Vol. 20 - Num. 79
Original Papers
Severe neonatal hypernatremic dehydratation in the initiation of the breastfeeding: study of incidence and associated factors
David López Martína, M.ª Mar Alonso Montejob, José Miguel Ramos Fernándeza, Ana M.ª Cordón Martíneza, Tomás Sánchez Tamayoc, Antonio Luis Urda Cardonaa
aUGC de Pediatría. Hospital Materno-Infantil de Málaga. Hospital Regional Universitario de Málaga. Málaga. España.
bMIR-Pediatría. Hospital Materno Infantil de Málaga. Málaga. España.
cUGC de Neonatología. Hospital Materno-Infantil de Málaga. Hospital Regional Universitario de Málaga. Málaga. España.
Correspondence: D López. E-mail: lopez.martin.david@hotmail.com
Reference of this article: López Martín D, Alonso Montejo MM, Ramos Fernández JM, Cordón Martínez AM, Sánchez Tamayo T, Urda Cardona AL. Severe neonatal hypernatremic dehydratation in the initiation of the breastfeeding: study of incidence and associated factors. Rev Pediatr Aten Primaria. 2018;20:229-35.
Published in Internet: 10-09-2018 - Visits: 42377
Abstract
Introduction: neonatal hypernatremic dehydration associated with failure in the establishment of breastfeeding instauration can cause significant complications and even death. There are few studies on its incidence in Spain. Objectives: our aim was to determine the incidence of this problem and describe the epidemiological and clinical features associated with it.
Materials and methods: we conducted a retrospective observational study in newborns with a diagnosis of hypernatremic dehydration and serum sodium levels of more than 150 mEq/l that required hospitalization between 2011 and 2017 in our catchment area. We excluded patients with underlying conditions or concomitant infection. We collected data on epidemiological, clinical, laboratory, treatment and outcome variables through the review of health records, followed by their statistical analysis.
Results: the estimated size of the susceptible population was 41 084 newborns. Twenty met the inclusion criteria. In this sample, 19/20 newborns were exclusively breastfed, 14/20 were the first-born child, and the median maternal age was 34 years (interquartile range: 31-37). The most frequent reasons for seeking care were weight loss, jaundice and irritability. The median age at admission was 5.5 days (interquartile range: 3.3-9.8), the percentage of birth weight lost was 14.4% (interquartile range: 10-17), and the median serum sodium level was 157.25 mEq/l (interquartile range: 152-157.8). The mean length of stay was 6.5 days (interquartile range: 4-8.75), and 2/20 newborns required intensive care. None of the patients died or had severe complications.
Conclusions: we found an overall incidence of hypernatremic dehydration of 0.5 per 1000 live births per year in the population under study. We found an association with exclusive breastfeeding, primiparity and greater maternal age. In light of these results, it seems advisable to provide information on the warning signs at the time of discharge from the maternity ward, and to schedule the first checkup for the baby at an earlier time.
Keywords
● Breastfeeding ● Dehydration ● Hypernatremia ● NewbornINTRODUCTION
Hypernatremic dehydration (HND) in exclusively breastfed newborns (NBs) is a health problem that started being featured in the literature in the 1990s. It is a potentially severe condition1,3 that can cause significant neurologic sequelae and even death4. Although the actual incidence of HND in Spain is unknown, it is considered a significant public health problem due to its repercussions; the estimated incidence is 1.7 to 5 per 1000 live births2,5.
Hypernatremic dehydration is defined as a serum sodium level of 150 mmol/l or higher, and it may be associated with weight loss in excess of what is expected physiologically (10%)4,6. Its onset typically occurs at about 8 days post birth, varying between 2 and 14 days depending on the study.
This condition is underdiagnosed, as it presents with nonspecific symptoms such as lethargy, although some patients become irritable instead. Furthermore, the baby may show signs of dehydration (such as dry mucous membranes, a sunken fontanel, poor skin turgor), a malnourished appearance, jaundice, fever, oliguria or anuria or neurologic abnormalities.
The risk factors for HND described in the literature include inadequate feeding of NBs (poor breastfeeding [BF] technique, poor sucking or low milk supply), preterm birth, small for gestational age or low birth weight, maternal primiparity, caesarean delivery, or failure of mothers to identify signs of inadequate feeding early on4,7-10. A reduced daily urine output (less than 6 diaper changes), less than four bowel movements a day after day 4 post birth, the presence of urate crystals in the diaper after day 3 post birth, hyperbilirubinemia and a weight loss of more than 10% of the birth weight are predictors of a poor outcome11.
Some authors have found an association between HND and high sodium concentrations in the breast milk of mothers that have difficulty BF, with absence of the physiological reduction in the concentration of this electrolyte2,12.
The aim of our study was to determine the incidence of hospital admission due to severe HND and to describe the associated risk factors for the purpose of proposing preventive measures.
MATERIALS AND METHODS
We conducted a retrospective descriptive study of patients aged less than 30 days admitted to our referral hospital between January 2011 and December 2016 with a diagnosis of hypernatremic dehydration (serum sodium level ≥150 mmol/l). We included healthy NBs that had been delivered at term (37-42 weeks’ gestational age), with a chronological age of less than 30 days, discharged home after birth and that required admission to hospital, who belonged to the catchment population of our hospital.
We excluded patients born preterm, with concomitant infectious disease, with underlying disease or who died of unknown causes during the study. We retrieved the data from the health records of NBs admitted to our hospital.
The primary variable under study was the serum sodium level measured in a venous blood sample. Other variables we took into account were maternal age, parity, type of delivery, sex, gestational age at birth, chronological age at admission, weight at birth, at admission and at discharge, temperature at admission, type of feeding, presence of clinical signs of dehydration, creatinine, blood urea nitrogen (BUN) and urea levels at admission, serum glucose level at admission, referral to our hospital, previous assessment by another health professional, length of stay in days, admission to the paediatric intensive care unit (PICU), need for additional diagnostic tests, presence of complications, comorbidity and mortality.
We also categorised the reason parents sought care in our hospital based on the presenting symptoms: jaundice, irritability, somnolence, absence of bowel movements in 24 hours, fever, refusal to feed, presence of urate crystals in urine, number of diaper changes per day and weight loss. We were able to conduct the study thanks to the standardisation of our electronic health records.
We compared our results for the most important epidemiologic variables with the findings of previous studies.
We performed the statistical analysis defining significance as a p-value of less than 0.05. We have summarised qualitative variables as frequencies with confidence intervals, and quantitative variables as medians with the corresponding interquartile range.
We used the recorded population for our catchment area as the susceptible population for the purpose of calculating the incidence of HND. We compared differences in the incidence between the warm seasons (spring and summer) and the cold seasons (autumn and winter) by means of the Student t test.
The study adhered to the principles of our hospital’s ethics board. We preserved confidentiality by anonymising the data retrieved from health records.
RESULTS
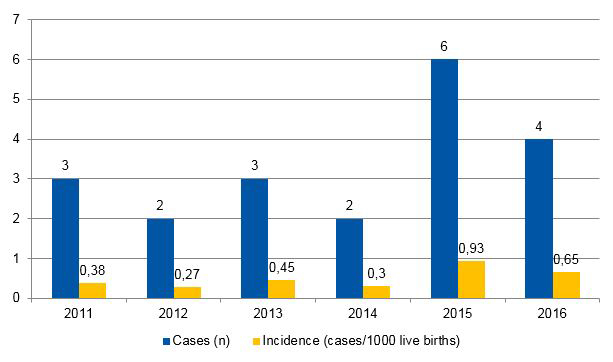
We estimated the size of the susceptible population during the period under study at 41 084 newborns, which corresponded to the newborns delivered in the maternity departments of one secondary level hospital and one tertiary level hospital that are both part of the public health system in the catchment area of our sample. Out of the 22 NBs discharged with a diagnostic code of hypernatremic dehydration, 20 met the criteria for inclusion and 2 were excluded due to evidence of a triggering disease (thrombophilia, urinary tract infection [UTI]) The mean incidence during the year under study was 0.5 per 1000 live births per year, and Figure 1, shows the incidence by year, with the maximum in 2015 (0.93 per 1000 live births/year) and the minimum in 2012 (0.27 per 1000 live births/year).
Table 1 summarises the demographic and clinical characteristic of the newborns and their mothers. The sample included 11 girls (55%) and 9 boys (45%). Eight cases (40%) presented during the spring/summer, and 12 (60%) in autumn/winter, a difference that was not statistically significant (p = .371).The mean gestational age at birth was 39.1 weeks (standard deviation [SD] ±1.11) and the mean birth weight was 3272 g (SD ±373.3). Two of the newborns were delivered by caesarean section, one due to nonreassuring foetal heart rate tracings and the other due to prolonged labour. All 20 NBs (100%) had Apgar scores of 9-10 at 5 and 10 minutes post birth. Newborns were discharged from the maternity ward between the 2nd and 3rd day post birth in 18 cases (90%), and none were discharged early (at 24 hours post birth). Of all patients, 14 were the first-born child (70% of mothers were primiparous), and the median maternal age in our sample was 34 years (interquartile range [IQR]: 31-37). Most NBs (19; 95%) were exclusively breastfed—one of the mothers had unilateral mastitis at the time her child was admitted—and breast milk was fortified from birth in only 1 case by parental choice.
Five of the babies (25%) were referred after previous assessment, in 3 cases by their paediatricians, in 1 case by a midwife and in 1 case by the emergency team. In the remaining cases, the family visited the emergency department in our hospital of their own initiative. The presenting complaints are summarised in Table 1: the most frequent reasons for seeking care were jaundice—in 4 cases (20%) requiring phototherapy—and irritability with inconsolable crying, followed by somnolence, absence of bowel movements in 24 hours, fever and excessive weight loss or failure to regain the birth weight. Other, less frequent reasons to seek care were refusal to feed and appearance of urate crystals in the diaper. The median age at admission was 5.5 days (IQR: 3.3-9.8), and the median number of diaper changes was 3 a day (IQR: 2-4). The median percentage of weight loss relative to the birth weight was 14.4% (IQR: 10-17). During the initial evaluation, 11 of the patients (55%) exhibited sucking that was ineffective, slow or lazy.
| Table 1. Maternal and newborn characteristics (n = 20) in cases of neonatal hypernatremic dehydration associated with breastfeeding | |||
|---|---|---|---|
| Variable (unit of measurement) | Median | Interquartile range | Range |
| Age at admission (days) | 5,5 | 3,3-9,8 | 2-15 |
| Number of wet diapers/day | 3 | 2-4 | 0-6 |
| Number of bowel movements/day | 1 | 0-1 | 0-4 |
| Weight loss (%)) | 14,4 | 10-17 |
5,9-30 |
| Serum sodium level (mEq/l) | 155 | 152-157,8 | 150-178 |
| Maternal age (years) | 34< | 31-37 | 19-47 |
| Variable (unit of measurement) | Mean | Standard deviation | |
| Mean birth weight (grams)) | 3272,3 | ±373,3 | |
| Mean gestational age (weeks) | 39,1 | ±1,11 | |
| Variable | Absolute frequency | ||
| Female newborn | 11 | ||
| Exclusive breastfeeding | 19 | ||
| Poor sucking | 11 | ||
| Uncomplicated delivery | 18 | ||
| Primiparous mother | 14 | ||
| Maternal mastitis | 1 | ||
| Admission during the cold-weather season |
12 |
||
| Presenting complaint at admission (n = 20) | |||
| Irritability | 9 | ||
| Jaundice | 9 | ||
| Somnolence | 8 | ||
| Absence of stools in 24 hours | 8 | ||
| Fever | 7 | ||
| Weight loss | 6 | ||
| Refusal to feed | 4 | ||
| Urate crystals in urine | 4 | ||

The median serum sodium level was 157.25 mEq/l (IQR: 152-157.8). Twelve patients (60%) had mild metabolic acidosis, and the median blood pH in the overall sample was 7.34 (IQR: 7.29-7.35). Five patients (25%) had hypoglycaemia, and the median blood glucose level in the overall sample was 65 mg/dl (IQR: 53-82). The medium serum creatine level in our sample was 0.62 mg/dl (IQR: 0.53-0.73). A head ultrasound was performed in 12 NBs (60%), due to excessive somnolence (in 7 of the patients) or irritability (in 5), with abnormal findings in only 1, whose scan revealed mild bilateral hyperechogenicity in the basal nuclei, suggestive of possible oedema; although a follow-up ultrasound was not performed, the neurologic outcome of this patient was favourable. Table 2 summarises the findings of other diagnostic tests..
| Table 2. Abnormal findings of diagnostic tests in cases of neonatal hypernatremic dehydration associated with breastfeeding (n = 20) | |||
|---|---|---|---|
| Variable | Absolute frequency | ||
| Mild metabolic acidosis | 12 | ||
| Prerenal acute kidney injury | 5 | ||
| Blood glucose <60 mg/dl | 5 | ||
| Abnormalities in head ultrasound | 1 | ||

The mean length of stay was 6.5 days (IQR: 4-8.75), and the median weight at discharge was 3175 g (IQR: 2800-3370). Two newborns required admission in the intensive care unit for 48 hours, one due to a serum sodium level of 178 mEq/l and the other to neurologic involvement with episodes of central apnoea. Sixteen patients (80%) required intravenous fluid therapy, with an average duration until correction of hypernatraemia of 48 hours. None of the patients required renal replacement therapy, and all but 1 were fed a modified artificial formula during their stay, although only the mothers of 13 had a low milk supply (65%). There were no deaths among the patients in our sample.
DISCUSSION
The overall frequency of HND in our sample (0.5 cases per 1000 live births/year) was very similar to the incidence reported in the medical literature. As reference for Spain, the incidence of hypernatremia per 1000 live births found in a study in Asturias was 0.47 between 2002 and 2008 and 0.81 between 2009 and 201513, although the sample in this study consisted of NBs admitted to the neonatal unit, in whom the condition was more likely to be identified. A study in a hospital in Gandía (Valencia) found an incidence of 1.4 per 1000 live births in 2002, with the peak in the study reaching 10.3 in year 200014. In contrast with the improvement in care delivery in other aspects, we did not find a declining trend in incidence in our patients during the period under study, nor in relation to the data from previous studies, which indicates that we need to develop strategies to address this yet unresolved problem.
In our sample, all cases had onset within 15 days from birth, with a median age at admission that was slightly greater compared to the age reported in other case series, which can probably be explained by our study focusing on newborns admitted after discharge from the maternity ward.
The most common reasons care was sought in our case series were, with equal frequency, irritability and jaundice, presenting symptoms that were consistent with the literature, which also describes presentations with hypertonia and hyperreflexia, altered level of consciousness or seizures, which were not observed in any of our patients14,15. As occurred in previously published case series, excessive weight loss from birth was a frequent feature, as was the appearance of urate crystals in the urine14,16-18.
In agreement with the previous literature, we did not find relevant features in the prenatal or perinatal history in our sample of NBs19. Contrary to other studies, we did not find an association with caesarean delivery, as in Spain this intervention usually does not entail a delay of more than 12 hours in BF initiation20. Most mothers in our sample were primiparous, and the median maternal age was 34 years, which was consistent with previous studies where the median ages of the mothers age were 3017 and 34 years,13.
The metabolic comorbidities found in our study were similar to those described in other studies in Spain, with mild acidosis detected in half of our sample, although our patients did not develop the disorders described in other case series while they received treatment to correct the acidosis21,22. We found few instances of seizures or intracranial abnormalities in our series, probably due to the median serum sodium level of 155 mEq/l, which was below the levels reported in other series that described these manifestations13,14.
In our well-child programme, the first check-up visit is scheduled at 15 days post birth, which in our opinion is too late to detect problems derived from inadequate BF in at-risk NBs, as our data imply. The scheduling of a first appointment at the end of the first week of life could help prevent HND associated with BF or at least reduce its incidence, and also support BF, preventing early discontinuation of BF due to inefficient technique or maternal discouragement13. Another possibility would be to schedule a visit to measure the NB on the day that they are brought in for the heel prick test, or to establish education programmes for mothers in maternity wards13,18. Education of health care staff though the development of consensus documents and the implementation of BF support workshops for mothers are measures that succeeded in reducing the incidence of HND in other facilities in Spain13,19.
One of the limitations of our study, which was due to its retrospective design, was that we were unable to obtain data on parental educational attainment. A future prospective study, one which would include an analysis of the impact of the improvement measures proposed here, could be the starting point to decrease the incidence of this health problem.
Our study is the first in Spain to calculate the incidence of HND in newborns after discharge, identifying primiparity as a relevant maternal risk factor. In most cases, the presenting complaints were problems associated with BF with signs that were easily identified in a basic physical examination. We believe that BF provides the best nutrition for the infant, but that it requires adequate monitoring, as having the first routine child wellness checkup early on, at day 7 post birth, could help reduce the incidence of lactation failure and HND.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
BF: breastfeeding · BUN: blood urea nitrogen · HND: hypernatremic dehydration · IQR: interquartile range · NB: newborn · PICU: paediatric intensive care unit · SD: standard deviation · UTI: urinary tract infection.
REFERENCES
- Neifert MR. Prevention of breastfeeding tragedies. Pediatr Clin North Am. 2001;48:273-97.
- Ivan Amerongen RH, Moretta AC, Gaeta TJ. Severe hypernatremic dehydration and death in a breast-fed infant. Pediatr Emerg Care. 2001;17:175-80.
- Gebara BM, Everett KO. Dural sinus thrombosis complicating hypernatremic dehydration in a breastfed neonate. Clin Pediatr (Phila). 2001;40:45-8.
- Moritz ML, Manole MD, Bogen DL, Ayus JC. Breastfeeding-associated hypernatremia: are we missing the diagnosis? Pediatrics. 2005;116:343-7.
- Segovia RE. Hiponatremia e hipernatremia. En: Facultad de Medicina, Universidad de Chile [en línea] [consultado el 03/09/2018]. Disponible en basesmedicina.cl/nefrologia/12_3_hiponatremia/inicio.htm
- Oddie S, Richmond S, Coulthard M. Hypernatraemic dehydration and breast feeding: a population study. Arch Dis Child. 2001;85:318-20.
- Laing A, Wong C. Hypernatraemia in the first few days: is the incidence rising? Arch Dis Child Fetal Neonatal. 2002;87:F158-F162.
- Moritz ML, Ayus JC. Disorders of water metabolism in children: hyponatremia and hypernatremia. Pediatr Rev. 2002;23:371-80.
- Asturizaga MA, Mazzi GE. Hipernatremia neonatal: factores de riesgo. Rev Chil Pediatr. 2011;82:150-1.
- Erdeve O, Atasay B, Arsan S. Hypernatraemic dehydration in breastfed infants: is caesarean section a risk? Ann Trop Paediatr. 2005;25:147-8.
- Solá A, León HAP. Balance hidroelectrolítico. En: Docstoc [en línea]. Disponible en docstoc.com/docs/153840669/Balance-Hidroelectrol%C3%ADtico-Neonatal
- Juliao J. Deshidratación hipernatrémica e hiperbilirrubinemia indirecta en el recién nacido a término. Rev Medica Sanitas. 2009;12:34-42.
- González García LG, Carrera García L, Arias Llorente RP, Romero MC, Suárez Rodríguez M, Fernández AI, et al. Deshidratación hipernatrémica asociada a la alimentación con lactancia materna en el periodo neonatal. Acta Pediatr Esp. 2016;74:261-5.
- Peñalver Giner O, Gisbert Mestre J, Casero Soriano J, Bernal Ferrer A, Oltra Benavent M, Tomás Vila M. Deshidratación hipernatrémica asociada a lactancia materna. An Pediatr (Barc). 2004;61:340-3.
- Jonguitud-Aguilar A, Calvillo-Robles S, Ruiz-Martínez E, Olvera-López G. Protocolo de manejo en deshidratación hipernatrémica neonatal. Perinatol Reprod Hum. 2015;29:65-9.
- Fernando C, Álvarez H, Fernando J, Robledo G, López AV. Curso clínico de la deshidratación hepernatrémica en recién nacidos. Arch Investig Matern Infant. 2014;6:52-60.
- Berger-Larrañaga M, Bustamante-Abuid C, Díaz-Vergara S, Tresierra-Cabrera J, Mayta-Tristán P, Segura ER. Trastornos de la lactancia materna y otros factores asociados a la pérdida de peso neonatal excesiva en un hospital de la Seguridad Social en Lima, Perú. Nutr Hosp. 2015;32:2062-70.
- Tofé Valera I, Párraga Aquiles MJ, Ruiz González MD, Huertas Muñoz MD, Guzmán Cabañas JM, Zapatero Martínez M. Deshidratación hipernatrémica en un recién nacido con lactancia materna exclusiva. Vox Peadiatr. 2005;1:39-41.
- Vázquez I, Ferrández MJ, Mendoza MR, Quiles JL. Lactancia materna y deshidratación neonatal. ¿Se puede disminuir el número de casos? Acta Pediatr Esp. 2015;73:e247-e251.
- Lavagno C, Camozzi P, Renzi S, Lava SA, Simonetti GD, Bianchetti MG, et al. Breastfeeding-associated hypernatremia: a systematic review of the literature. J Hum Lact. 2016;32:67-74.
- Albalate Ramon M, Alcazar Arroyo R, de Sequera Ortiz P. Alteraciones del agua y del sodio. En: Nefrología al Día [en línea] [consultado el 03/09/2018]. Disponible en revistanefrologia.com/es-monografias-nefrologia-dia-articulo-alteraciones-del-sodio-del-agua-19
- Jaramillo I, López G, Hernández H. Hypernatremic dehydration and death in an infant. Pediatr Emerg Care. 2003;19:62-3.