Electrocardiographic and echocardiographic abnormalities in female adolescents with anorexia nervosa
Álvaro Martín Rivadaa, Clara Luna Parera Pinillaa, Antonio Baño Rodrigob, Raquel Jiménez Garcíac, Amalia Tamariz Martel-Morenob
aMIR-Pediatría. Hospital Infantil Universitario Niño Jesús. Madrid. España.
bServicio de Cardiología Pediátrica. Hospital Infantil Universitario Niño Jesús. Madrid. España.
cSección de Pediatría. Hospital Infantil Universitario Niño Jesús. Madrid. España.
Correspondence: A Martín. E-mail: amrivada@salud.madrid.org
Reference of this article: Martín Rivada A, Parera Pinilla CL, Baño Rodrigo A, Jiménez García R, Tamariz Martel-Moreno A. Electrocardiographic and echocardiographic abnormalities in female adolescents with anorexia nervosa. Rev Pediatr Aten Primaria. 2020;22:e13-e19.
Published in Internet: 21-01-2020 - Visits: 19248
Abstract
Introduction: the aim of the study was to describe the electrocardiographic and echocardiographic findings in female adolescents with anorexia nervosa and to assess their correlation with clinical variables.
Patients and methods: we conducted a retrospective observational case-control study. The analysis included 98 female adolescents admitted to a tertiary hospital due to anorexia nervosa over the last 15 years, all of who underwent an electrocardiographic and echocardiographic evaluation.
Results: the mean age was similar in both groups: 14.6 ± 2.0 years in cases vs. 14.7 ± 2.0 years in controls. Patients with anorexia had significantly lower heart rates (57 ± 12 vs. 72 ± 13 bpm), a smaller R-wave in V5 (1.1 ± 0.5 vs 1.6 ± 0.4 mV) and a lesser left ventricular mass (65.7 ± 14.8 vs 90 ± 15.3 g/m2) compared to controls. We found no differences in the QTc interval. In patients with anorexia, the presence of bradycardia was not correlated to weight (r = -0.20, p = 0.05) or body mass index (r = 0.02, p = 0.22) at admission. We found that the left ventricular mass was significantly correlated to the body mass index (r = 0.21, p <0.001,) and the heart rate (r = -0.225, p <0.001).
Conclusions: cardiac abnormalities were more prevalent in patients with anorexia nervosa. Bradycardia, changes in ventricular repolarization, and a lesser left ventricular mass were the most frequent abnormalities in our sample.
Keywords
● Adolescent ● Anorexia nervosa ● Echocardiography ● ElectrocardiogramINTRODUCTION
Restricting-type anorexia nervosa (RTAN) is characterised by a restriction of energy intake leading to significantly low body weight, an intense fear of gaining weight or persistent behaviour that interferes with weight gain combined with a disturbance in the way in which one’s body weight or shape is perceived.1 It is the psychiatric disorder that has the highest mortality rate,2,3 with death resulting from suicide or complications of weight loss, including cardiac arrhythmias and sudden cardiac death.4,5 The assessment of cardiovascular health is an essential component in the management of these patients, and the electrocardiogram (ECG) is a key tool for this purpose. Electrocardiographic abnormalities in this context were first described in 1975 in 7 patients with anorexia nervosa.6 Since then, numerous studies, systematic reviews and meta-analyses have been published on the subject,7-15 with abnormalities found in up to 75% of patients hospitalised for this disease.7 The most frequently reported abnormalities are sinus bradycardia and changes in repolarization evinced by QT interval prolongation and increased QT dispersion.16 Relative bradycardia and a lower amplitude of the R-wave in V6 have been described as the most useful electrocardiographic markers of severity in patients with anorexia nervosa, as they have been found to be significantly correlated to a lower standardised body mass index (BMI).8,17 Other abnormalities include QRS right axis deviation, decreased QRS and T-wave amplitude and QRS prolongation. Most authors report that these abnormalities can be reversed with weight recovery and improvement of nutritional status. 18-21 Electrocardiographic changes are less apparent in patients with bulimia nervosa or unspecified eating disorder.8
The fasting state generated by the disease involves a transient metabolic adaptation process that varies based on the degree of fasting, the level of physical activity and intrinsic factors such as sex, age, race or body composition.22
The risk factors most frequently associated with hearth rhythm disorders are: electrolyte imbalance (most commonly hypopotassaemia and hypocalcaemia), chronic hypoalbuminaemia and longer duration of disease. In addition, undernutrition leads to changes in cardiac anatomy, mainly a thinning of the ventricular walls and a reduction of the heart chambers, which can then lead to heart failure on refeeding.22
The aim of our study was to describe the electrocardiographic and echocardiographic findings in female adolescent patients with anorexia nervosa and assess their association with clinical and laboratory parameters.
MATERIAL AND METHODS
We conducted a retrospective, observational case-control study analysing the findings of ECG and echocardiography in the initial evaluation of female adolescents following admission to a children’s hospital in the past 15 years.
The cases corresponded to 98 female adolescents with a diagnosis of restricting-type anorexia nervosa. We included patients that met the criteria specified in the Diagnostic and Statistical Manual for Mental Disorders, 5th edition (DSM-5). All patients admitted with RTAN underwent a routine cardiological evaluation at the time of admission that includes the performance of at least 1 conventional 12-lead ECG. In this study, we analysed the findings obtained in this initial inpatient cardiological evaluation following admission for RTAN. Blood tests were also performed in this initial evaluation, including measurement of serum levels of electrolytes (sodium, potassium and calcium).
The control group included 98 healthy female adolescents referred for evaluation to the department of cardiology for other reasons (most frequently heart murmurs or chest pain). We considered that controls were free of cardiovascular disease based on an evaluation that included an ECG and an echocardiogram.
We collected data on demographic variables, clinical variables including the characteristics of the disease, height, weight, arterial blood pressure (BP) and heart rate (HR). We calculated the BMI and the standardised BMI (BMIz) calculating the z-scores based on the standards of the World Health Organization.
The variables documented in the ECG at admission were the resting heart rate, the voltage amplitudes in the 12 leads, repolarization and the corrected QT interval (QTc). We calculated the QTc using the Bazett formula (QT interval divided by the square root of the preceding RR interval), to correct for heart rate extremes. The measured values were recorded electronically.
The evaluation also included a conventional ECG in all patients, with documentation of the following parameters: left ventricular thickness, diameter and mass indexed to body surface area.
We performed the statistical analysis with the software SPSS Statistics version 15.0. We performed the following analyses: descriptive analysis, Student t test for comparison of means, correlation and linear regression equation.
RESULTS
The age of patients was similar in both groups (cases: 14.6 ± 2.0 years; controls: 14.7 ± 2.0 years, difference not statistically significance). The weight (37 ± 5.8 kg versus 52.2 ± 7.4 kg; p < 0.001) and BMI (14.4 ± 1.4 kg/m2 versus 20.2 ± 1.8 kg/m2; p < 0.001) were significantly lower in the case group. Patients with anorexia nervosa had a lower heart rate (57 ± 12 versus 72 ± 13 bpm), lower voltages (RV5 = 1.1 ± 0.5 versus 1.6 ± 0.4 mV; RV6=1.0 ± 0.4 versus 1.4 ± 0.4 mV), and a greater right axis deviation (P-wave axis: 56° ± 22.7° versus 47° ± 21.7°; QRS axis: 82° ± 18.1° versus 73° ± 16.7°) compared to controls. We did not find significant differences in the QTc interval (Table 1). Table 2 shows the number of patients with electrocardiographic changes in each group.
| Table 1. Electrocardiographic measurements in female adolescents with restricting-type anorexia nervosa and controls | |||
|---|---|---|---|
| Cases (mean ± SD) | Controls (mean ± SD) | p-value | |
| HR (bpm) | 57 ± 12 | 72 ± 13 | <0.001 |
| RV5 (mV) | 1.1 ± 0.5 | 1.6 ± 0.4 | <0.001 |
| RV6 (mV) | 1.0 ± 0.4 | 1.4 ± 0.4 | <0.001 |
| P-wave axis (°) | 56 ± 22.7 | 47 ± 21.7 | <0.001 |
| QRS axis (°) | 82 ± 18.1 | 73 ± 16.7 | <0.001 |
| Qtc (ms) | 392 ± 17.7 | 398 ± 40.5 | Not significant |

| Table 2. Number of patients with electrocardiographic abnormalities in the restricting-type anorexia nervosa group and control group | ||
|---|---|---|
| Cases (n = 98) | Controls (n = 98) | |
| Bradycardia (FC <60 bpm) | 59 | 17 |
| Short PR (<120 ms) | 11 | 7 |
| Prolonged PR (>200 ms) | 1 | 0 |
| Narrow QRS (<80 ms) | 11 | 8 |
| Wide QRS (>120 ms) | 1 | 0 |
| Short QTc (<350 ms) | 1 | 0 |
| Prolonged QTc (>450 ms) | 1 | 0 |
| Repolarization changes | 21 | 0 |

Bradycardia was the most frequent finding in patients with anorexia nervosa, found in up to 60%. Table 3 presents the distribution of patients with bradycardia in each group by HR ranges. There were also changes in repolarization in 21 of the patients with RTAN, with ST segment depression in 1 patient, nonspecific ST segment and T-wave (ST-T) changes in 4, and nonspecific T-wave changes in 16. We did not find such changes in the control group.
| Table 3. Distribution of patients with bradycardia (HR <60 bpm) in the group of patients with anorexia nervosa y and the control group | ||
|---|---|---|
| Cases (n = 98) | Controls (n = 98) | |
| HR: 50-60 bpm | 24 (24.5%) | 16 (16.5%) |
| HR: 40-50 bpm | 28 (28.5%) | 1 (1.5%) |
| HR: 30-40 bpm | 7 (7.5%) | 0 |

In addition, the left ventricular mass, thickness and diameter were significantly smaller in patients with RTAN (Table 4).
| Table 4. Echocardiographic measurements in female adolescents with anorexia nervosa and in the control group | |||
|---|---|---|---|
| Cases (mean ± SD) | Controls (mean ± SD) | p-value | |
| LV thickness (mm) | 5.7 ± 0.7 | 6.8 ± 0.7 | <0.001 |
| LV diameter (mm) | 41.6 ± 3.5 | 44.6 ± 3.2 | <0.001 |
| LV mass (g/m2) | 65.7 ± 14.8 | 90 ± 15.3 | <0.001 |

We did not find abnormalities in laboratory tests results, including electrolyte levels, in any of the patients.
We did not find an association of HR with weight (r = -0.20; p = 0.05) or BMI (r = 0.0162; p = 0.22) at admission in patients with RTAN (Fig. 1). However, we did find that the left ventricular mass was significantly correlated to BMI (r = 0.20; p < 0.001 (Fig. 2) and HR (r = -0.22; p < 0.001).
| Figure 1. Correlation of heart rate and body mass index in female adolescents hospitalised due to anorexia nervosa (r = -0.016; p = 0.22) |
|---|
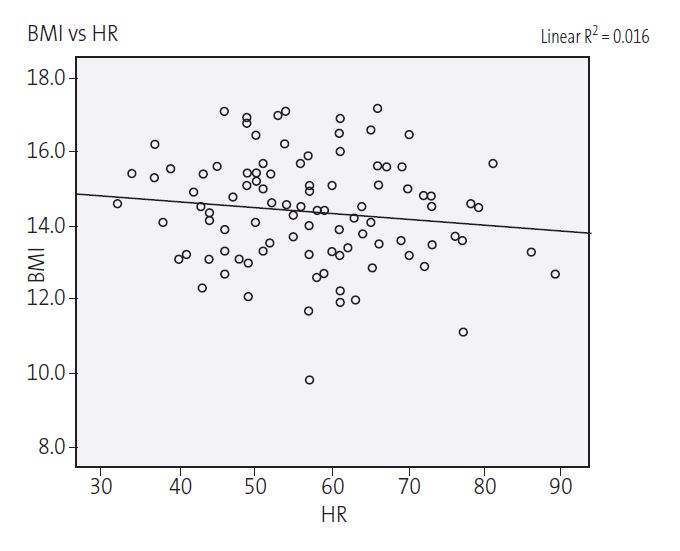 |

| Figure 2. Correlation of left ventricular mass and body mass index in female adolescents hospitalised due to anorexia nervosa (r = 0,20; p <0,001) |
|---|
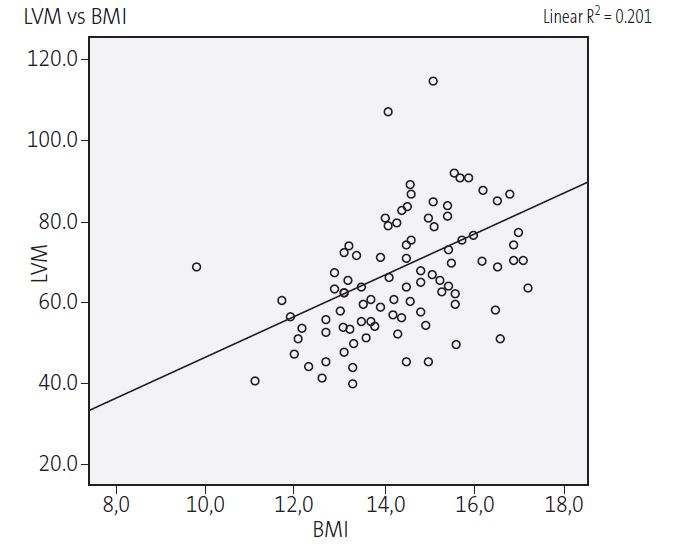 |

DISCUSSION
In our study, electrocardiographic abnormalities were more prevalent in the group of patients with RTAN compared to the control group. The most frequent abnormality was bradycardia, found in more than half of the patients with (60%). The prevalence of relative bradycardia in patients with RTAN varies considerably between studies, with 1 that included hospitalised patients subject to a strict diet reporting a prevalence as high as 95%.7 In our case series, bradycardia was an independent event that was not associated with the weight or the BMI at admission.
There is a years-long controversy in the medical literature on the indicators of life-threatening severity in anorexia nervosa that may call for hospital admission or closer clinical monitoring. The heart rate has been analysed in various studies, as sinus bradycardia has been previously described as a clinically relevant marker of severity.8,23-27
Changes in the PR segment were slightly more frequent in the anorexia nervosa group (both short PR and prolonged PR). Changes in the QRS complex were also more frequent in patients with RTAN. We did not find significant differences between cases and controls in the prevalence of prolonged QTc. This feature was only found in 1 patient in our study. In the case group, only 2 patients had changes in the QT interval: short QT interval in 1 and prolonged QT interval in the other. The blood tests performed before the ECG in both showed electrolyte levels in the normal range. Previous studies have described a high prevalence of long QT interval in adolescents with anorexia nervosa.7,14 However, the data on this association are contradictory and subject of controversy. In this case, the results we obtained could be due to the sample including only patients with RTAN and not with other eating disorders, such as bulimia or binge eating/purging type anorexia in which electrolyte abnormalities and therefore changes in the QTc are more common due to vomiting.
Another salient finding in our study was a lesser amplitude in the R-wave in V6 in cases versus controls, consistent with the results of previous studies,8,28 which is indicative of diminished strength in the left ventricle, a problem that was also reflected by the smaller mass and thickness of the left ventricle in these patients.
A relevant novelty in our study was the analysis of echocardiographic findings, which have not been a subject of study as often in these patients. In our sample, we found a lesser mass and thickness of the left ventricle in patients with anorexia nervosa compared to controls, a finding that makes sense given the loss of muscle mass due to food restriction.
We found a significant correlation between greater severity of disease (as indicated by a lower BMI) and lesser left ventricular mass. The latter was also significantly correlated to a lower heart rate. However, we did not find a correlation between BMI and heart rate. This suggests that it may be worth considering additional objective prognostic factors for this disease based on the echocardiographic examination.
Certain abnormal laboratory test results, especially changes in electrolyte levels, have been described as being more frequent in patients with eating disorders and as potential causes of cardiovascular complications found in these patients.29 In our study, we only analysed electrolyte serum levels, and we did not find any abnormalities in any of the patients. None of the patients had severe cardiac complications during their hospital stay.
The main limitations of our study are its retrospective data collection and not having included other eating disorders such as bulimia nervosa or unspecified eating disorders, as comparative studies have described a higher prevalence of these changes in patients with anorexia nervosa compared to patients with other eating disorders.8 Furthermore, our study focused solely on the electrocardiographic and echocardiographic findings at admission, and did not take into account the potential impact of refeeding or weight recovery or analyse changes in electrocardiographic and echocardiographic findings over the long term.
It would be useful to carry out prospective studies with greater sample sizes and with a medium-to-long-term followup of these patients to assess the normalization of these changes and its association with recovery from the disease.
CONCLUSIONS
In our study, a high number of female adolescents hospitalised due to anorexia nervosa exhibited electrocardiographic and echocardiographic abnormalities. The most prevalent abnormalities in the ECG were sinus bradycardia and ventricular repolarization abnormalities. The most frequent echocardiographic abnormalities were reduced left ventricular mass and reduced mean thickness of the left ventricle.
An understanding of the clinical course of these abnormalities is essential, as is the establishment of a specific long-term follow-up plan.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
BMI: body mass index · BP: arterial blood pressure· DSM-5: Diagnostic and Statistical Manual for Mental Disorders, 5th edition · ECG: electrocardiogram/electrocardiography · HR: heart rate · LV: left ventricle · mV: millivolts · QRS: QRS complex · QT: QT interval · QTc: corrected QT interval · RTAN: restricting type anorexia nervosa · ST: ST interval.
REFERENCES
- American Psychiatric Association. Manual Diagnóstico y Estadístico de los Trastornos Mentales (5th edition). Arlington: American Psychiatric Publishing; 2013.
- American Psychiatric Association. Practice guidelines for eating disorders. Am J Psychiatry. 1993;150:212-28.
- Zenker J, Hagenah U, Rossaint R. Anesthesia in patients with anorexia nervosa and bulimia nervosa. Der Anaesthesist. 2010;59:261-72.
- Papadopoulos FC, Ekbom A, Brandt L, Ekselius L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. Br J Psychiatry. 2009;194:10-7.
- Olivares JL, Vázquez M. Alteraciones cardiológicas, potencialmente letales, en adolescentes con anorexia nerviosa. Rev Esp Pediatr. 2004,60:91-4.
- Thurston J, Marks P. Electrocardiographic abnormalities in patients with anorexia nervosa. Br Heart J. 1974;36:719-23.
- Palla B, Litt IF. Medical complications of eating disorders in adolescents. Pediatrics. 1988;81:613-23.
- Panagiotopoulos C, McCrindle BW, Hick K, Katzman DK. Electrocardiographic findings in adolescents with eating disorders. Pediatrics. 2000;105:1100-5.
- Nussinovitch M, Gur E, Nussinovitch N, Kaminer K, Volovitz B, Nussinovitch U. Medically treated anorexia nervosa is associated with normal P wave parameters. Psychiatry Res. 2012;198:259-62.
- Vanderdonckt O, Lambert M, Montero MC, Boland B, Brohet C. The 12-lead electrocardiogram in anorexia nervosa: A report of 2 cases followed by a retrospective study. J Electrocardiol. 2001;34:233-42.
- Cooke RA, Chambers JB, Singh R, Todd GJ, Smeeton NC, Treasure J, et al. QT interval in anorexia nervosa. Br Heart J. 1994;72:69-73.
- Galleta F, Franzoni F, Cupisti A, Belliti D, Prattichizzo F, Rolla M. QT interval dispersion in young women with anorexia nervosa. J Pediatr. 2002;140:456-60.
- Nahshoni E, Weizman A, Yaroslavsky A, Toledano A, Sulkes J, Stein D. Alterations in QT dispersion in the surface electrocardiogram of female adolescents diagnosed with restricting-type anorexia nervosa. J Psychosom Res. 2007;62:469-72.
- Durakovic Z, Durakovic A, Korsic M. Changes of the corrected Q-T interval in the electrocardiogram of patients with anorexia nervosa. Int J Cardiol. 1994;45:115-20.
- Sachs KV, Harnke B, Mehler PS, Krantz MJ. Cardiovascular complications of Anorexia Nervosa: a systematic review. Int J Eat Disord. 2016;49:238-48.
- Vargas Upegui C, Gómez J. Alteraciones electrocardiográficas en anorexia nervosa: revisión crítica de la literatura. Rev Colomb Psiquiat. 2015;44:33-40.
- Lesinskiene S, Barkus A, Ranceva N, Dembinskas A. A meta-analysis of heart rate and QT interval alteration in anorexia nervosa. World J Biol Psychiatry. 2008;9:86-91.
- Mont L, Castro J, Herreros B, Pare C, Azqueta M, Magrina J, et al. Reversibility of cardiac abnormalities in adolescents with anorexia nervosa after weight recovery. J Am Acad Child Adolesc Psychiatry. 2003;42:808-13.
- Ulger Z, Gurses D, Ozyurek AR, Arikan C, Levent E, Aydogdu S. Follow-up of cardiac abnormalities in female adolescents with anorexia nervosa after refeeding. Acta Cardiol. 2006;61:43-9.
- Roche F, Barthélémy JC, Mayaud N, Pichot V, Duverney D, Germain N, et al. Refeeding normalizes the QT rate dependence of female anorexic patients. Am J Cardiol. 2005;95:277-80.
- Yoshida N, Yoshiuchi K, Kumano H, Sasaki T, Kuboki T. Changes in heart rate with reffeding in anorexia nervosa: a pilot study. J Psychosom Res. 2006;61:571-5.
- Guerrero-Vázquez R, Olivares-Gamero J, Pereira-Cunilla JL, Soto-Moreno A, García-Luna PP. Nutrición en anorexia nerviosa. Endocrinol Nutr. 2006;53:113-23.
- Vázquez M, Olivares JL, Fleta J, Lacambra I, González M. Alteraciones cardiológicas en mujeres adolescentes con anorexia nerviosa. Rev Esp Cardiol. 2003;56:669-73.
- Mont L, Castro J. Anorexia nerviosa: una enfermedad con repercusiones cardiacas potencialmente letales. Rev Esp Cardiol. 2003;56:652-3.
- Shamim T, Golden NH, Arden M, Filiberto L, Shenker IR. Resolution of vital sign instability: an objective measure of medical stability in anorexia nervosa. J Adolesc Health. 2003;32:73.
- Portilla MG. Bradycardia: an important physical finding in anorexia nervosa. J Ark Med Soc. 2011;107:206-8.
- Yahalom M, Spitz M, Sandler L, Heno N, Roguin N, Turgeman Y. The significance of bradycardia in anorexia nervosa. Int J Angiol. 2013;22:83-94.
- Moodie DS, Salcedo E. Cardiac function in adolescents and young adults with anorexia nervosa. J Adolesc Health Care. 1983;4:9-14.
- Facchini M, Sala L, Malfatto G, Bragato R, Redaelli G, Invitti C. Low-K+ dependent QT prolongation and risk for ventricular arrhytmia in anorexia nervosa. Int J Cardiol. 2006;106:170-6.






