Experience in the implementation of the health education programme If it is urgent for you, is it urgent for me?
Marta Esther Vázquez Fernándeza, María Sanz Almazánb, Carlos Ruiz Labargac, Teresa Palencia Ercillad, María Tríguez Garcíae, Susana García Sanzf
aPediatra. CS Arturo Eyries. Facultad de Medicina. Universidad de Valladolid. Valladolid. España.
bMédico de Familia. CS Arturo Eyríes. Valladolid. España.
cPediatra. CS Rondilla. Valladolid. España.
dPediatra. CS de Cuellar. Cuellar. Segovia. España.
ePediatra. CS Eras del Bosque. Palencia. España.
fEnfermera. CS Arturo Eyries. Valladolid. España.
Correspondence: ME Vázquez. E-mail: mvmarvazfer@gmail.com
Reference of this article: Vázquez Fernández ME, Sanz Almazán M, Ruiz Labarga C, Palencia Ercilla T, Tríguez García M, García Sanz S. Experience in the implementation of the health education programme If it is urgent for you, is it urgent for me? Rev Pediatr Aten Primaria. 2018;20:e5-e14.
Published in Internet: 31-01-2018 - Visits: 17928
Abstract
Objective: to analyse our experience in the implementation of a health education programme in the Primary Care Paediatrics setting.
Materials and methods: observational and retrospective study. Setting: five primary care centres in urban and semi-urban areas. Participants: pregnant women in the third trimester of gestation and their partners. We held six 90-minute workshops: one on the appropriate use of paediatric emergency services and another five on the management of the most common health problems in children: fever, acute respiratory tract infections (ARTIs), acute gastroenteritis (AGE), skin lesions and traumatic injuries, burns and sprains. We analysed epidemiological data, the baseline level of knowledge, attendance and degree of satisfaction with the intervention.
Results: of the total universe of pregnant women, 44.21% attended the workshops. Women attended more frequently than their male partners. Most women were primiparous, had attended university, were currently employed and of Spanish nationality. Their mean age was 34.53 years. We found greater gaps in knowledge in attendees that were going to be parents for the first time, aged less than 30 years, without a college education and receiving care in specific primary care centres. The workshops with the highest attendance were those on fever and respiratory tract infections. The workshops were designed to be entertaining and interactive. Participants reported a high level of satisfaction and gave positive feedback.
Conclusions: we propose the use of this type of programmes to better prepare parents-to-be to manage potential health problems in their children and make appropriate use of health care services.
Keywords
● Health education ● Knowledge ● Patient satisfaction ● Pregnant women ● Primary health careINTRODUCTION
In the public health care system of Spain, paediatrics services receive a high volume of visits, but most of them are made for mild health problems, especially self-limiting diseases that do not require diagnostic tests or even treatment.1 In the past few decades, paediatric health care has come to encompass any situation that in the opinion of parents, relatives or the patients themselves requires immediate attention, even if it is not actually an emergency.2 The likely consequences of this situation include delays in the care of those patients that actually do need it, a lack of time to develop health prevention and promotion activities, stressful and frustrating conditions for health care workers and escalating health care costs.
This is a difficult problem to tackle. Various approaches have been proposed to address the situation: health education interventions,3,4 coordination of health care services,5 triage systems,6 telephonic consultations and messages,7,8 use of mobile applications9 and other digital tools (web pages, blogs, etc).10 However, the impact on health care of these interventions remains unclear. There are significant gaps in our knowledge of their long-term impact, quality and limitations. We need larger studies with better designs to obtain further data.
The aim of this study was to describe our experience in implementing a group-based health education programme (HEP) called Si es urgente para ti, ¿es urgente para mí? (If it is urgent for you, is it urgent for me?).11 This program targets potential users of paediatric services (future parents) to encourage appropriate use of these services. The materials used in the programme are available in the website of the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics).
MATERIALS AND METHODS
We conducted an observational descriptive study based on the data collected during the implementation of the programme over a 6-month period, from October 2016 to March 2017. The universe consisted of 294 women in the third trimester of gestation (starting from 26 weeks) included in the caseloads of 5 urban and semi-urban primary care centres (PCCs) and their partners. Participants were selected by convenience sampling of consecutive patients by the midwives of participating PCCs until the desired sample size was reached. Information on the programme was provided through individual conversations and posters attached to the doors of the midwives’ offices.
The programme consisted of six 90-minute sessions or workshops: one on the appropriate use of paediatric emergency departments, and five on the management of the most frequent health problems encountered in children—fever, acute respiratory tract infections (ARTIs), acute gastroenteritis (AGE), skin lesions and traumatic injuries, wounds, burns and sprains. The sessions took place in the conference rooms of the participating PCCs. Eight paediatricians and three nurses were involved in the programme. The workshops were offered in morning sessions running from 9:00 to 10:30 or 12:00 a 13:30, and in evening sessions from 17:00 to 18:30,
The If it is urgent for you, is it urgent for me? programme applies a group-based interactive approach and consists of structured activities and contents (chronograms). Table 1 presents the objectives of each workshop. The programme applies different dynamics or techniques: in-class exploration (to express and analyse ideas, beliefs and experiences: brainstorming, picture-word association, questionnaires, Phillips 66), exposition (to increase knowledge: videos, PowerPoint® presentations, texts, printed handouts), situation analysis (to identify challenges and seek possible solutions: analysis of case studies, texts, videos) and skill building (rehearsal: role playing, games, demonstrations, exercises).
| Table 1. Objectives of the workshops included in the If its urgent for you, is it urgent for me? health education programme |
|---|
| Session 1. Appropriate use of Emergency Services |
For participants:
|
| Session 2. Fever |
For participants:
|
| Session 3. Respiratory infections |
For participants:
|
| Session 4. Atopic dermatitis and other skin conditions |
For participants:
|
| Session 5. Gastroenteritis |
For participants:
|
| Session 6. Traumatic injuries, wounds, burns and sprains |
For participants:
|

The variables and questionnaires analysed in the study were:
- Basic sociodemographic characteristics of workshop participants: age, sex, current number of children, educational attainment, employment status, nationality.
- Baseline knowledge: six questions related to the subjects covered in the workshops, one per educational unit (Table 2).
- Attendance to workshops.
- Level of satisfaction with each workshop: 10 questions with answers on a scale of 1-10 regarding the contents, usefulness, and structure of the workshop; 2 open-ended questions asking which subjects felt most relevant and for suggestions.
| Table 2. Baseline knowledge questionnaire administered to the parents that attended the workshops |
|---|
| 1. Mark the correct answer regarding public health services: |
|
| 2. Which do you think is the correct course of action when a child has a fever?: |
|
| 3. Select the wrong statement concerning respiratory tract infections: |
|
| 4. Gastroenteritis episodes: |
|
| 5. Which of the following statements is false?: |
|
| 6. Children frequently have accidents. Select what should not be done to treat a wound: |
|

We created an Excel database for data collection. The statistical analysis was performed with the software SPSS® version 15.0 (SPSS Inc; 1989-2006). We described normally distributed quantitative variables as mean ± standard deviation (SD), and qualitative variables as absolute and relative frequencies (percentages). We analysed the association between variables by means of the χ2 or Fisher exact test or with the likelihood ratio. We compared means using the Student t or the Mann-Whitney U test. We defined statistical significance as p ≤0.05.
The study was approved by the Clinical Research Ethics of the Hospital Universitario Río Hortega and the Valladolid Oeste Health Area. We obtained the written informed consent of all participants.
RESULTS
A total of 154 participants attended the workshops: 130 pregnant women (44.21% of the study population) and 24 fathers-to-be (8.16%). We did not collect data on the reasons why the remaining pregnant women did not participate. The mean age of the parents was 34.76 years (SD: 3.95; 36.66 years in fathers vs. 34. 53 in mothers). The distribution by age groups was: <30 years, 9.13%; 30-35 years, 40.08%; 36-40 years, 39.28%; >40 years, 11.5%. Of all participants, 62.3% were going to have their first child, 33.8% their second, and 3.8% had 2 or more previous children. Of all pregnant women, 74.6% were currently employed, 18.5% unemployed, 4.6% were homemakers and 2.3% were students; while 98.4% of the fathers were employed and 1.6% unemployed. The sample was predominantly of Spanish nationality: 94.6% of mothers and 98.4% of fathers were Spanish.
The distribution by PCC was the following: PCC1, 42.3%; PCC2, 23.8%; PCC3, 13.8%; PCC4, 16.9% and PCC5, 3.2%. The sociodemographic characteristics of the patients were very similar in each PCC, with no statistically significant differences in age, number of children, educational attainment, employment status or nationality.
As to the questionnaire used to assess baseline knowledge before the workshops, the question that was answered correctly most frequently was the one pertaining to fever (88.7%), and the one answered correctly least frequently was the one regarding the use of health care services (13.6%). We did not find significant differences in the answers between mothers and fathers. Of all participants, 68.8% answered three or more questions correctly. Only 5 pregnant women answered all correctly (Table 3).
Table 3. Baseline knowledge in pregnant women and their partners |
|||
|---|---|---|---|
| Total (%) | Mothers | Fathers | |
| Question 1. AUES | A: 32 (20.8) B: 4 (2.6) C: 21 (13.6) D: 88 (57.1) NA or invalid: 9 (5.8) |
A: 27 (20.8) B: 3 (2.3) C: 19 (14.6) D: 73 (56.6) NA or invalid: 8 (6.2) |
A: 5 (20.8) B: 1 (4.2) C: 2 (8.3) D: 15 (62.5) NA or invalid: 1 (4.2) |
| Question 2. Fever | A: 2 (1.3) B: 135 (88.7) C: 11 (7.1) D: 0 NA or invalid: 6 (3.9) |
A: 2 (1.5) B: 112 (86.2) C: 10 (7.7) D: 0 NA or invalid: 6 (4.6) |
A: 0 B: 23 (95.8) C: 1 (4.2) D: 0 NA or invalid: 0 |
| Question 3. ARTIs | A: 37 (24.0) B: 30 (19.5) C: 46 (29.9) D: 31 (20.1) NA or invalid: 10 (6.5) |
A: 30 (23.1) B: 27 (20.8) C: 40 (30.8) D: 23 (17.7) NA or invalid: 10 (7.7) |
A: 7 (29.2) B: 3 (12.5) C: 6 (25) D: 8 (33.3) NA or invalid: 0 |
| Question 4. AGE | A: 92 (59.7) B: 22 (14.3) C: 32 (20.8) D: 1 (0.6) NA or invalid: 7 (4.5) |
A: 78 (60.0) B: 17 (13.1) C: 27 (20.8) D: 1 (0.8) NA or invalid: 7 (5.4) |
A: 14 (58.3) B: 5 (20.8) C: 5 (20.8) D: 0 NA or invalid: 0 |
| Question 5. Skin | A: 10 (6.5) B: 23 (14.9) C: 106 (68.8) D: 9 (5.8) NA or invalid: 6 (3.9) |
A: 9 (6.9) B: 21 (16.2) C: 87 (66.9) D: 7 (5.4) NA or invalid: 6 (4.6) |
A: 1 (4.2) B: 3 (12.5) C: 18 (75) D: 2 (8.3) NA or invalid: 0 |
| Question 6. Accidents | A: 26 (16.9) B: 24 (15.6) C: 7 (4.5) D: 85 (55.2) NA or invalid: 12 (7.8) |
A: 22 (16.9) B: 17 (13.1) C: 6 (4.6) D: 76 (58.5) NA or invalid: 9 (6.9) |
A: 5 (20.8) B: 7 (29.2) C: 1 (4.2) D: 9 (37.5) NA or invalid: 2 (3.3) |
| Total correct answers | 0: 6 (3.9) 1: 6 (3.9) 2: 37 (24) 3: 45 (29.2) 4: 35 (22.7) 5: 20 (13.0) 6: 5 (3.2) |
0: 6 (4.6) 1: 6 (4.6) 2: 29 (22.3) 3: 37 (28.5) 4: 28 (21.5) 5: 19 (14.6) 6: 5 (3.8) |
0: 0 1: 0 2: 8 (33.3) 3: 9 (37.5) 4: 6 (25) 5: 1 (4.2) 6: 0 |

Several sociodemographic variables were associated with the number of correct answers (number of children, PCC, educational attainment and age). Thus, 78.3% of parents that had 1 previous child and 100% of parents with 2 or more children answered 3 or more questions correctly, compared to 62.1% of first-time parents (P = .020). More than 67% of the parents in each PCC answered 3 or more questions correctly except in PCC4, where this percentage was of only 50%, although this difference was not statistically significant. All the parents that answered every question correctly had a college education, as did 75% of the parents that answered 5 correctly and 60% of the parents that answered 4 correctly (P = .040). Of the pregnant women aged less than 30 years, 61.1% answered fewer than 3 questions correctly, while mothers in all other age groups answered more questions correctly (P = .037).
Ten cycles of six workshops each were held. Table 4 summarises attendance, including differences between mothers and fathers, for each workshop and overall. Mothers attended more frequently than fathers, a difference that was statistically significant. The workshop with the highest attendance was the one on fever, followed by the workshop on respiratory tract infections. Of all participants, 70.1% attended three or more workshops and 29.9% all six. Of all mothers, 81.5% attended alone and 18.5% attended at least one of the workshops with their respective partners.
| Table 4. Attendance to workshops | |||||
|---|---|---|---|---|---|
| Mothers | Fathers | Significance (P) | Total | ||
| Attendance per workshop | AUES | 68 (90.2) | 7 (9.8) | .026 | 75 (12.9) |
| Fever | 106 (87.6) | 15 (12.4) | .022 | 121 (20.9) | |
| ARTI | 102 (90.3) | 11 (9.7) | .000 | 113 (19.5) | |
| Skin | 88 (92.6) | 7 (7.4) | .000 | 95 (16.4) | |
| AGE | 90 (88.2) | 12 (11.8) | .039 | 102 (17.6) | |
| Accidents | 67 (90.5) | 7 (9.5) | .031 | 74 (12.7) | |
| Total | 521 (89.8) | 59 (10.2) | .000 | 580 (100) | |
| Number of workshops attended: | 1-2 | 31 (67.4) | 15 (32.6) | .000 | 46 (29.9) |
| 3 or more | 99 (91.7) | 9 (8.3) | .000 | 108 (70.1) | |
| 1 | 11 (8.5) | 11 (45.8) | .000 | 21 (13.7) | |
| 2 | 20 (15.4) | 4 (16.7) | .000 | 23 (15.0) | |
| 3 | 20 (15.4) | 3 (12.5) | .000 | 23 (15.0) | |
| 4 | 16 (12.3) | 5 (20.8) | .000 | 21 (13.7) | |
| 5 | 28 (21.5) | 0 (0.0) | .000 | 29 (19.0) | |
| 6 | 35 (26.9) | 1 (4.2) | .000 | 36 (23.6) | |

Attendance was associated with the number of children (P = .01), and it is worth noting that 75% of participants that attended all 6 workshops were going to be parents for the first time, while 25% had one previous child; none had 2 or more children. The percentage of mothers accompanied by their partners was also higher among first-time parents (91.7% of the women accompanied by their partners vs. 55.7% of the women that attended alone; P = .001).
Another factor that was associated with attendance was the PCC where the mothers received care (P = .002). The mothers that attended 3 or more workshops were in the caseloads of the following primary care centres: CS1, 53 (79.1%); CS2, 27 (79.4%); CS3, 12 (52.2%); CS4, 12(46.2%) and CS5, 5 (100%). We found no statistically significant differences in attendance based on maternal age.
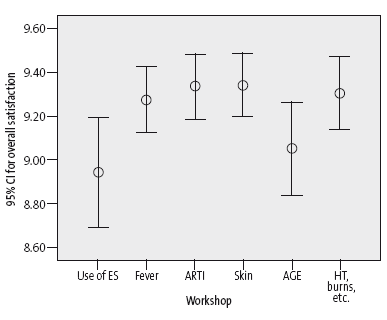
As to the assessment of the satisfaction of participants after each workshop, we collected a total of 580 questionnaires, of which 83.6% (485) were completed by mothers, 11.4% (66) by fathers and 5% (29) by an unspecified parent. Table 5 shows the number of participants per workshop and the mean score given to the items of the satisfaction questionnaire for each workshop. Only one item received a score that was significantly below the mean, which was the one regarding the belief that the workshop would prevent visits to the paediatrician or the emergency room. Another aspect worth noting is that the workshop on the appropriate use of emergency services was the least well received, with a satisfaction rating of less than 9 (Figure 1).
| Table 5. Satisfaction with the workshops | |||||||
|---|---|---|---|---|---|---|---|
| Overall (580) | Workshop 1. AUES (75) | Workshop 2. Fever (121) | Workshop 3. ARTI (113) | Workshop 4. Skin (95) | Workshop 5. AGE (102) | Workshop 6. Accidents (74) | |
| Contents | 9.09 (0.94) | 8.75 (1.04) | 9.12 (0.97) | 9.24 (0.84) | 9.27 (0.79) | 8.87 (1.05) | 9.2 (0.80) |
| Usefulness | 9.25 (0.9) | 8.89 (1.09) | 9.25 (0.95) | 9.36 (0.83) | 9.39 (0.69) | 9.15 (0.95) | 9.39 (0.79) |
| Resolves concerns | 9.06 (1.05) | 8.55 (1.18) | 8.94 (1.15) | 9.25 (0.81) | 9.33 (0.80) | 8.97 (1.21) | 9.25 (0.92) |
| Will prevent visits to emergency room | 8.8 (1.17) | 8.39 (1.28) | 8.75 (1.12) | 8.97 (1.13) | 8.73 (1.2) | 8.73 (1.18) | 9.14 (0.99) |
| Language | 9.41 (0.77) | 9.19 (0.93) | 9.51 (0.68) | 9.51 (0.68) | 9.36 (0.85) | 9.33 (0.80) | 9.49 (0.69) |
| Hand-outs | 9.13 (0.99) | 8.96 (1.04) | 9.08 (1.10) | 9.22 (0.88) | 9.15 (0.91) | 9.01 (1.11) | 9.36 (0.83) |
| Time | 9.05 (1.03) | 8.85 (1.06) | 9.06 (1.03) | 9.17 (0.96) | 9.05 (1.1) | 8.91 (1.16) | 9.20 (0.83) |
| Setting | 9.11 (0.99) | 9.04 (0.99) | 9.04 (1.09) | 9.19 (0.94) | 9.19 (0.98) | 9.02 (0.97) | 9.20 (0.90) |
| Would recommend to others | 9.37 (0.93) | 9.25 (1.17) | 9.40 (0.87) | 9.48 (0.75) | 9.43 (0.72) | 9.21 (1.25) | 9.47 (0.69) |
| Overall satisfaction | 9.22 (0.87) | 8.94 (1.04) | 9.27 (0.8) | 9.33 (0.79) | 9.34 (0.71) | 9.05 (1.06) | 9.30 (0.74) |

| Figure 1. Overall satisfaction with each of the workshops in the programme If it is urgent for you, is it urgent for me? |
|---|
 |

The workshops were very dynamic and interactive. Each included activities performed individually or in small groups that were subsequently discussed by the larger group. Participants rated the workshops highly and made very positive comments. Many of the parents took notes and reported that they had not known many of contents, their questions were answered, and written materials were handed out. Participants expressed the most interest in the following subjects:
- Workshop 1: use of emergency services. Differences between urgency and emergency. Symptoms that require medical care.
- Workshop 2: fever. Fever cut-off points. Management of fever and when to seek emergency care. Febrile seizures.
- Workshop 3: acute respiratory tract infections. Technique for performing nasal lavage in infants.
- Workshop 4: skin. Skin care for atopic dermatitis and infants.
- Workshop 5: acute gastroenteritis. Types of saline solutions. Use of probiotics.
- Workshop 6: wounds, burns, sprains and traumatic injuries. Approach to wounds, burns and head trauma. Wound dressing technique.
DISCUSSION
Our everyday experience in PCCs demonstrates that paediatric patients tend to seek care due to a lack of knowledge on the management of health problems and to psychosocial and emotional factors rather than strictly medical necessity. Paediatrics clinics often manage health problems that are mild or in the early stages: children presenting (without a scheduled appointment) with fever of 20 minutes’ duration, cough in the absence of fever, vomiting and diarrhoea in the context of good general health, a mild skin rash on a hot day, etc.
We are aware that the solution to this unwarranted increase in the demand for health care cannot be a simple one.12 When someone brings in their child or grandchild, it is not just to pass time or to spite us, but because they are facing an overwhelming situation that elicits emotions (fear, uncertainty, anxiety) whose resolution requires professional help. Consequently, we need to develop educational strategies to gradually modify the pattern of utilization of paediatric services.
The HEP that we present here aimed at providing potential users of paediatric services with tools to make appropriate decisions regarding their children’s health. It is based on a combination of health education approaches developed in the past few decades, which are themselves based on the theories of active learning and meaningful learning.13,14 Individuals learn in the framework of their personal experiences, motivations, preconceived ideas and prior knowledge, which are reorganised and modified in the learning process.
The outcomes of health education interventions are heterogeneous. Some studies have found these interventions useful.15 There is evidence that they can succeed, for instance, in promoting physical activity and physical wellbeing in children and adolescents,16 improving health outcomes in disadvantaged populations17 or reducing the prevalence of binge drinking in college students.18 It is also clear that outcomes in certain diseases improve with multimodal approaches.19 Lengths of stay can be reduced by effectively educating parents and children about asthma and its management,3 the prevalence of overweight and obesity in children aged 3 to 5 years can be reduced with combined interventions,20 etc. But the impact of prenatal childbirth education programmes or parent education programmes on postnatal health,10 child safety21 or vaccination coverage rates in early childhood is unclear.22 The studies published to date have concluded that further research with a longer duration of followup is needed.
The HEP presented here targets pregnant women at a stage in their lives when they have more time and motivation. The characteristics of the pregnant women that participated were quite homogeneous: first-time mothers, older age, with a higher education, employed, and of Spanish nationality. We do not know whether this is the actual profile of the pregnant women that receive care in these PCCs or whether our findings are biased due to the non-attendance of mothers with more children, lower educational attainment or different nationality. In our study, we did not know the reason why the rest of the pregnant women chose not to participate (busy with work or household activities, lack of interest, forgetting about the workshops or other personal circumstances).
When it came to the baseline knowledge prior to participation in the workshops, we found the lowest level in parents in their first pregnancy, aged less than 30 years, with an education below college level and managed in specific PCCs. This suggests that it is important for health education programmes to reach these specific subpopulations.
When we analysed the answers, we found that the question answered incorrectly most frequently was the one regarding the use of health care services: more than half of the participants believed that parents visit emergency departments because they are afraid their children have a severe condition (when in fact most of them are actually mild), and one fourth believed that most visits to emergency departments are appropriate. Only a very low percentage knew that health care services constitute a significant economic burden in most countries. Another question that was frequently answered incorrectly was the one regarding respiratory tract infections: many parents-to-be did not know that mucolytic agents and expectorants are not that effective in treating these diseases, an issue that was subsequently addressed during the workshops. There was a fair percentage of correct answers in the rest of the questions.
Another aspect we analysed was attendance. Sex was a clearly influential factor. Significantly fewer fathers attended compared to mothers: are mothers responsible for the health of children? Most of the fathers that attended were going to have their first child. This fact may be explained by a greater lack of knowledge and need for education combined with a greater availability due to the lack of previous children. The workshops that were most attractive to participants were those on fever, respiratory infections and gastroenteritis. The PCC to which mothers were assigned was also a significant factor. This may have been due to the specific birth rate at each PCC at the time of enrolment or to differences in the recruitment skills of specific midwives. We believe that the recruitment process implemented by the midwife is key to the success of the programme.
The level of satisfaction elicited by these workshops was very high for every aspect we analysed. The item rated lowest was the one regarding the workshops succeeding in preventing visits to emergency services or the paediatrician. This demonstrates, on one hand, the anxiety of parents regarding illness in the child, and on the other, their trust in health care services. Although there are aspects of this study that we have yet to analyse, given the existing lack in knowledge, the acceptance of this programme and the intent to improve the use of health care resources, we propose implementing this type of HEPs, as they address the health conditions in children that account for the highest proportions of the total visits.5
CONCLUSIONS
- Parents-to-be, especially first-time parents, are lacking in knowledge and have few skills in the management of the main health problems in children.
- It is important to prioritise the engagement of parents and pregnant women of younger ages, lower socioeconomic status, lower educational attainment and foreign nationality to ensure their participation in this type of educational programmes.
- Participants in this programme reported a very high level of satisfaction and provided positive feedback.
- In order to make sensible decisions concerning health care, individuals must have the necessary knowledge, experience and skills to carry out their responsibilities. Group health education is a tool that could be incorporated in the regular activity of primary care paediatrics.
- We intend to assess the impact of the programme on the number of visits, the level of knowledge and the perception of the medical care received (pre and post intervention).
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
FUNDING
Research Project in Biomedicine 2016, file GRS 1226/B/2016 funded by Sanidad Castilla y León (SACYL).
ABBREVIATIONS
AGE: acute gastroenteritis • ARTI: acute respiratory tract infection • HEP: health education programme • PCC: primary care centre • SD: standard deviation.
REFERENCES
- Ruger JP, Richter CJ, Spitznagel EL, Lewis LM. Analysis of costs, length of stay, and utilization of emergency department services by frequent users: implications for health policy. Acad Emerg Med. 2004;11:1311-7.
- Flores CR. La saturación de los servicios de urgencias: una llamada a la unidad. Emergencias. 2011;23:59-64.
- Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M. Intervenciones educativas para niños en posible visita al servicio de urgencias a causa del asma. Revisión Cochrane traducida. In: Epistemonikos [online] [accessed 24/01/2018]. Available at: https://goo.gl/6Qo7xc
- Gagnon AJ, Sandall J. Individual or group antenatal education for childbirth or parenthood, or both. Cochrane Database Syst Rev. 2007;(3):CD002869.
- Luaces Cubells C. Urgencias pediátricas: dos reflexiones…, dos retos. An Pediatr (Barc). 2017;86:59-60.
- Rivas A, Garrido B. Sistemas de triage hospitalario. In: Míguez MC, Guerrero G, Ignacio MC (eds.). Manual de clasificación y triage del paciente pediátrico en urgencias. Madrid: Ergon; 2015. p. 25-48.
- García de Ribera MC. Consulta telefónica pediátrica urgente en Atención Primaria. Análisis de la implantación de un modelo. Tesis doctoral. Valladolid: Universidad de Valladolid; 2011.
- Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012;12:CD007457.
- García MC, Bachiller MR, Vázquez ME, Barrio MP, del Río AM, Hernández P, et al. Health education through a pediatric mobile phone application. Rev Calid Asist. 2014;29:364-5.
- Vázquez ME, González C, Sanz M, García MM, Ruiz C, Calvo P. La tecnología 2.0 al servicio de la salud materno infantil. Acta Pediatr Esp. 2016;74:e63-5.
- Vázquez ME, Núñez C, Serrano E. Programa de EPS sobre el uso racional de las urgencias pediátrica y actuación ante los principales problemas de salud. ¿Si es Urgente para ti, es urgente para mí? In: Asociación Española de Pediatría de Atención Primaria [online] [accessed 24/01/2018]. Available at https://www.aepap.org/grupos/grupo-de-educacion-para-la-salud/biblioteca/programa-de-eps-sobre-el-uso-racional-de-las-urgencias-pediatricas
- Álvarez de Laviada T, Martínez M, Mínguez R, Sebastián V, Serrano E, Suarez E, et al. Recomendaciones para la atención de urgencias y consultas no demorables en la consulta pediátrica de Atención Primaria. In: Asociación Española de Pediatría de Atención Primaria [online] [accessed 24/01/2018]. Available at https://www.aepap.org/sites/default/files/noticia/archivos-adjuntos/informe_gatpap.pdf
- Pérez MJ, Echauri M, Ancizu E, Chocarro J. Manual de educación para la salud. In: Gobierno de Navarra, Instituto de Salud Pública [online] [accessed 24/01/2018]. Available at https://goo.gl/QWimfA
- Riquelme M. Metodología de educación para la salud. Rev Pediatr Aten Primaria Supl. 2012;14:77-82.
- Nutbean D. Eficacia de la promoción de la salud. In: International Union for Health Promotion and Education. La evidencia de la eficacia de la promoción de la salud. Configurando la salud pública en una nueva Europa. In: Ministerio de Sanidad y Consumo [online] [accessed 24/01/2018]. Available at http://www.msc.es/profesionales/saludPublica/prevPromocion/docs/Parte_2.pdf
- Dobbins M, De Corby K, Robeson P, Husson H, Tirilis D. Intervenciones escolares para promover la actividad física y el buen estado físico en niños y adolescentes. In: Cochrane [online] [accessed 24/01/2018]. Available at http://www.cochrane.org/es/CD007651/intervenciones-escolares-para-promover-la-actividad-fisica-y-el-buen-estado-fisico-en-ninos-y
- O’Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. BMC Public Health. 2015;15:129.
- Bhochhibhoya A, Hayes L, Branscum P, Taylor L. The use of the internet for prevention of binge drinking among the college population: a systematic review of evidence. Alcohol. 2015;50:526-35.
- Flores-Mateo G, Violan-Fors C, Carrillo-Santisteve P, Peiró S, Argimon JM. Effectiveness of organizational interventions to reduce emergency department utilization: a systematic review. PLoS One. 2012;7:e35903.
- Ling J, Robbins LB, Wen F. Interventions to prevent and manage overweight or obesity in preschool children: a systematic review. Int J Nurs Stud. 2016;53:270-89.
- Orton E, Whitehead J, Mhizha-Murira J, Clarkson M, Watson M, Mulvaney C, et al. School-based education programmes for the prevention of unintentional injuries in children and young people. Cochrane Database Syst Rev. 2016;12:CD010246.
- Kaufman J, Synnot A, Ryan R, Hill S, Horey D, Willis N, et al. Face to face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2013;(5):CD010038.






