, Engeland A, Litleskare I, Ronning M. Age- and gender-specific antibacterial prescribing in Norway. J Antimicrob Chemother. 2007;59:971-6.
- Lallana-Álvarez mj, Feja-Solana c, Armesto-Gómez J, Bjerrum L, Rabanaque-Hernández MJ. Prescripción extrahospitalaria de antibióticos en Aragón y sus diferencias por género y edad. Enferm Infecc Microbiol Clin. 2012;30:591-6.
- Bryant V, Timoner J, Oliva B, Gil M, Alegre P, de Abajo FJ. Análisis de la utilización de antibióticos en población pediátrica con patología respiratoria. Estudio en la base de datos BIFAP. Rev Pediatr Aten Primaria. 2009;11:s36-s36.
- Calvo C, Albañil MR, Sánchez M, Olivas A. Patrones de prescripción de antibióticos en Atención Primaria. ¿Usamos racionalmente los antibióticos en Pediatría? An Esp Pediatr. 2000;52:157-63.
- Cars O, Mölstad S, Melander A. Variation in antibiotic use in the European Union. Lancet. 2001;357:1851-3.
- Youngster I, Avorn J, Belleudi V, Cantarutti A, Díez-Domingo J, Kirchmayer U, et al. Antibiotic Use in Children - A Cross-National Analysis of 6 Countries. J Pediatr. 2017;182:239-44.
- Holstiege J, Schink T, Molokhia M, Mazzaglia G, Innocenti F, Oteri A, et al. Systemic antibiotic prescribing to paediatric outpatients in 5 European countries: a population-based cohort study. BMC Pediatr. 2014;14:174-83.
- Piovani D, Clavenna A, Cartabia M, Bonati M. The regional profile of antibiotic prescriptions in Italian outpatient children. Antibiotic Collaborative Group. Eur J Clin Pharmacol. 2012;68:997-1005.
- Vázquez ME, Pastor E, Bachiller MR, Vázquez MJ, Eiros JM. Variabilidad geográfica de la prescripción de antibióticos en la población pediátrica de Castilla y León durante el periodo 2001 a 2005. Rev Esp Quimioterap. 2006;19:342-8.
- Di Martino M, Lallo A, Kirchmayer U, Davoli M, Fusco D. Prevalence of antibiotic prescription in pediatric outpatients in Italy: the role of local health districts and primary care physicians in determining variation. A multilevel design for healthcare decision support. BMC Public Health. 2017;17:886-93.
- Indicadores clave del Sistema Nacional de Salud. In: Ministerio de Sanidad, Consumo y Bienestar Social [online] [accessed 19/11/2020]. Available at http://inclasns.msssi.es/report/area/
- De Bie S, Kaguelidou F, Verhamme KM, De Ridder M, Picelli G, Straus SM, et al. Using Prescription Patterns in Primary Care to Derive New Quality Indicators for Childhood Community Antibiotic Prescribing. Pediatr Infect Dis J. 2016;35:1317-23.
- De Bont EG, van Loo IH, Dukers-Muijrers NH, Hoebe CJ, Bruggeman CA, Dinant GJ, et al. Oral and topical antibiotic prescriptions for children in general practice. Arch Dis Child. 2013;98:228-31.
- Serna MC, Ribes E, Real J, Galván L, Gascó E, Godoy P. Alta exposición a antibióticos en la población y sus diferencias por género y edad. Aten Primaria. 2011;43:236-44.
- Kourlaba G, Kourkouni E, Spyridis N, Gerber JS, Kopsidas J, Mougkou K, et al. Antibiotic prescribing and expenditures in outpatient paediatrics in Greece, 2010-13. J Antimicrob Chemother. 2015;70:2405-8.
- Holstiege J, Garbe E. Systemic antibiotic use among children and adolescents in Germany: a population-based study. Eur J Pediatr. 2013;172:787-95.
- Schneider-Lindner V, Quach C, Hanley JA, Suissa SJ. Secular trends of antibacterial prescribing in UK paediatric primary care. J Antimicrob Chemother. 2011;66:424-33.
- Vázquez Fernández ME, Luquero Alcalde FJ, Pastor García E, Bachiller Luque MR, Vázquez Fernández MJ, Eiros Bouza JM. Análisis del consumo de antibióticos en la población pediátrica de Castilla y León durante el periodo 2001 a 2005. An. Pediatr (Barc). 2007;67:11-7.
- Albañil Ballesteros MR, Calvo Rey C, Sanz Cuesta T. Variación de la prescripción de antibióticos en Atención Primaria. An Esp Pediatr. 2002;57:420-6.