Vol. 18 - Num. 69
Original Papers
Salmonella serovar Poona outbreak in a nursery
María del Mar Andreu Romána, Marta Allué Tangob, Clara Berbel Hernándezb, Irene Andrés Garcíac
aSubdirección General de Promoción de la Salud y Epidemiología. Ministerio de Sanidad, Servicios Sociales e Igualdad. Madrid. España.
bSección de Epidemiología. Servicio Territorial de Sanidad y Bienestar Social de Valladolid. Valladolid. España.
cServicio de Medicina Preventiva y Salud Pública. Hospital Clínico Universitario de Valladolid. Valladolid. España.
Correspondence: MM Andreu. E-mail: mandreu@msssi.es
Reference of this article: Andreu Román MM, Allué Tango M, Berbel Hernández C, Andrés García I. Salmonella serovar Poona outbreak in a nursery. Rev Pediatr Aten Primaria. 2016;69:35-43.
Published in Internet: 30-03-2016 - Visits: 19234
Abstract
Introduction: during the first three months of 2011, a gastroenteritis outbreak caused by Salmonella poona was described in one of the Valladolid´s nurseries.
Objectives: to describe the epidemiologic characteristics of the outbreak, its relation between a supracommunity outbreak and its transmission mechanism.
Methods: a descriptive bidireccional study. Starting from an index case a database from the nursery of the children records, the pediatrics and the microbiology records was done. The overall attack rate and the epidemic curve from each classroom was calculated.
Results: thirteen cases between five months and five years old were found; all of them were asymptomatic. The overall attack rate was 28,2% without significant difference between the classrooms. Salmonella poona 13,22:z:1,6 was found, and it was identical to that isolated in the national outbreak.
Conclusions: it seems that the nursery´s outbreak was caused by the same organism related to the supracommunity outbreak and the powdered infant formula was the vehicle involved in the transmission and it allowed the introduction of the organism in the nursery spreading through other pathways between students.
Keywords
● Epidemic outbreak ● Gastroenteritis ● Nursery ● Powdered infant formula ● Salmonella poonaINTRODUCTION
Diseases transmitted by the faecal-oral route have given rise to food-related outbreaks on numerous occasions. The literature also provides numerous examples of outbreaks in which primary cases caused by the consumption of a food lead to secondary cases transmitted by the faecal-oral route in specific population subsets.1
Salmonella is one of the most frequent causes of foodborne gastroenteritis. Within this genus, Salmonella enterica serotype poona is one of the more than two thousand Salmonella serotypes that cause disease in humans.2,3 It belongs to group G in the Kauffman-White classification and its antigenic formula is 13,22:z:1,6. It is an infrequent serotype, both in Spain4 and in countries with a similar level of development in health care. In the United States, it accounted for 1% of human Salmonella isolates reported in 2001.
Some outbreaks of S. poona associated to consumption of cantaloupe have been described in the scientific literature,5 but so far there was no known outbreak of S. poona in infants related to consumption of a powdered infant formula.4 We know of outbreaks in infants with different transmission routes, such as the one documented in a neonatal unit in the United States whose point source was an infected mother.1
Although there are sterile, liquid, ready-to-use artificial formulas in the market, powdered formulas continue to be the type used most frequently to feed infants. These powdered products are not sterile and may be contaminated with pathogens due to improper manufacturing, storage, or handling conditions. Salmonella enterica and Enterobacter sakazakii are the microorganisms that pose the highest risk of contamination.4,6
In the past few years, Salmonella serotypes other than S. poona have caused outbreaks in infants associated with the consumption of artificial formula, some of them in Spain. Thus, there have been reports of outbreaks by S. ealing (United Kingdom, 1985), S. tennessee (United States and Canada, 1993), S. virchow (Spain, 1994), S. anatum (United Kingdom and France, 1996–1997), S. london (Korea, 2000), S. agona (France, 2004-2005), S. give (France, 2008) and S. kedougou (Spain, 2008). Most of these outbreaks were detected because the implicated Salmonella strains were atypical.4,7–9
In the context of an outbreak of supracommunity interest (affecting more than one of Spain’s autonomous communities) of Salmonella poona that occurred in Spain in 2010, involved infants4 (33 cases were reported in Valladolid) and was associated with the consumption of a specific lot of one brand of powdered formula, we found a group of cases that were linked by attending a nursery where there had been an initial case, an infant aged 5 months, that was the only one with exposure to the artificial formula that was the suspected source of infection.
Our objectives in this study were to describe the epidemiological characteristics of an outbreak of Salmonella poona in a nursery and its relationship with the outbreak of supracommunity interest in Spain, and to analyse the transmission mechanism that led to the infection of older children that had not been exposed to the artificial formula that was believed to be contaminated.
MATERIALS AND METHODS
Type of study: bidirectional (retrospective and prospective) descriptive study.
Case definition: individual with a stool culture positive for Salmonella in the first five months of 2011, with or without symptoms and with an epidemiological link to the nursery.
Epidemiological investigation
Since January 2011, the Section of Epidemiology of the Servicio Territorial de Sanidad (Territorial Service of Health) of Valladolid collaborated in the investigation of the outbreak of supracommunity interest of acute gastroenteritis (AGE) due to Salmonella poona in infants.
The case of a girl aged 5 years with AGE due to Salmonella poona caught our attention, as this was an atypical causative agent, and led to us focusing on several cases in non-infant children that seemed to have no epidemiological relationship to the contaminated formula that had been identified as the potential source of infection. Starting from this case, we investigated its personal characteristics and found that this girl had a 13-month-old brother that had not had any clinical manifestations of gastroenteritis and had not consumed the suspected artificial formula. However, this boy attended the same nursery as another infant diagnosed with AGE due to Salmonella poona.
Continuing the investigation, we found more cases related to the nursery. We reported our findings to the Section of Food Hygiene and Environmental Health of our Territorial Service, and they conducted an inspection of the facilities that revealed no irregularities.
We contacted the paediatricians of all the children enrolled in the nursery to perform a retrospective search for cases and to request stool cultures for any children that had shown symptoms of AGE during the outbreak period and also for asymptomatic children based on the judgment of the paediatrician.
At the time of the outbreak, a total of 39 children aged up to 3 years were enrolled in the nursery and distributed in the following groups: six infants, 14 toddlers aged 1 to 2 years, and 19 children older than 2 years. Four staff, all of them young women, were responsible for all the tasks in the nursery. The nursery had one bathroom for the older children and changing stations in the infant and toddler classrooms.
When it came to food handling, the nursery had a kitchen where the staff prepared blended foods for lunch. Children brought breakfast from their homes and the bottles were prepared as follows: children brought the bottles with the adequate amounts of water, the staff heated the bottles in the microwave, and then added powdered formula, and, if applicable, the cereal. Both formula and cereal containers were marked with the name of each child and had the corresponding dosing scoops inside.
We found evidence that one container from the lot of artificial formula suspected in the outbreak of supracommunity interest was used in the nursery; the container belonged to the 5-month-old girl that had shown symptoms first in the group of cases. When the staff became aware of the alert that had been issued, they removed the container.
Microbiological investigation
Twenty-four stool samples taken from children enrolled in the nursery and two from siblings that did not attend the centre were cultured. Salmonella was isolated from 13 out of the 26 stool cultures (11 corresponded to children enrolled in the nursery and 2 to siblings). All the Salmonella isolates were submitted to the Centro Nacional de Microbiología (National Centre of Microbiology [CNM]) for serotyping, and all were found to correspond to Salmonella serotype poona 13,22:z:1,6, with all isolates presenting the same patterns in pulse-field gel electrophoresis (PFGE). We have no data on their sensitivity to antimicrobials. We did not obtain samples from the container of suspected formula that had been used by the infected infant. Follow-up stool cultures were performed in nine cases.
Statistical analysis
We performed the basic calculations with the software Epidat® 3.1 and compared proportions by means of Fisher’s exact test.
RESULTS
We identified 13 cases, eight in males (61%) and five in females (39%), with ages ranging between 5 months and 5 years (mean, 21 months).
The clinical manifestations were those of AGE, usually mild (no cases required hospital admission), and the most frequent symptoms were liquid stools (in one case with blood), abdominal pain and fever. We did not identify any cases among the nursery staff or other adults in close contact with the cases.
Three of the thirteen cases were asymptomatic (23%). Table 1 summarises the main characteristics of the cases.
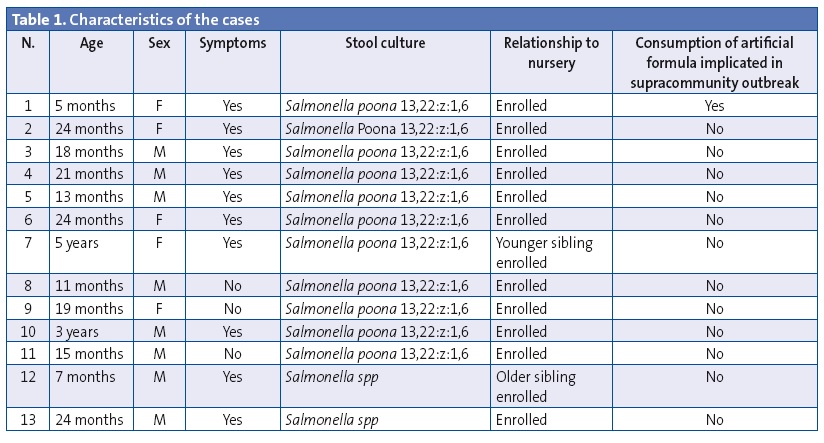
The attack rates were the following: overall attack rate, 28.2%; attack rate in the infant group, 33.3%; attack rate in the 1-2 year old group, 35.7%; attack rate in the older than 2 years group, 21.1%. The differences between the attack rates of the different groups were not statistically significant.
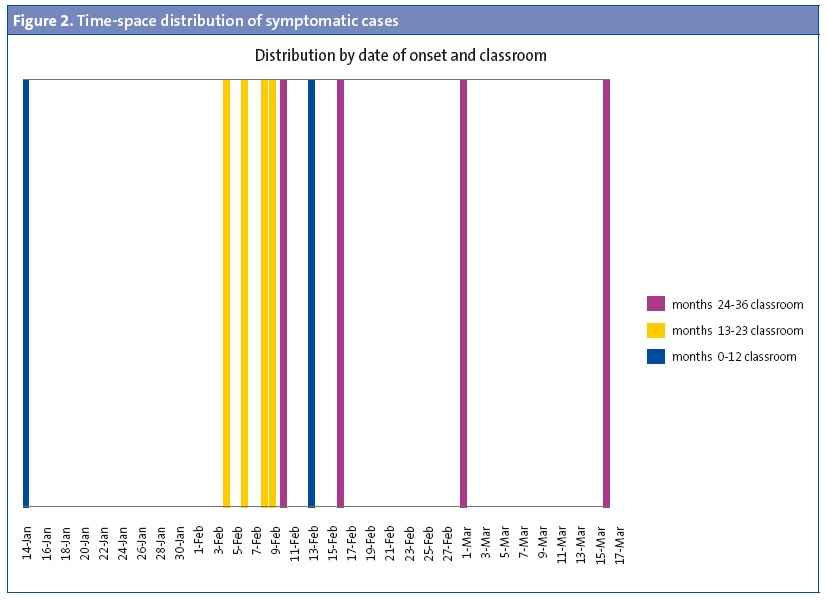
As for the temporal distribution of symptomatic cases (Figure 1), the dates of the onset of symptoms ranged between January 14 and March 16, 2011.

The first case was that of the infant that was taking the artificial formula associated with the supracommunity outbreak. When we analysed the distribution in space and time of symptomatic cases by classroom, we included the two children that did not attend the nursery in the classrooms of their respective siblings. Figure 2 shows the temporal distribution of cases by classroom.
The results of follow-up stool cultures showed that at least 56% continued to be positive for Salmonella 46 days after the onset of symptoms.
DISCUSSION
Salmonella serotyping is an important tool in epidemiological surveillance, as it not only allows the assessment of the outcomes of control measures applied to animal and food sources of infection, but also the detection of trends and shifts. It is also used to identify sources of infection and person-to-person routes of transmission and to develop new interventions and control measures.
Although a great number of Salmonella strains have been described, most infections in humans are caused by a few of them.
In the 2010–2012 period, S. enteritidis and S. typhimurium accounted, respectively, for 43% and 24% of all serotyped isolates in countries of the European Union and the European Economic Area (EEA), while significant shifts in the serotype distribution were observed in the same period. The prevalence of some serotypes increased due to outbreaks, such as a S. thompson outbreak in the Netherlands in 2012 associated with the consumption of smoked salmon, a multinational outbreak of S. stanley between August 2011 and January 2013 linked to contamination in the manufacturing process of turkey products; and a S. panama outbreak in Germany and Italy linked to the consumption of contaminated pork products.10
The prevalence of Salmonella enterica poona increased due to the outbreak in Spain, and precisely due to the fact that this strain is very rare in our country, and as happened in similar outbreaks caused by atypical pathogens,9,11 microbiology laboratories and epidemiological surveillance departments played an essential role in detecting an outbreak that could otherwise have gone unnoticed.
The epidemiological, clinical and microbiological investigation allowed us to link an apparently sporadic case of gastroenteritis due to this pathogen in a school-aged girl with a supracommunity outbreak of Salmonella poona in infants, and to discover the existence of an outbreak caused by the same organism in a nursery.
There is epidemiological evidence, supported by a case and control study conducted by the Centro Nacional de Epidemiología (National Centre of Epidemiology), that consumption of the powdered artificial formula was the source of infection in the infants affected by the outbreak of supracommunity interest.4
In outbreaks caused by Salmonella, transmission mainly occurs through the consumption of contaminated foods. Person-to-person transmission through the faecal-oral route is also significant, especially in the presence of diarrhoea,12-15 and cross-contamination during the handling of powdered artificial formulas has been previously described in the literature.4,7 Furthermore, the ways in which reconstituted formula is stored and preserved may allow rapid bacterial growth, amplifying a previously low level of contamination.7 Secondary person-to-person transmission of diseases initially linked to the consumption of contaminated food or water has also been described in outbreaks caused by other enteropathogens.16
In this case, we think that the outbreak started in the nursery with an infant that was being fed one of the brands of formula implicated in the outbreak of supracommunity interest. The fact that this girl was the only one among all the children that attended the nursery that had consumed contaminated formula and the temporal and spatial distribution of cases suggest that she was the point source from which Salmonella spread to the other children by the faecal-oral route or possibly by cross-contamination during food preparation in the kitchen of the nursery. The disease even reached two siblings of children enrolled in the nursery that did not attend it.
The intrafamilial transmission of intestinal pathogens has been well documented, and it is known that if a member of the family is infected, up to one third of family close contacts may be infected too,13 with transmission rates varying depending on the causative pathogen.17-19 Our index case, the school-aged girl, had an asymptomatic brother that attended the nursery and that connected her epidemiologically to the outbreak in that facility. Similarly, the contagion of an infant that did not consume the contaminated formula nor attended the nursery can be explained by having a brother that did attend it, with both the infant and the brother having stool cultures positive for Salmonella.
It is likely that more individuals, including adults, were affected by this outbreak and were not identified due to various reasons:
- An initially unexpected change in the mechanism of transmission.
- The nonspecific and/or mild nature of symptoms in some cases, as well as the presence of asymptomatic cases. Due to these reasons, it is possible that some of the affected individuals did not seek medical care, and that among those that did, some would not have had a stool sample collected for culture, and therefore would not have met the criteria for the definition of a case. This is not an unusual occurrence, even in infants, a population that receives medical care more often, 4 or in very sophisticated paediatric hospitals.7
- The fact that this was a relatively small outbreak, with cases that seemed sporadic and which were managed by different paediatricians at different times, made it difficult to establish a connection between them. Based on the literature, it is precisely small outbreaks that are most likely to go undetected, even though in theory they are much more frequent than massive outbreaks, especially in small groups of people, such those in a nursery or a family, that are exposed to the same source of infection.18
In our study, at least 56% of patients continued to have positive stool cultures 46 days after the onset of symptoms. It is well known that intestinal infections by Salmonella tend to be protracted in children, who continue to shed this organism in their faeces in the absence of clinical manifestations for longer periods than adults.11 A study conducted in Sweden on a group of children aged 0 to 5 years showed that 18% of them continued to shed Salmonella bacteria twelve weeks after an episode of gastroenteritis, and 4% continued for six months.20,21
We believe that the work of paediatricians in raising awareness and educating parents, as well as the collaboration of the parents and the nursery staff, contributed to containing the spread of the outbreak. Furthermore, the active retrospective search for cases allowed the identification of possible sources of infection, which in turn allowed the implementation of appropriate preventive measures.
Some of the limitations of the study were the inability to collect stool culture samples from the nursery staff and of performing follow-up stool cultures in all clinically significant cases. The study may also be affected by recall bias, as the information for some of the cases was collected long after they had happened.
To conclude, it seems evident that the outbreak in the nursery was caused by the same pathogen that had caused the outbreak of supracommunity interest, and that the artificial formula implicated in that outbreak was the source of infection that brought the pathogen into the nursery, which then was transmitted by other routes among the children that attended the centre.
It is important that cases of AGE in young children are monitored closely, especially if they attend nurseries or other types of indoor facilities. Combined with appropriate diagnostic testing, this would allow the early identification of a potential outbreak and the implementation of the measures required to manage and control it.
This kind of outbreak calls our attention to the importance of adequately managing children in nurseries, with particular emphasis on the basic hygiene and food handling measures that should be universally implemented, keeping in mind the possibility of asymptomatic cases that work as sources of infection.
One such measure is the correct handling of infant formulas, emphasising the importance of handwashing, safe storage conditions, and the health education of parents and caregivers.
We also want to underscore the need for professionals and all involved sectors to make a concerted effort to prevent this disease, while keeping in mind the importance of strict adherence to food safety legislation.
In order to implement preventive measures to reduce the incidence of this disease, it is essential that we understand its epidemiology and microbiology, as is maintaining surveillance systems that can detect the emergence of atypical Salmonella strains and issue the corresponding alerts.
FUNDING
We conducted this study with the resources that are generally available to the Section of Epidemiology of the Servicio Territorial de Sanidad y Bienestar Social (Territorial Service of Health and Social Welfare) of Valladolid for the study of outbreaks.
CONFLICT OF INTERESTS
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: AGE: acute gastroenteritis • CNM: Centro Nacional de Microbiología (National Centre of Microbiology) • EEA: European Economic Area • PFGE: pulse field gel electrophoresis.
ACKNOWLEDGMENTS
We want to thank the disinterested help of the paediatricians of affected children in the Basic Health Areas of Valladolid Rural II, Parque Alameda-Covaresa and Arturo Eyríes in collecting the necessary data to study the outbreak.
We are also grateful for the collaboration of parents and the nursery staff, who were very helpful in controlling the outbreak and helping us obtain the information we needed to study it.
We also thank María del Sol Granados Alonso, for her help with translating and her contributions to the writing of this article.
BIBLIOGRAFÍA
- Stone A, Shaffer M, Sautter RL. Salmonella poona infection and surveillance in a neonatal nursery. Am J Infect Control. 1993;21:270-3.
- Jackson BR, Griffin PM, Cole D, Walsh KA, Chai SJ. Outbreak-associated Salmonella enterica serotypes and food Commodities, United States, 1998-2008. Emerging Infect Dis. 2013;19:1239-44.
- National Salmonella surveillance annual summary, 2009. In: Centers for Disease Control and Prevention [online] [consulted in 30/03/2016]. Available in cdc.gov/ncezid/dfwed/PDFs/SalmonellaAnnualSummaryTables2009.pdf
- Centro Nacional de Epidemiologia. Brote supracomunitario de gastroenteritis por Salmonella Poona en 2010-2011. Bol Epidemiol Sem. 2012;19:176-85.
- Multistate outbreaks of Salmonella serotype Poona infections associated with eating cantaloupe from Mexico, United States and Canada, 2000-2002; 2002. In: Centers for Disease Control and Prevention [online] [consulted in 30/03/2016]. Available in cdc.gov/mmwr/preview/mmwrhtml/mm5146a2.htm
- Vargas-Leguás H. Guía para la elaboración de fórmulas infantiles en polvo en el medio hospitalario. Sistema de análisis de peligros y puntos de control crítico. An Pediatr (Barc). 2009;70:586-93.
- Cahill SM, Wachsmuth IK, Costarrica ML, Ben Embarek PK. Powdered infant formula as a source of Salmonella infection in infants. Clin Infect Dis. 2008;46:268-73.
- Juncosa Morros T, Palacín Camacho E, Latorre Otín C. Salmonelosis en un hospital materno-infantil de Barcelona durante diez años (1992-2001). An Pediatr (Barc). 2005;63:403-8.
- Centro Nacional de Epidemiologia. Brote supracomunitario por Salmonella enterica serotipo Kedougou en niños asociado al consumo de una leche maternizada, España, 2008. Bol Epidemiol Sem. 2008;16:97-8.
- Surveillance of seven priority food- and waterborne diseases in the EU/EEA 2010-2012. In: European Centre for Disease Prevention and Control [online] [consulted in 30/03/2016]. Available in http://goo.gl/BBsOAQ
- Usera MA, Rodriguez A, Echeita A, Cano R. Multiple analysis of a foodborne outbreak caused by infant formula contaminated by an atypical Salmonella virchow strain. Eur J Clin Microbiol Infect Dis. 1998;17:551-5.
- Gil-Setas A. Salmonelosis no tifoidea en un Área de Salud de Navarra, España. Rev Esp Salud Pública. 2002;76:49-56.
- Bennett JE, Dolin R, Blaser MJ. Mandell, Douglas y Benett. Enfermedades infecciosas. Principios y práctica. Madrid: Elsevier; 2002.
- Yáñez Ortega JL, Carramiñana Martínez I, Bayona Ponte M. Brote por Salmonella enteritidis en una residencia de ancianos. Rev Esp Salud Pública. 2001;75:81-8.
- Centro Nacional de Epidemiologia. Infecciones por Salmonella no tifoidea de origen humano en España. Sistema de Información Microbiológica. Años 2000-2008. Bol Epidemiol Sem. 2009;17:193-6.
- Pere Godoy RB. Brote de gastroenteritis por el consumo de agua de suministro público causado por Shigella sonnei. Gac Sanit. 2011;25:363-7.
- Tandé D, Boisramé-Gastrin S, Münck MR, Héry-Arnaud G, Gouriou S, Jallot N, et al. Intrafamilial transmission of extended-spectrum-beta-lactamase-producing Escherichia coli and Salmonella enterica Babelsberg among the families of internationally adopted children. J Antimicrob Chemother. 2010;65:859-65.
- Ethelberg S, Olsen KEP, Gerner-Smidt P, Mølbak K. Household outbreaks among culture-confirmed cases of bacterial gastrointestinal disease. Am J Epidemiol. 2004;159:406-12.
- Wilson R, Feldman RA, Davis J, LaVenture M. Salmonellosis in infants: the importance of intrafamilial transmission. 1982;69:436-8.
- Svenungsson B, Goffe G. Persistent excretion of Salmonella in foreign-born adopted and native Swedish children. Scand J Infect Dis. 1990;22:37-42.
- Berezin EN, Carvalho Eda S, Farhat CK, Mimica IM, Mimica L, Raphaelian TA. Persistence of colonization time in patients infected by Salmonella. AMB Rev Assoc Med Bras. 1990;36:100-6.





