Vol. 18 - Num. 72
Original Papers
Follow-up in Primary Care Pediatric consultations of very premature babies: born at less than 32 weeks' gestation or weighing less than 1500 grams
Begoña Domínguez Aurrecoecheaa, Guadalupe del Castillo Aguasb, César García Verac, R García Pérezd, Ana Martínez Rubioe, José M.ª Mengual Gilf
aPediatra. Instituto de Investigación Sanitaria del Principado de Asturias (ISPA). Asturias. España.
bUnidad de Atención Infantil Temprana. CS Colonia Sta. Inés-Teatinos. Málaga. España.
cPediatra. CS José Ramon Muñoz Fernández. Zaragoza. España.
dPediatra. CS Txurdinaga. Bilbao. España.
ePediatra. CS de Camas. Sevilla. España.
fPediatra. CS Delicias Sur. Zaragoza. España.
Correspondence: B Domínguez. E-mail: begoa.dominguez@gmail.com
Reference of this article: Domínguez Aurrecoechea B, del Castillo Aguas G, García Vera C, García Pérez R, Martínez Rubio A, Mengual Gil JM. Follow-up in Primary Care Pediatric consultations of very premature babies: born at less than 32 weeks' gestation or weighing less than 1500 grams. Rev Pediatr Aten Primaria. 2016;18:311-6.
Published in Internet: 19-10-2016 - Visits: 17503
Abstract
Introduction: almost 20% of premature babies abandons the follow-up in hospitals and they have worse outcomes than those who continue the program. Obtaining data on the involvement of Primary Care pediatricians (PAPs) in monitoring premature babies born at less than 32 weeks or weighing less than 1500 g is necessary to propose strategies for improvement.
Methods: it is an observational, transversal, descriptive study, in the area of the 17 Spanish autonomous communities, through PAPenRED network (304 PAPs). Data were collected by questionnaires filled out online about the number of premature babies by pediatrician, the type of monitoring and the difficulties found in their attention. Frequency distributions, percentages, qualitative variables are described.
Results: 870 very premature infants were included with an average of 3.8 per pediatrician. 68.84% of PAPs do not share a common monitoring program between hospitals and Primary Care centers, despite the fact that 99% of the pediatricians would like to have it. 84.27% say that these children have more complex problems. The diseases that occur more frequently compared to those born at term are family anxiety, respiratory disease and problems in relation to growth, feeding, motor development and cognitive and behavioral issues.
Conclusions: PAPs believe necessary commmon programs between hospitals and Primary Care centers for monitoring the very premature babies.
Keywords
● Follow-up studies ● Premature ● Primary careINTRODUCTION
Preterm birth is one of the most prevalent health problems in children in developed countries. Between eight and ten percent of births occur before 37 weeks’ gestation, and these births account for 75% of perinatal mortality and 50% of childhood disabilities.1
Preterm birth has a psychological, family, social and occupational impact that is difficult to quantify in economic terms, and places a financial burden on the health care system estimated at a little over 1200 euro a day until the newborn is discharged, but which will continue to grow through the lifespan depending on the subsequent development of each individual.2
Technological and therapeutic advances in perinatal care have reduced the mortality of newborns (NBs) weighing less than 1500 grams, and changed the associated morbidity.3
Long-term follow-up studies have shown that even children that are considered normal and without functional limitations on evaluation at age 2 years go on to develop learning disorders, have a reduced survival and have reproductive health problems, and women that were born preterm are at higher risk of giving birth preterm.4
Nearly 20% of children born very preterm drop out of followup at hospitals, and those that do not attend checkups have worse outcomes than children that adhere to the programme.
Primary Care (PC) paediatric services provide efficient and humanised health care, keeping in close contact with children and their families and taking into account the specific characteristics of their environment; in addition, the PC paediatrician is responsible for providing care for chronic diseases, coordinating the necessary resources, advising children and their families in their interactions with the health care system and serving as case managers and coordinators and as regulators of patient flow. Between 85% and 90% of the population aged 0 to 14 years receives care at their offices, with a mean of four visits per patient in year 2015, and patients aged 0 to 4 ages making the most visits (nine a year). In 2014, 33 millions of visits were made to PC clinics in Spain.5
Based on this information, PC paediatrics seems to be the ideal setting for the intermediate- and long-term follow up of children born very preterm, facilitating their access to health care services. The use of joint follow-up protocols by hospital and PC services would prevent the duplication of visits and diagnostic tests, improve the use of resources, and facilitate research.1
The aim of this study was to collect data on the involvement of PC paediatricians in the followup of children born very preterm before 32 weeks’ gestation or with a birth weight of less than 1500 g, and to propose measures to improve care for this population based on this information.
MATERIALS AND METHODS
We conducted a descriptive, cross-sectional observational study in the seventeen autonomous communities (ACs) of Spain through the Primary Care Research Network (PAPenRED).
The PAPenRED is a network of sentinel surveillance collaborators employed in public or government-subsidised primary care centres in all ACs with a distribution proportional to that of the population. At the time of the study (data collection period, May 1 to June 30, 2015), the network consisted of 304 paediatricians that submitted data through an online survey available at http://tinyurl.com/grandes-prematuros.
The inclusion criteria were: child aged less than 15 years at the time of the study, born at a gestational age of less than 32 weeks or with a weight of less than 1500 g, and with complete data in the medical records. After applying these criteria, we collected data for the following variables: number of children born very preterm per caseload, type of followup, difficulties encountered in health care delivery, and the most frequent pathologies.
We analysed the data by finding the distribution in frequencies and percentages of the qualitative variables. Inferential analysis did not apply.
RESULTS
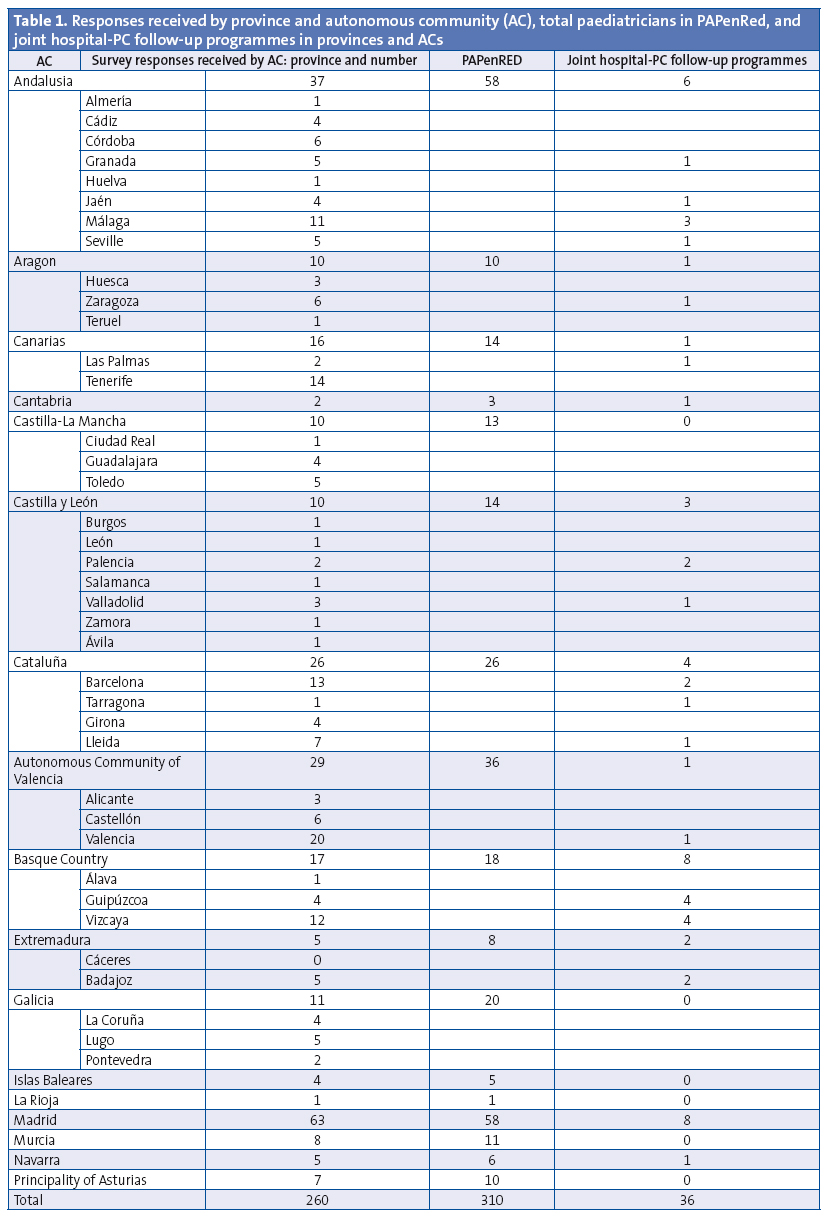
We collected data for 260 paediatricians serving a population of approximately 234 900 children aged 0 to 14 years; 35 paediatricians (13.4%) could not provide the number of children born preterm in their caseloads.
The total number of children born very preterm was 870, with a mean of 3.8 per paediatrician, and eleven paediatricians as outliers with ten or more children born very preterm in their caseloads (Figure 1).

Of all the responding PC paediatricians, 68.84% reported not having a joint hospital-PC follow-up programme; 45 were not aware of such a programme, but were not certain that it did not exist. Of the 36 PC paediatricians that reported having a joint programme, eight worked in the Basque Country, eight in Madrid, six in Andalusia, four in Catalonia and two in Castilla y León (Table 1). The paediatricians in five ACs did not report having joint hospital-PC follow-up programmes. Of all PC paediatricians, 7.6% did not have a specific follow-up protocol. Twenty-one percent of paediatricians that did not have a programme followed hospital guidelines and 26.8% also used the follow-up programme published in PrevInfad.1
Ninety-nine percent of PC paediatricians would like to have a joint followup hospital-PC programme. Of all respondents, 72.09% considered that children born very preterm visited PC clinics more frequently than children born at term, and 84.27% reported that children born very preterm presented with more complex problems.
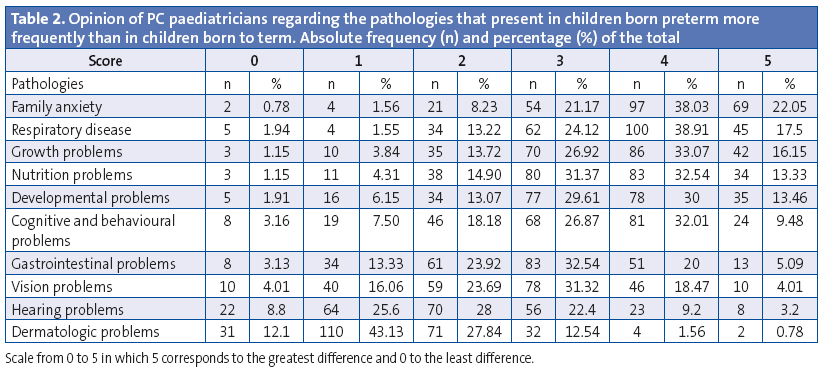
The pathologies reported most frequently in comparison to children born to term (Table 2) were: family anxiety, which on a scale of 0 to 5 was reported at 4 to 5 in 77.3% of the received responses; respiratory diseases, scored at 4 or 5 in 67.59% of responses; growth problems in 60.18% of responses; problems related to nutrition in 54.6% of responses, followed by psychomotor development problems (52.77%) and cognitive and behavioural disorders (49.0%); the differences were lesser in gastrointestinal, vision and hearing problems, and minimal in dermatologic problems.
The main difficulties experienced by PC paediatricians in completing the survey involved access to electronic data and diagnostic coding.
CONCLUSIONS
Primary care paediatricians believe that follow-up programmes in collaboration with hospital-based PC are necessary in the care of children born very preterm.
Diagnostic codes need to be reviewed in order to adjust them to the pathologies found in childhood, and PC paediatricians should be granted access to electronic data for research purposes.
This has a translational research orientation, as its results will be relayed to the collectives involved in the care of children born very preterm and support the development of a joint follow-up protocol applicable to everyday clinical practice with the goal of improving care delivery in this subset of the paediatric population.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: AC: autonomous community · NB: newborn · PC: Primary Care.
ACKNOWLEDGMENTS
We thank all collaborating paediatricians of the PAPenRED: https://goo.gl/X6MyFI
BIBLIOGRAFÍA
- Carmen Rosa Pallás Alonso. Programa de Actividades Preventivas y de Promoción de la Salud para niños prematuros con una edad gestacional menor de 32 semanas o un peso inferior a 1500 gramos. Del alta hospitalaria a los 7 años. In: Asociación Española de Pediatría de Atención Primaria [online] [updated on 28/03/2010; consulted on 05/10/2016]. Available in www.aepap.org/previnfad/rec_menor32-1500.htm
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Estrategia de promoción de la salud y prevención en el SNS. En el marco del abordaje de la cronicidad en el SNS. Estrategia aprobada por el Consejo Interterritorial del Sistema Nacional de Salud el 18 de diciembre de 2013. Madrid: MSSSI; 2014. Available in www.msssi.gob.es/profesionales/saludPublica/prevPromocion/Estrategia/docs/EstrategiaPromocionSaludyPrevencionSNS.pdf
- García P, San Feliciano L, Benito F, García R, Guzmán J, Salas S, et al. Evolución a los 2 años de edad corregida de una cohorte de recién nacidos con peso inferior o igual a 1500 g de los hospitales pertenecientes a la red neonatal SEN1500. An Pediatr (Barc). 2013;79:279-87.
- Swamy GK, Osbye T, Skjaerven R. Association of preterm birth with long term survival, reproduction and next generation preterm birth. JAMA. 2008;299:1429-36.
- Sistema de Información de Atención Primaria SIAP. Actividad asistencial en centros de Atención Primaria y a domicilio (realizada en el horario habitual de funcionamiento, actividad ordinaria). En: Ministerio de Sanidad, Servicios Sociales e Igualdad [[online] [updated on 28/03/2010; consulted on 05/10/2016]. Available in www.msssi.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/docs/Actividad_ordinaria_A_P_2014.pdf





