Vol. 19 - Num. 76
Original Papers
Socio-cultural aspects of breastfeeding older children
José Ignacio Perales Martíneza, Beatriz Pina Marquésb
aPediatra. CS Calatayud Norte. Calatayud. Zaragoza. España.
bMatrona. Hospital Universitario Miguel Servet. Zaragoza. España.
Correspondence: JI Perales. E-mail: josiperales@hotmail.com
Reference of this article: Perales Martínez JI, Pina Marqués B. Socio-cultural aspects of breastfeeding older children. Rev Pediatr Aten Primaria. 2017;19:337-44.
Published in Internet: 25-10-2017 - Visits: 27273
Abstract
Introduction and objectives: breastfeeding beyond 1 year or “extended” breastfeeding is a common practice in many cultures, although rare in Western countries. Our objective was to analyse the experiences of mothers that practice extended breastfeeding from a social perspective.
Materials and methods: survey of 35 mothers that had breastfed or were currently breastfeeding children aged more than 1 year. We explored basic aspects related to this practice. In a second part, we assessed the support received from healthcare professionals, the social perception of extended breastfeeding and the obstacles faced by these mothers.
Results: 60% of mothers were currently breastfeeding, and the mean age of their children was 32.5 months. Most wished to maintain breastfeeding until the child chose to stop. They had all known from the outset that they wanted to breastfeed and would choose this feeding modality again as their preferred option. When concerns arose, their main sources of support were healthcare professionals (58%) and support groups (42%). Up to 65.7% reported getting help from health professionals, with midwives and paediatricians rated as being most supportive. Most mothers reported a high level of satisfaction with extended breastfeeding, but up to 50% had experienced some type of social rejection. Relatives, friends and co-workers had posed barriers at some point that prevented mothers from breastfeeding spontaneously.
Conclusions: these mothers expressed a high degree of satisfaction and confidence. Healthcare professionals play an important role. There are still prejudices in society that pose barriers to this option and limit is widespread practice.
Keywords
● BreastfeedingINTRODUCTION
The benefits of breastfeeding for the mother and child are well known.1 Breastfed children are at lower risk of developing otitis media, respiratory infections, diarrhoea and hypersensitivity reactions. In mothers, breastfeeding helps lose weight, reduces the risk of anaemia and reduces the long-term risk of osteoporosis and breast and ovarian cancers. Overall, it has a significant psychological (reinforcing the mother-child bond), economic and social impact.2 Most studies corroborate these findings, but are limited to infants aged less than 1 year, which could be interpreted as suggesting that breastfeeding is only necessary in early infancy. However, its beneficial effects persist through time and adapt at each stage. Consequently, the leading scientific societies, such as the World Health Organization (WHO), UNICEF, the Asociación Española de Pediatría (Spanish Association of Pediatrics [AEP]) or the American Academy of Pediatrics (AAP), among others, recommend human milk, or breastfeeding (BF), as the sole nutrition in the first 6 months of life, to be continued supplemented with other foods until at least age 12-24 months, and thereafter for as long as the mother and child desire.3-5
Breastfeeding beyond age 12 months or extended breastfeeding (EBF) is a common practice in many cultures, despite it being rare in Western countries. At times, and especially in older children, it attracts attention or is even rejected by society,6 health professionals or even the family.7 The Committee on BF of the AEP has highlighted that the use of the term EBF may lead to confusion, as it may suggest that it involves BF beyond the recommended period. For this reason, some authors choose to use the term BF only, without qualification, with the aim of normalising this practice.
A passage in the 2 Maccabees book of the Bible reads: “My son, have pity on me. Remember that I carried you in my womb for nine months and nursed you for three years. I have taken care of you and looked after all your needs up to the present day.”8 This historical reference serves to illustrate that children have habitually continued to breastfeed past 2 and 3 years of age since the dawn of humanity.
However, the modernization of medicine in the XX century has been associated with a progressive decline in the rates of BF throughout the developed world. Approaches such as the calorimetric method to assess infant nutrition or the development of bacteriological techniques to advance a “clean milk” campaign did nothing but promote feeding with artificial milk substitutes. In 1950, paediatricians recommended the introduction of vegetables in the diet at 4 months of age, which inevitably interfered with BF. To this body of modern medical advice we need to add the emergence of corporate interests, which have also been a strong force in the promotion of “formula” feeding or what in Spain is erroneously referred to as “artificial lactation.” In the United States, for example, contraindications were established for BF, excluding drug users and mothers with evidence of smallpox infection, with the suggestion that wet nursing required “adequate nipples.” These guidelines sometimes included frivolous criteria, such as hair colour. This decline in BF led to the re-emergence of nutritional deficiencies with an associated increase in morbidity, such as scurvy and rickets. Furthermore, the United States census revealed that the mortality rate in breastfed children was 40% lower than that of their formula-fed peers.9
In light of these historical references and aware of the attitude of the majority in today’s society, we set out to carry this study with two main objectives:
- To explore the role of healthcare professionals in BF and their attitude toward supporting and promoting EBF.
- To analyse the socio-cultural perspective of mothers that continue to breastfeed children past infancy. To do so, we assessed the level of personal satisfaction and the difficulties they encountered in different settings of their everyday lives.
MATERIALS AND METHODS
We surveyed 35 women that had breastfed or were currently breastfeeding children aged more than 12 months. The questionnaire consisted of 3 sections:
- Demographic data of the mother: we only collected the age and number of children.
- BF experience: first of all, we explored whether the mothers were still BF as well as past experience with BF. We also asked about how long they had initially planned to breastfeed and how long they intended to maintain BF at present. We then proceeded to explore the personal history of the child the mother was referring to (sex, birth weight, gestational age, type of delivery and history of foetal distress, possibility of skin-to-skin contact after birth and time elapsed until BF was initiated). Other aspects analysed were exclusive BF in the first 6 months of life, co-sleeping, experience with BF during pregnancy or tandem BF.
- Socio-cultural aspects in BF and EBF: experiences of the mothers in their social environment. Where they sought help for questions and/or problems related to BF. Rating of support received from healthcare professionals scored on a scale of 1 to 5. Lastly, social experiences of the mothers associated with EBF in their personal environment. To do so, we asked, among other things, about their level of satisfaction (scale from 1 to 5), whether they had experienced any form of rejection or barrier, or whether they needed to conceal their EBF at some point. Mothers were also asked to rate on a scale of 1 to 5 how they believed their EBF was perceived in different settings in their everyday life.
We obtained a sample of mothers with a similar socio-cultural background, a majority of who were involved in the healthcare field, where there is a high degree of knowledge and acceptance of BF. We submitted the questionnaire by electronic mail and the mothers filled it out individually and anonymously.
We used the software SPSS version 15.0 to collect data and perform a descriptive analysis.
RESULTS
Description of sample and characteristics of the breastfed children
The questionnaire was completed by 35 mothers with a mean age of 34.59 ± 8.41 years (range: 27-48 years). They had a mean number of 1.8 ± 0.93 children. The median age of the children that mothers were referring to in the survey was 32.5 months, with an interquartile range of 14-72.
The most relevant perinatal findings were the following: 65.7% of the children were male. The percentage delivered by caesarean section was 31.4%, while the percentage of uncomplicated births was 58.3%. Of all children, 85.7% were born at term (> 37 weeks). Only 8.5% had a history of foetal distress, and none required advanced cardiopulmonary resuscitation at birth. Breastfeeding was established within 3 hours of birth in 80% (within 1 hour in 54%). We also assessed relevant factors such as skin-to-skin (SSC) contact at birth, exclusive BF in the first 6 months of life and the routine practice of co-sleeping in the first weeks after birth, which were reported by 91.4%, 97.1% and 54.3% of mothers, respectively (Table 1).
| Table 1. Most relevant perinatal aspects in our sample of breastfed children | |
|---|---|
| Sex | Male 65.7%; female 34.3% |
| Type of delivery | Caesarean 31.4%, normal 58.3%, instrumental 10.3% |
| Initiation of breastfeeding | 80% in first 3 hours, 54% in first hour, 5.7% after more than 6 hours |
| Exclusive breastfeeding at 6 months | 91.4% |
| Co-sleeping | 97.1% |
| Skin-to-skin contact | 54.3% |

Variables related to breastfeeding initiation
Sixty percent of mothers were breastfeeding at the time of the survey, while 57.1% reported their previous experience with BF.
All mothers reported intending to BF from the outset, and would choose it again as their first feeding option. As for the timing of weaning, 85.7% reported wanting to continue BF until the child weaned him or herself off. Other relevant findings involved the rate of BF during pregnancy and of tandem BF, which were reported by 34.2% and 20% of mothers, respectively.
Socio-cultural aspects in breastfeeding and extended breastfeeding
The main sources of BF support, both in establishing and maintaining it, were healthcare professionals (58%) and support groups (42%).
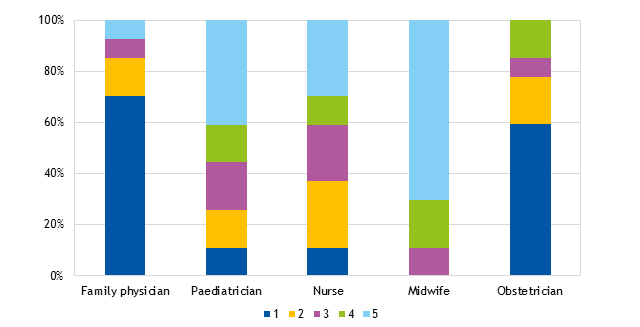
When it came to the degree of helpfulness of healthcare professionals, 65.7% of mothers reported receiving some type of support from this collective. The professionals rated as being most supportive were midwives (4.39 ± 0.69) and paediatricians (3.28 ± 1.44), and those rated as least supportive were family physicians (1.27 ± 1.15) and obstetricians (1.58 ± 1.12) (Figure 1).
| Figure 1. Level of support offered by healthcare professionals |
|---|
 |

To complete our analysis, we placed particular emphasis on BF beyond age 12 months, which is misleadingly referred to as EBF. We explored social aspects to assess the feelings and concerns that mothers experience in different environments. We ought to highlight that 50% of surveyed mothers reported that BF beyond 12 months was common in their social environment. The level of satisfaction with this experience was very high (4.37 ± 0.51 points out of a possible 5), but up to 48.6% of mothers reported experiencing some form of social rejection. Barriers were reported by 51.4%, most frequently involving family or friends. Furthermore, 45.7% of mothers reported having to hide that they breastfed at some point, mainly from relatives or co-workers. Figure 2
| Figure 2. Perception of extended breastfeeding in different everyday life settings |
|---|
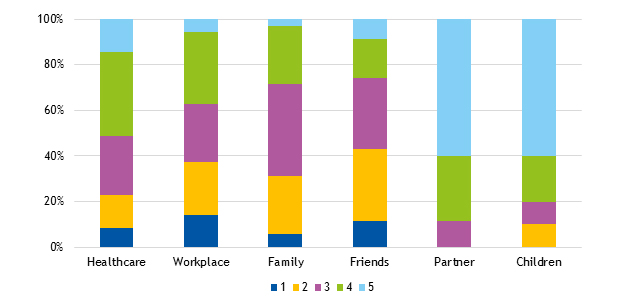 |

represents how mothers believe their EBF is perceived in different settings of their everyday life. The partner (4.29 ± 0.70) and other children of the mother (4.10 ± 1.03) received the highest scores, while relatives (2.29 ± 1.16), friends (2.42 ± 1.17) and co-workers (2.36 ± 0.78) received the lowest scores.
DISCUSSION
Duration of breastfeeding, weaning age
In more traditional societies where the use of formula is not widespread, the mean duration of BF is 3 to 4 years, according to ethnographic sources.10 In these ethnic groups, which have little contact with outside influences, the weaning age varies, ranging from 4 months in the Khoikhoi of Africa to 5 years in Hawaiian tribes and 7 or more in some Eskimo populations.11 In year 1989, out of a total of 46 non-industrialised societies in the world, weaning occurred between ages 2 and 3 years in 75%, and by 18 months in the rest; the mean age was 6 months in only one country.10
The latest guidelines recommend maintaining BF for as long as the mother and child desire, as 85.7% of our respondents intended to do. It is recommended that once a woman feels it is time to wean the child, she does not do so abruptly or use ploys to deceive the child. The best strategy is gradual weaning, without offering or withholding the breast, and possibly negotiating conditions with the child (for instance, BF only in certain places or situations, or for a limited amount of time). During weaning, it is important to offer the child alternatives to satisfy the need for closeness, as the attachment that develops through BF is very deep and needs to be reoriented in a gradual fashion.12
Establishment and maintenance of breastfeeding in Spain
Despite the known benefits of BF and the efforts made to promote it, BF rates in Spain have been low in recent decades. Data from the Encuesta Nacional de Salud (National Health Survey [ENS]) of the Ministry of Health and Consumer Affairs revealed a very low rate of exclusive BF at 6 months, of 15% in year 1995 and 21% in 1997.13 One of the largest studies on the prevalence of BF conducted in Spain was promoted by the Committee on BF of the AEP in 1997, and consisted of a cross-sectional survey of mothers in 18 provinces. The median duration of BF reported in the more than 10 000 completed questionnaires was 3.0 months (95% confidence interval [95 CI]: 2.93 to 3.07). The rate of BF (exclusive and mixed) was 77.6% in the first month of life, 54.6% at 3 months, 25% at 6 months and 7% at 1 year of age. The most salient finding may be that only 55% of mothers breastfed their children, exclusively or otherwise, for more than 3 months.14 Other studies in different autonomous communities found similar percentages.15,16 Based on the data of the last ENS survey published by the Instituto Nacional de Estadística in 2011, the prevalence of exclusive BF in Spain is of 63% at 6 weeks and 26% at 6 months.17 There seems to have been a slight improvement in Spain in the past 15 years, especially in the duration of BF. This improvement is more manifest in Aragon, where the prevalence exceeds the national average, after the IHAN programme was launched in the Hospital de Alcañiz, with maintenance of BF in 41.8% of mothers at 6 months and 12.2% at 1 year, practically doubling the percentages found in previous studies.18 The CALINA longitudinal study aimed to determine the prevalence of BF through the 12-month followup of 1602 infants born between March 2009 and March 2010. The authors reported that overall BF (exclusive and mixed) was maintained in 82.5% at 1 month of life, 71.8% at 3 months, 54.3% at 6 months and 27.8% at 1 year.19 In Zaragoza, a retrospective review of 550 mothers and children born between 2010-2012 and followed up over 12 months found a mean duration of exclusive BF of 2.5 months and of overall BF of 5.1 months. Breastfeeding rates remained high, although they were slightly lower than those found in the CALINA study: 74% at 1 month of life, 40.7% at 6 months and 14.2% at 1 year. The factors most strongly associated with BF rates were: difficulty establishing BF in the first month and the return of the mother to the workplace between the fourth and sixth month.20
Benefits and risks of BF in older children
Breast milk does not lose its properties with the passage of time.21 After one year of lactation, the fat content of the milk increases compared to the first months,22 yielding a balanced and nutritious food that covers one third of the daily energy and protein requirements (sometimes more, especially during illness), while also providing significant amounts of vitamins and minerals. In addition, the immunological benefits of breast milk persist, with a lower incidence of infection in breastfed children compared to children of the same age who are not breastfed. These benefits are not only observed in the short term, but also years after weaning, as there is evidence of a lower incidence of certain types of cancer (leukaemia), metabolic disorders and autoimmune diseases (such as type 1 diabetes).23,24 Another study found that cognitive development improved with increased duration and exclusiveness of BF, an effect that persists for years and may even be associated with higher educational attainment and income in adulthood.25 Several studies have found a positive correlation between BF duration and improved social and emotional development in children.26 Lastly, the literature describes several benefits for mothers who breastfeed, such as a decreasing risk of type 2 diabetes, breast cancer, ovarian cancer, high blood pressure and heart attack with increasing overall duration of breastfeeding.
As for the risks, there is no evidence in the literature of any physical or psychological risks in children that breastfeed beyond 2 or 3 years of age. There is also no evidence of an association of EBF with malnutrition in developing countries27 or with tooth decay in children.
Breastfeeding during pregnancy (in 34.2% of our sample), when wanted by the mother, does not carry any known risks, although the possibility of discontinuing it should be considered and assessed on a case-to-case basis if there is risk of miscarriage or preterm labour, or in other special situations.28 Tandem BF (20% in our sample) is possible, as milk production is adjusted to meet demand. The main risks are that the mother may feel overwhelmed by the demands of both children and the contradictory feelings she may have regarding breastfeeding the older child.29
Beyond doubt, the main problem in BF beyond 1 year of age is the rejection by society and health professionals rooted in prejudice and ignorance of the current scientific evidence. We found ample evidence of this fact in our survey. We should start by underscoring a relevant finding: 58% of mothers sought support or guidance from healthcare professionals. Therefore, we must be aware of the key role we play as healthcare professionals, and it is our duty and responsibility to update our knowledge on BF so that each family and each mother can make informed decisions. If their wish is to continue BF, our duty is to support this decision and provide tools for them to overcome the difficulties they may encounter. In short, as healthcare professionals we must offer information and respect. In our survey, only midwives and paediatricians received good ratings in relation to providing support to mothers, so we need to continue improving on this front. Furthermore, the remaining 42% of mothers attended BF support groups, a strategy that has also proven useful in supporting and reinforcing the decision to breastfeed beyond 12-24 months of age.30
It is very important that these concerns are resolved, as ultimately the degree of satisfaction reported by respondents in relation to EBF was very high, and they described the experience as very positive. Furthermore, all mothers would choose to breastfeed again as their first option.
We ought to highlight the considerably high proportions we found of various types of social conflict, as approximately half of the surveyed mothers reported experiencing some degree of social rejection, having encountered barriers to EBF or even having had to conceal its practice at some point. The spheres that are most hostile in this regard continue to be the traditional social networks, such as family, friends and co-workers.
CONCLUSIONS
Human milk continues to be the best and most complete food for infants, but is also highly beneficial after 1 year of life, with no risk associated with continued BF. Weaning should happen when the mother and child desire. Mothers report a high level of satisfaction in continuing to breastfeed their older children. As healthcare professionals, we are one of their main sources of support, and our duty is to provide information and be respectful. There is still considerable prejudice against mothers that continue to breastfeed older children, which prevents them from carrying it out naturally.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS
AAP: American Academy of Pediatrics · AEP: Asociación Española de Pediatría · CI: confidence interval · BF: breastfeeding · EBF: extended breastfeeding · SSC: skin-to-skin contact · WHO: World Health Organization.
REFERENCES
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep). 2007;153:1-186.
- Gartner LM, Morton J, Lawrence RA, Naylor AJ, O’Hare D, Schanler RJ, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496-506.
- Nutrición del lactante y del niño pequeño. Estrategia mundial para la alimentación del lactante y del niño pequeño. Report by the Secretariat. 55th World Health Assembly. In: World Health Organization [online] [accessed 24/10/2017]. Available at http://apps.who.int/iris/bitstream/10665/81907/1/sa5515.pdf
- Innocenti Declaration on the Protection, Promotion and Support of Breastfeeding. In: UNICEF [online] [accessed 24/10/2017]. Available at www.unicef.org/programme/breastfeeding/innocenti.htm
- Comité de Lactancia Materna de la AEP. Recomendaciones sobre lactancia materna. In: Asociación Española de Pediatría [online] [accessed 24/10/2017]. Available at www.aeped.es/sites/default/files/recomendaciones_lm_26-1-2012.pdf
- Dowling S, Brown A. An exploration of the experiences of mothers who breastfeed long-term: what are the issues and why does it matter? Breastfeed Med. 2013;8:45-52.
- Cockerham-Colas L, Geer L, Benker K, Joseph MA. Exploring and influencing the knowledge and attitudes of health professionals towards extended breastfeeding. Breastfeed Med. 2012;7:143-50.
- Paricio JM. Lactancia prolongada… ¿Hasta cuándo es normal? Perspectiva histórico-antropológica. VII Congreso español de Lactancia Materna. Madrid; 2014.
- Piovanetti Y. Breastfeeding beyond 12 months: an historical perspective. Pediatr Clin North Am. 2001;48:199-206.
- Stuart-Macadm P, Dettwyker KA. Breastfeeding. Biocultural perspectives. Nueva York: Ed. Aldine de Gruyter; 1995.
- Wickes IG. A history of infant feeding. I. Primitive peoples; ancient works; Renaissance writers. Arch Dis Child. 1953;28:151-8.
- Gribble KD. “As good as chocolate” and “better than ice cream”: how toddler, and older, breastfeeders experience breastfeeding. Early Child Dev Care. 2009;179:1067-82.
- Encuesta sobre discapacidades, deficiencias y estado de salud 1999. In: Instituto Nacional de Estadística [online] [accessed 24/10/2017]. Available at www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176782&menu=resultados&idp=1254735573175)
- García Vera C, Martín Calama J. Lactancia materna en España. Resultado de una encuesta de ámbito estatal. Rev Pediatr Aten Primaria. 2000;2:373-87.
- Ortega JA, Pastor E, Martínez I, Bosch V, Quesada J, Hernández F, et al. Proyecto Malama: medio ambiente y lactancia materna. An Pediatr (Barc). 2008;68:447-53.
- González M, Toledano J. La lactancia materna en nuestro medio: análisis de la situación. Acta Pediatr Esp. 2007;65:123-5.
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Encuesta Nacional de Salud 2011. In: Instituto Nacional de Estadística [online] [accessed 24/10/2017]. Available at www.ine.es/prensa/np770.pdf
- Guerrero C, Garafulla J, Lozano D, García C, Bielsa A. Estudio lactancia en Área Hospital de Alcañiz. ¿Merece la pena poner en práctica los diez pasos de la Iniciativa Hospital Amigo de los Niños en un hospital comarcal? Bol Pediatr Arag Rioj Sor. 2006;36:20-6.
- Oves B, Escartín L, Samper MP, Cuadrón L, Álvarez ML, Lasarte JJ, et al. Inmigración y factores asociados con la lactancia materna. Estudio CALINA. An Pediatr (Barc). 2014;81:32-8.
- Giménez V, Jimeno B, Valles MD, Sanz E. Prevalencia de la lactancia materna en un centro de salud de Zaragoza (España). Factores sociosanitarios que la condicionan. Rev Pediatr Aten Primaria. 2015;17:17-26.
- Boediman D, Ismail D, Iman S, Ismangoen, Ismadi SD. Composition of breast milk beyond one year. J Trop Pediatr Environ Child Health. 1979; 25:107-10.
- Mandel D, Lubetzky R, Dollberg S, Barak S, Mimouni FB. Fat and energy contents of expressed human breast milk in prolonged lactation. Pediatrics. 2005;116:e432-5.
- Amitay EL, Keinan-Boker L. Breastfeeding and childhood leukemia incidence: a meta-analysis and systematic review. JAMA Pediatr. 2015;169:e151025.
- Patelarou E, Girvalaki C, Brokalaki H, Patelarou A, Androulaki Z, Vardavas C. Current evidence on the associations of breastfeeding, infant formula, and cow’s milk introduction with type 1 diabetes mellitus: a systematic review. Nutr Rev. 2012;70:509-19.
- Belfort MB, Rifas-Shiman SL, Kleinman KP, Guthrie LB, Bellinger DC, Taveras EM, et al. Infant feeding and childhood cognition at ages 3 and 7 years: effects of breastfeeding duration and exclusivity. JAMA Pediatr. 2013;167:836-44.
- Lawrence RA. Supporting breastfeeding/early childhood social and emotion development. In: Encyclopedia on Early Childhood Development [online] [accessed 24/10/2017]. Available at www.child-encyclopedia.com/breastfeeding/according-experts/supporting-breastfeedingearly-childhood-social-and-emotion
- Cousens S, Nacro B, Curtis V, Kanki B, Tall F, Traore E, et al. Prolonged breast-feeding: no association with increased risk of clinical malnutrition in young children in Burkina Faso. Bull World Health Organ. 1993;71:713-22.
- Cetin I, Assandro P, Massari M, Sagone A, Gennaretti R, Donzelli G, et al. Breastfeeding during pregnancy: position paper of the Italian Society of Perinatal Medicine and the Task Force on Breastfeeding, Ministry of Health, Italy. J Hum Lact. 2014;30:20-7.
- Bryant T. Tandem nursing: a review and guidelines. Int J Childbirth Educ. 2012;27:84-8.
- Thomson G, Crossland N, Dykes F. Giving me hope: women’s reflections on a breastfeeding peer support service. Matern Child Nutr. 2012;8:340-53.





