Vol. 18 - Num. 71
Original Papers
Vitamin D deficiency: situation in an urban center of the Mediterranean coast
Ramona Martín Martína, Antoni Collado Cucòb
aServicio de Pediatría. ABS Marià Fortuny. Reus. Tarragona. España.
bMédico Adjunto. CAP Riudoms. Riudoms. Tarragona. España.
Correspondence: R Martín. E-mail: rmartin@grupsagessa.com
Reference of this article: Martín Martín R, Collado Cucò A. Vitamin D deficiency: situation in an urban center of the Mediterranean coast. Rev Pediatr Aten Primaria. 2016;18:213-8.
Published in Internet: 08-09-2016 - Visits: 18553
Abstract
Introduction: in recent years several proposals have been made on the need to supplement the diet with vitamin D. We are witnessing a rise in the deficit, related to situations that increase the risk: prematurity, prolonged exclusive breastfeeding, dark-skinned immigrants, less sun exposure.
Objective: find out if vitamin D deficiency is a common problem in children of a village in the Mediterranean coast.
Material and methods: observational study. Vitamin D value determination, for a period of 18 months, in children from 0 to 15 years assigned to a Primary Care center, in a blood sample obtained coinciding with any reason. Statistical analysis: Descriptive and inferential statistics, analysis of conformity of the sample.
Results: 145 determinations were performed. 42.1% immigrant children and 57.9% national. The total sample 37.9% had some degree of vitamin D deficiency: mild: 67.3%, moderate: 21.8%, severe: 10.9%. 30% of men and 44% of women had deficits. 20% of Spanish children had vitamin D deficiency compared to 62% of immigrant children (p <0.001%). Between national children he had deficit 15% of men and 24% of women. Among immigrants, 45% of men and 82% of women.
Conclusions: vitamin D deficiency is very common in our environment. Immigrants, female sex, especially if they are teenagers are the ones who are more likely to present it.
Keywords
● Vitamin D ● Vitamin D deficiencyINTRODUCTION
In recent years, different recommendations regarding the use or lack thereof of dietary vitamin D (VD) supplementation have been made in the paediatrics field. This controversy can be explained by the lack of specific biomarkers and of universal criteria defining optimal VD levels and VD deficiency. The heterogeneity of the methods used to measure VD and the cut-off values used to define normal levels in research account for the wide variability in reported prevalences. Furthermore, some of the related variables are difficult to assess: the endogenous sunlight-dependent synthesis of vitamin D, and the intake of foods fortified with VD. These limitations notwithstanding, recent evidence suggests that the prevalence of vitamin D deficiency may be increasing in children of all ages.
The recommendations for VD supplementation vary across institutions and countries. Some of them take into account the influence of VD levels on skeletal tissue and the development of chronic diseases.1
New functions of VD have been described recently, such as its role in cancer prevention and in the development of cardiovascular diseases and high blood pressure, diabetes, metabolic syndrome, the immune response, pathological neuropsychological states and reproductive health.1-5
Although it was assumed that the prevalence of VD deficiency was very low in developed countries, we are witnessing a resurgence that is associated with circumstances that increase the risk of developing it: preterm birth, prolonged exclusive breastfeeding, immigration of individuals from ethnic groups with dark skin pigmentation, and lack of sun exposure due to cultural or religious reasons or to lifestyle changes.1
The aim of our study was to determine the prevalence of VD deficiency in the children residing in an urban area of a developed country undergoing an economic crisis in the Mediterranean coast.
MATERIALS AND METHODS
We analysed the levels of vitamin D (25-hydroxyvitamin D [25(OH)D]) over a period of 18 months between February 1, 2013 and July 31, 2014, of all children aged 0 to 15 years in the paediatrics primary care caseload in an urban area of the Mediterranean coast with a population of 100 000 inhabitants that underwent blood testing for any reason.
The cut-off value that we applied for the diagnosis of vitamin D deficiency in children was 20 ng/mL, as this is the threshold most widely accepted by the scientific community in recent years. Following the same criteria, we classified the levels of 25(OH)D as optimal (30–80 ng/mL), insufficiency (20–30 ng/mL), mild deficiency (10–20 ng/mL), moderate deficiency (5-10 ng/mL) and severe deficiency (< 5 ng/mL).6-8
Our statistical analysis included descriptive statistics (frequency distributions and measures of position and dispersion), inferential statistics (comparison of means, analysis of variance and multivariate logistic regression) and concordance analysis for the sample.
RESULTS
A total of 145 measurements of vitamin D levels were performed (54.5% in female patients, 45.5% in males). In this sample, 42.1% of children were immigrants (61) and 57.9% Spanish nationals (84). This distribution does not differ significantly from the distribution of the entire target population (37% immigrant children out of a total of 1360 children). The distribution by region of origin of immigrant children was the following: Morocco, 78.7%; Romania, 9.8%; Latin America, 6.4%; and Asia, 4.8%.
Of all patients in the sample, 37.9% had some degree of vitamin D deficiency: mild (67.3%), moderate (21.8%) or severe (10.9%).
Calcium and phosphorus levels were normal in all children. The levels of alkaline phosphatase were elevated in 25.5% of patients, with no association with the degree of deficiency (difference not statistically significant, P > .1). Eleven percent had nonspecific symptoms (asthenia, anorexia or muscle pain) that were not associated with the degree of vitamin D deficiency (difference not statistically significant, P > .1).
When we analysed the sample by sex, we found that 30% of boys and 44% of girls had vitamin D deficiency (P > .05).
When we analysed the sample by region of origin, 20% of Spanish children had vitamin D deficiency compared to 62% of immigrant children, a difference that was statistically significant (P < .001%).
In the subset of Spanish children, 15% of boys and 24% of girls had vitamin D deficiency, and the difference was not statistically significant (P > .1). In the subset of immigrant children, vitamin D was found in 45% of boys and 82% of girls (P = .02).
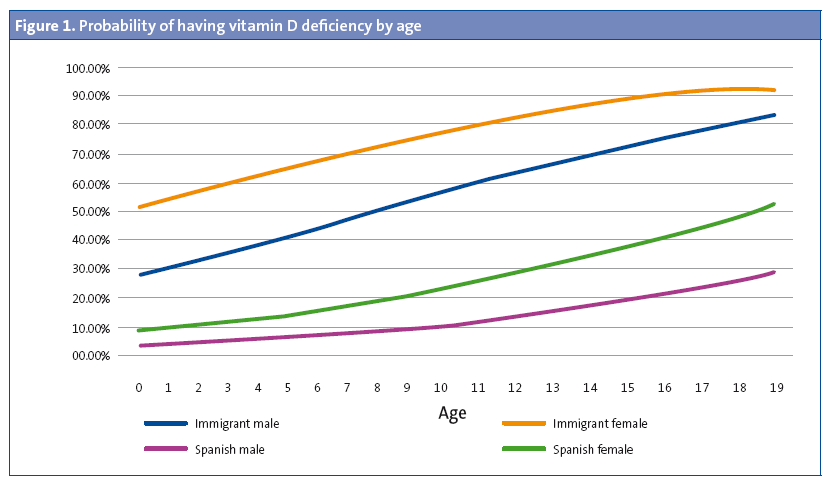
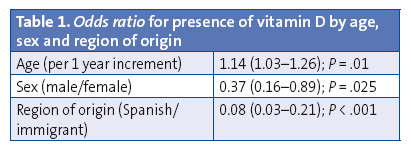
As for the distribution by age group, 26% of children aged less than 5 years had VD deficiency compared to 38% of children aged 5 to 10 years. The group with the highest prevalence of deficiency, of 44%, was that of children aged 11 to 15 years. Figure 1 shows the probability of having VD deficiency by age, and Table 1 presents the odds ratio for each of the variables under study.
DISCUSSION
We conducted a cross-sectional study to assess the presence or absence of a problem guided by the scientific literature published in the last few years, which suggests that this deficiency is experiencing a resurgence. With the improvements in nutrition that started in the 1950s and the high number of sunny days per year, vitamin D deficiency was considered all but eradicated in Spain. Our study cannot establish a causal relationship, but considering what is known about the factors that influence low VD levels and our knowledge of the habits of the population that we serve, we could try to elucidate the factors that have contributed to our findings.
The recommended daily allowance established for infants aged less than 1 year is 400 IU. For older children, it is 600 IU.9 These amounts are hard to attain exclusively from dietary sources, which has led many scientific associations to recommend supplementation.
According to the latest recommendations of the American Academy of Pediatrics,7 the PrevInfad working group1,10 and the Committee on Breastfeeding of the Spanish Association of Paediatrics,9 in infants aged less than 1 year, supplementation should be given when they are breastfed or when the intake of artificial formula is of less than one litre a day or does not provide 400 IU of VD a day; in children aged more than 1 year, supplementation should be given if the intake of dairy products and fortified foods is insufficient or if the levels of 25(OH)D are less than 20 ng/mL until they normalize.9
Since 2007, the Canadian Paediatric Society has recommended a daily intake of vitamin D of 400 IU for all infants aged less than 1 year, raising it to 800 IU during the winter for children that live north of the 55th parallel and children living between the 40th and the 55th parallels with risk factors other than latitude alone.11
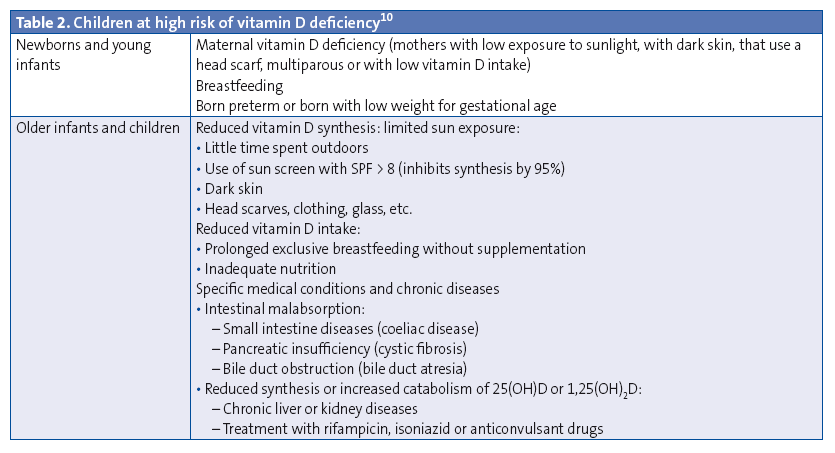
Plasma levels of VD vary based on the duration, time of day, latitude, altitude and season of sunlight exposure, as well as on the age, skin pigmentation, body surface area exposed and sun protection use of the individual. The levels can also vary based on the diet and other factors (Table 2).10
Few foods contain VD. Most that do are dairy products. Eggs and some oily fish contain significant amounts, although the amount varies between species, tissues, and through the year. But dietary sources of VD only account for 10% of the VD plasma levels that can be achieved, compared to the 90% derived from cutaneous synthesis.
Breastfeeding provides variable amounts of VD, estimated to range between 25 and 136 IU/L depending on maternal diet and sun exposure.12 Commercially available artificial formulas in Spain are fortified and contain 200 IU per 300 to 500 mL. More than two litres of breast milk or one litre of formula would be needed to achieve intakes of 400 IU/day.12 In our area, whole cow’s milk—not fortified, and containing 240 IU per litre—is introduced starting at age 12 months in the immigrant population and 18 to 24 months in the Spanish native population. Achieving the recommended intake of 400 IU/day would require consuming 1600 mL of this milk or 13 containers of yogurt every day. Consuming such volumes would be difficult. In our population, the intake of milk, yogurt or other dairy products is of 500 to 1000 mL of milk and/or one or two yogurt containers a day.
There is sufficient scientific evidence to support that most of the vitamin D in the body is synthesised in the skin and that 15 minutes a day of sun exposure would suffice to guarantee the recommended daily allowance, but no systematic review provides data to determine the levels of exposure that are sufficient and safe to guarantee optimal vitamin D levels. It has been demonstrated, however, that habitual lack of exposure is a risk factor for deficiency. Some scientific societies and groups of experts have published recommendations that take this into account. In 2010, PrevInfad made a general recommendation that children aged more than 1 year and adolescents be exposed to sunlight daily and without protection for a period of 10 to 15 minutes in the spring, summer and autumn (grade I recommendation).1,10 During the summer, exposure of only the arms, hands and face for this duration would suffice to release 1000 units, which would fulfil the daily requirement.10
In addition to the duration of sun exposure, cutaneous synthesis of vitamin D is influenced by geographical latitude. There is a threshold level of UVB radiation required to induce synthesis. The ideal threshold is located at the equator and decreases northward, and the threshold is usually not reached during the winter in areas at latitudes above 40° north. In the winter, vitamin D synthesis is nonexistent at latitudes above 42° north.1 Some regions in Spain are above 42° north.
Our city enjoys a mild climate that allows outdoor activity from May to October, and an advantageous geographical location 10 km from the shore. This facilitates the recommended 15 minutes’ exposure to sunlight in our population during these months. Yet due to our location at 41° north, the level of radiation may not suffice for vitamin D synthesis, especially during the winter.
Immigrants constitute 37% of the population we serve, with a majority being of Moroccan descent. Most of the boys and girls that receive care in our centre dress in the Western style. During adolescence, girls start to use traditional clothing and headscarves, exposing only the skin of their faces and hands. This attire could account for the higher prevalence of vitamin D deficiency in female adolescents, but not for the prevalence in boys and girls, which, based on our findings, is above the national average.
This population has darker skin, especially in individuals of Berber and Saharan descent, who are the majority in our population, compared to individuals of Arabian descent. Skin pigmentation influences the exposure time needed to produce a certain level of VD. Individuals of Indo-Asian descent require three times as long an exposure to achieve the same levels of VD as light-skinned individuals, and African-American individuals with highly pigmented skin require ten times the exposure.1
In recent years, both primary care centres and dermatology units in Spain have heavily promoted the use of sun protection measures (use of hats, shirts, parasols, sunscreen, etc) that are currently widely implemented. As recommended by dermatology units, we advise the use of a physical or chemical sunscreen with a sun protection factor of 30 or higher. Some studies suggest that the use of sunscreen with SPFs above 8 result in a reduction of vitamin D synthesis of more than 95%.1
Although sun exposure in our population could be sufficient most of the year, there is still a high prevalence of vitamin D deficiency. The diet does not help alleviate this problem, as the consumption of dairy products, while being adequate in volume, consists of foods that are not fortified, as the use of toddler formula (age 1–3 years) fortified with vitamin D is not widespread in Spain and has declined with the economic crisis.
In light of our results, the characteristics of our population, the vitamin D content of the dairy products that are consumed, and our geographical location, we could consider recommending VD supplementation as a nutritional strategy to prevent or alleviate this deficiency, given the few side effects of these supplements when they are administered in the recommended doses.7 Another option would be to increase the intake of fortified foods, but this would have a negligible impact in Spain, where few of these foods are commercialised. In other countries, all dairy products and a large proportion of juices and cereals in the market are fortified.
By implementing this strategy, we would adhere to the recommendations of the major associations of paediatrics, as nearly all of our population fulfils at least one the criteria for supplementation. Yet our children have vitamin D deficiency in isolation, with no repercussions on markers of bone metabolism, and are asymptomatic. Given these data, it is worth wondering whether VD supplementation is truly necessary. Recent publications have been pointing at this possibility. We expect that future scientific evidence will resolve these questions.
CONCLUSIONS
Our study evinces that vitamin D deficiency is very prevalent in our region when the currently accepted cut-off levels are applied. Immigrants, females and adolescents are at higher risk of having this deficiency, especially when all three factors are present.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: VD: vitamin D.
REFERENCES
- Alonso López C, Ureta Velasco N, Pallás Alonso CR, Grupo PrevInfad Infancia y Vitamina D profiláctica. Rev Pediatr Aten Primaria. 2010;12:495-510.
- Rosen CJ. Vitamina D Insufficiency. N Engl J Med. 2011;364:248-54.
- Manson JE, Mayne ST, Clinton SK. Vitamin D and prevention of cancer: Reddy for prime time? N Engl J Med. 2011;364:1385-7.
- Elamin MB, Abu Elnour NO, Elamin KB, Fatourechi MM, Alkatib AA, Almandoz JP, et al. Vitamin D and cardiovascular outcomes: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011;96:1931-42.
- Wang L, Manson JE, Song Y, Sesso HD. Systematic review: vitamina D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. 2010;152:315-23.
- Wagner CL, Taylor SN, Hollis BW. Does vitamin D make the World go “round”? Breastfeed Med. 2008;3:239-50.
- Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142-52.
- Holick MF, Chen TC. Vitamin D deficiency: a wordwide problem with health consequences. Am J Clin Nutr. 2008;87:1080S-6S.
- Martínez Suárez V, Moreno Villares JM, Dalmau Serra J, Comité de Nutrición de la Asociación Española de Pediatría. Recomendaciones de ingesta de calcio y vitamina D: posicionamiento del Comité de Nutrición de la Asociación Española de Pediatría. An Pediatr (Barc). 2012;77:57.e1-e8.
- Merino Moína M, Grupo PrevInfad. Prevención del cáncer de piel y consejo de protección solar. In: PrevInfad (AEPap)/PAPPS infancia y adolescencia [online] [consulted on 05/09/2016]. Available in www.aepap.org/previnfad/pdfs/previnfad_fotoproteccion_rec.pdf
- Vitamin D supplementation: recommendations for Canadian mothers and infants. Paediatr Child Health. 2007;12:583-98.
- Silva Rico JC, Silva Higuero N. Raquitismo carencial y otras formas de raquitismo. Pediatr Integral. 2011;XV:654-68.





