Vol. 18 - Num. 69
Original Papers
Who performs health checks in the Valencian Autonomous Community? Improvement proposals
Javier Soriano Fauraa, Carlos Labordena Barcelób, M.ª Dolores Gutiérrez Siglerc, Elena Fabregat Ferrerd, Julia Colomer Revueltae, Francesc Bargall Lleonartf
aPediatra. CS Fuensanta. Valencia. España.
bPediatra. CS Fernando el Católico. Castellón. España.
cPediatra. CS Nou Molés. Valencia. España.
dPediatra. CS Gran Vía. Castellón. España.
eDepartamento de Pediatría, Obstetricia y Ginecología. Unidad de Pediatría. Universidad de Valencia. Valencia. España.
fPediatra. CS Almenara. Castellón. España.
Reference of this article: Soriano Faura J, Labordena Barceló C, Gutiérrez Sigler MD, Fabregat Ferrer E, Colomer Revuelta J, Bargall Lleonart F. Who performs health checks in the Valencian Autonomous Community? Improvement proposals. Rev Pediatr Aten Primaria. 2016;69:17-24.
Published in Internet: 30-03-2016 - Visits: 19312
Abstract
Introduction: our main objective was to determine the overall pediatric nursing coverage on the Well Child Care (WCC) visits and the secondary objective was to assess acceptance, skills and training needs of pediatrics and nursing teams in Primary Care of the Comunitat Valenciana.
Material and methods: cross sectional descriptive study from data collected through anonymous online surveys to pediatricians and nurses for two months in 2014. They were asked about who performs and who should perform and abilities and training needs identified.
Outcomes: among those responding to the survey, 87% have referred to have pediatric nursing at their offices. 70% WCC visits have been delivered jointly by pediatrician and nurse. Main nursing abilities have been considered: advice on feeding, healthy lifestyle and immunizations. Half of the respondents recognize training needs. 95% surveyed believe that it’s mandatory to have pediatric nurses in all primary care settings. One out of four visits performed by pediatricians alone corresponds to early visits along the first month of life.
Conclusions: all Primary Care Units should be formed of pediatricians and nursing staff. The nursing work schedules must be flexible enough to enable their participation in the first WCC visits. In continuing education programs, the contents should be implemented according to the needs identified in this study for the performance of the activity in the WCC.
Keywords
● Child Health ● Pediatric nurse practitioners ● Primary preventionINTRODUCTION
Spanish society has experienced significant sociodemographic, economic and cultural changes since the creation of the first health care centres in the 1980s, when paediatricians were incorporated into primary care teams. Since then, and with the implementation of the Well Child Care programme (WCC) in the different autonomous communities, we have achieved significant advances in child disease prevention and health promotion. It has been one of the programmes most widely accepted by health care users, and there is widespread agreement by health professionals as regards its benefits, although there is no evidence demonstrating a measurable positive impact on health of most of the services it comprehends.1 The WCC programme provides an excellent opportunity to become acquainted with children, their families and their quality of life, and is an ongoing and valuable process of disease prevention and health promotion.
Well child care visits provide the appropriate framework to approach issues related to development, behaviour, learning and psychosocial health. All of these aspects have gained relevance due to the higher morbidity associated with increases in the prevalence of chronic diseases and disabilities in children, the heterogeneity of family structures, lifestyle changes in developed countries, and higher expectations from families and society at large.
These circumstances have led to an increase in the complexity of primary care services, faced with strong determination by paediatric teams in primary care (PC) as a health care and organisational challenge in the absence of investment by the Health Care Administration.
We are aware that the number of recommended services has grown significantly and far exceeds what can be accomplished in an average visit. This may be one of the factors contributing to the wide variability in the quality and quantity of services offered.3 We observe that not all the needs of families are addressed, that they leave clinics with unresolved concerns or issues they were unable to bring up, and that sometimes even screenings for the early detection of developmental delays are not performed. Despite the efforts of health professionals, with the system as it is set up today, the opportunity offered by the WCC programme is wasted, and families do not receive all the support and care they need to ensure that their children develop to their full potential.
Based on these shortcomings, identified by PC centres, we reviewed the scientific literature available on the subject, and while we found no original studies conducted in Spain, we observed that the same concerns exist in other countries such as the United States, where paediatricians that work in the PC system face similar circumstances and a shortage of physicians. Researchers and clinicians have proposed alternatives to improve care, focusing on changes in structural elements of care, such as personnel and care organization.4 These changes include the performance of services by nursing staff with a high degree of autonomy, and offering non-conventional formats of care delivery, such as group WCC visits or the incorporation of new communication technologies to offer advice, anticipatory guidance, and health education.
OBJECTIVES
The main objective of our study was to determine the participation and autonomy of paediatric nurses in the WCC programme in health care centres of the Autonomous Community of Valencia.
Our secondary objectives included analysing the acceptance, qualifications, skills and training needs of paediatric teams in relation to the WCC checkups performed in the Autonomous Community of Valencia.
MATERIALS AND METHODS
We conduced a cross-sectional, descriptive and nonrandomised study by means of an online anonymous and self-administered questionnaire sent to paediatricians and nurses in the Autonomous Community of Valencia.
The population of paediatricians and nurses that provide primary care for children is estimated at 1200, based on data from 2008,5 and we calculated a sample size of 221 for a confidence interval (CI) of 90% and a prevalence of 50±5% for the primary outcome variable: the staffing of paediatric nurses in health care centres.
We recruited participants by accessing the distribution lists of the Nursing Boards of the Autonomous Community of Valencia, the Paediatrics Associations of the three provinces, and the list of primary care health centres of the province of Valencia.
We designed the online questionnaire as a Google Docs ®< format. The contents of the questions were agreed on by the professionals of the Group for Technical Consulting in Primary Care Paediatrics (Grupo Asesor Técnico para la Pediatría de Atención Primaria [GATap]). Following the recommendations found in the scientific literature, we defined four domains for study in the questionnaire that fit the proposed objectives:
- The staffing of paediatric nurses in health care centres.
- Health checkups performed by only the nurse or the paediatrician.
- Degree of acceptance, qualifications and competence, as judged by paediatricians and nurses.
- Training needs identified by paediatricians and nursing staff.
We collected data between April 22 and June 20, 2014. We did a statistical analysis of the obtained data with the SPSS+ v.15.0® software, including a descriptive and inferential statistics, contingency tables, calculation of c2, risk estimates, and odds ratios (ORs) with a 95% CI.
RESULTS
We obtained responses from 253 providers, with a higher proportion of paediatricians (65%; n= 175) compared to nurses (35%; n = 78). A little more than three quarters of the respondents (210) worked in health care centres, and a lower proportion worked in auxiliary ambulatory clinics (26), private clinics (11) and hospitals (6). Of all respondents, 87% reported that the facility where they worked had specialised paediatric nurses on staff.
The proportion of professionals that worked in the province of Valencia was 65% (164), while 21% worked in Castellón (52) and 15% in Alicante (37).
Who performs the health checkups?
More than 70% of the respondents reported that health checkups were performed jointly by a paediatrician and nurse.
Approximately one in four checkups performed by paediatricians alone corresponded to the first neonatal visits at one week and one month post birth.
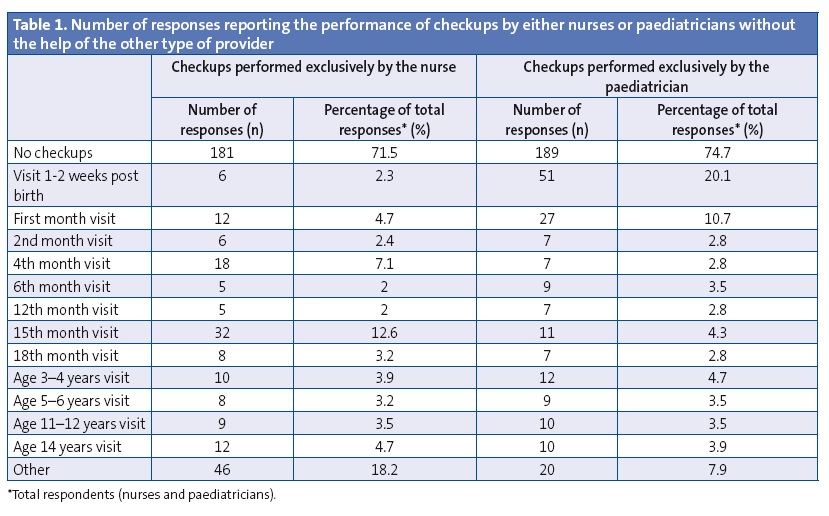
The 15-month visit was the one most frequently performed by nurses alone, and 18.2% of nurses attended other visits that were not included in the official programme (Table 1).
Who should perform health checkups?
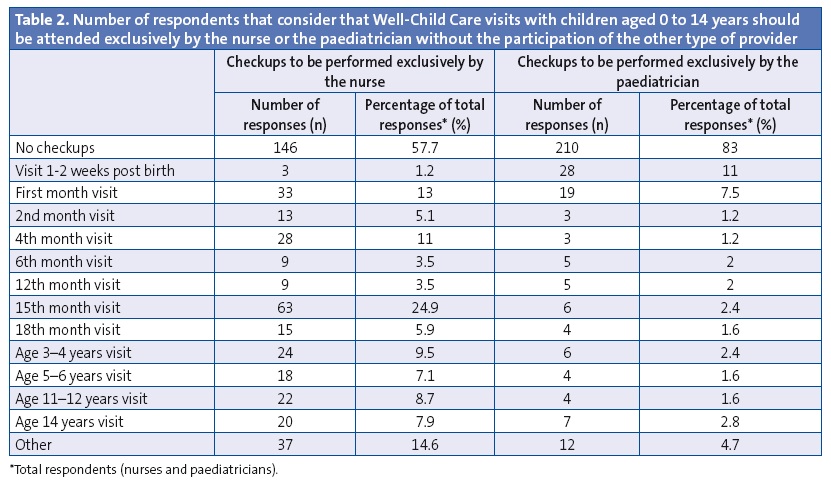
According to 57.7% of respondents, a nurse should never perform any of the checkups alone (without the participation of a paediatrician). Also, 83% of respondents considered that paediatricians should not do any checkups without the help of a nurse.
In agreement with the customary practice described in the paragraph above, the visits that respondents considered could be attended by a single provider were the first neonatal visit (with the paediatrician) and the 15-month visit (with the nurse) (Table 2).
Current skills of nurses and further training needed to perform health checkups
Table 3 offers a comparison of the various skills that respondents consider nurses currently have to perform in health checkups and the areas in which further training is needed.
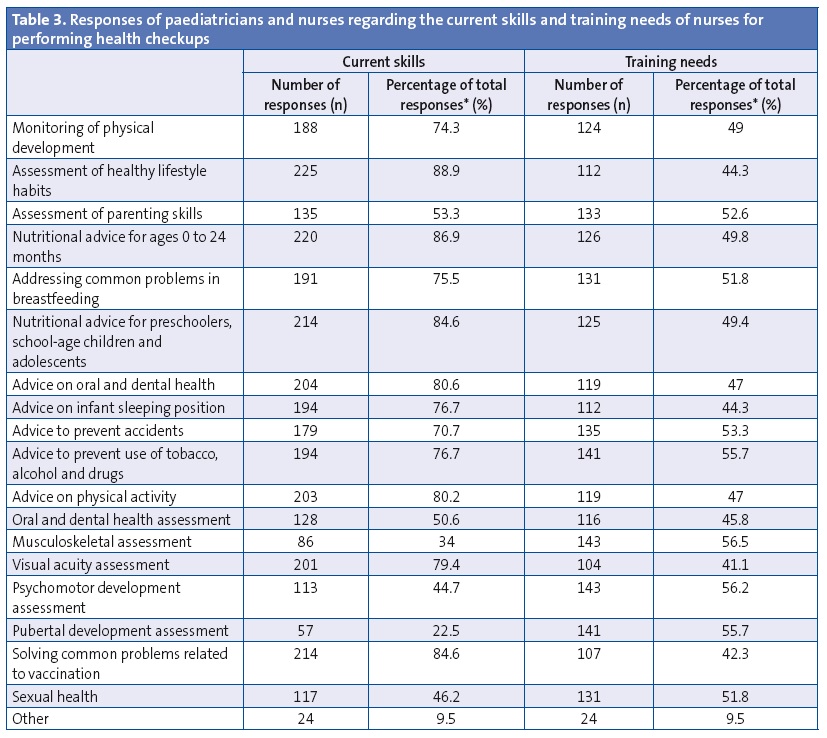
When it came to the areas in which respondents considered nurses were already skilled, the highest percentages corresponded to the assessment of healthy lifestyle habits (88.9%), providing advice (especially on nutrition), and solving common problems related to vaccination. However, the assessment of their current skills was below 50% when it came to performing examinations, except for the assessment of visual acuity, at which approximately 80% of respondents considered they were skilled.
When it came to areas requiring further training, nearly 50% of the respondents reported gaps in training for the 19 types of activities listed, with no marked differences between them.
Need for specialised paediatric nursing staff
Nearly all respondents expressed the need to have specialised paediatric nurses on staff (95%; n = 241). Paediatricians were 3.3 times more supportive of the role of the paediatric nurse than nurses (95% confidence interval [CI], 1.02–0.9; P = .041).
The centres that had paediatric nurses on staff were more likely to express the need for these professionals (OR, 12.09; 95% CI, 5.55–40.97).
In centres that did not have paediatric nurses on staff, the paediatrician was more likely to perform some of the health checkups alone, without the help of a nurse. Having a paediatric nurse on staff was identified as a protective factor for the paediatrician-nurse collaboration in performing health checkups (OR, 0.47; 95% CI, 0.19–0.95).
Paediatricians that did not usually perform health checkups in collaboration with a nurse disagreed more frequently with having a nurse perform them alone without their help (OR, 0.43; 95% CI, 0.24–0.78).
Nurses that usually performed health checkups in collaboration with the paediatrician stated more frequently that they should perform these checkups in collaboration with the paediatrician (OR, 7.16; 95% CI, 3.84–13.36).
DISCUSSION
The data we obtained showed that there was room for improvement in paediatric nurse staffing, as it currently is below 90%.
On the other hand, there is practically unanimous agreement that nurses should be integrated in paediatrics teams: 95% of respondents considered this issue important, and this model is considered essential by respondents from facilities where it is already established, in whom the probability of supporting the “paediatrician-nurse dyad” model was greater than 12 (OR, 12.09; 95% CI, 5.5–40.97).
As for the autonomy of nurses in the WCC programme, our findings showed that both types of professionals participated in nearly all checkups. Human resources were not organised with the aim of offering better coverage in psychosocial, educational and development-related services. Consistent with this finding, and possibly at its root, we found that there was only moderate agreement, amounting to nearly 43% of respondents, that nurses should perform some health checkups without the collaboration of a paediatrician. A slightly higher percentage, 52%, would support a change in the current model by which some of the health checkups would be performed exclusively by nurses.
We found considerable disagreement (83%) with the paediatrician performing some health checkups without the collaboration of a nurse, especially when it came to the health checkups performed at week one and month one post birth.
As for the current skills and training needs of the teams, our findings support the notion that nurses have sufficient skills to fulfil the tasks involved in health checkups. We also find agreement among respondents, ranging between 70% and 89% depending on the specific skill area we asked about, that nurses have the required skills to perform many of these tasks. This is not to say that efforts should not be made to improve or update training in screening, counselling and intervention in the context of health checkups, especially in the areas of the musculoskeletal system, puberty and addictive behaviours.
The scientific literature in English has made references to the figure of the paediatric nurse since the mid-1970s, over forty years ago, which was well received by families and was associated with increased care in the areas of behavioural disorders and psychomotor development. More recent studies have shown comparable health outcomes, and support expanding the responsibilities of nurses in primary care.6,7 Nursing professional associations have been advocating for increased autonomy for nurses, the acknowledgment of their contribution to care, and greater social visibility, and demand the support of organisations and physicians.8 In this regard, individualized nursing schedules allow the user to identify his or her primary nurse, and offer an access to services alternative to the paediatrics office, which until recently was the sole possible gateway for administrative services as well as referrals, on-demand visits, scheduled checkup or followup visits, the WCC programme, etc.
By 2010, the year that the Boletín Oficial del Estado (Official State Gazette [BOE]) published the Education Curriculum for the Paediatric Nursing Specialty (Order SAS/1730/2010, of June 17), which included extensive competencies in the WCC programme, the figure of the paediatric nurse was already widely established in actual practice, reaching 80% or more in twelve autonomous communities, including the Autonomous Community of Valencia.9
The literature we reviewed was consistent on the point that WCC visits could be performed by especially trained nurses working in collaboration with paediatricians. Nurses may have or acquire the necessary skills to correctly implement almost the entire WCC programme. The paediatrician must, at minimum, evaluate children at key points of their development and be informed by the nursing staff of any identified issues to ensure that they are properly addressed.
Our concern with how to provide a comprehensive visit comprising all services described in this article to our population was also expressed in the scientific literature, and we found that innovative models have been proposed that integrate a wide variety of health care providers. They most frequently involve nurses at the helm of teams completed by social workers or early childhood educators.10
The delivery of care in formats other than the conventional individual face-to-face visit has also been explored, for example, group preventive visits (group WCC), which proved to be at least as effective as individual visits, providing a broader array of services without increasing the time spent by providers. Group visits allow a family-centred educational approach, with increased participation of parents, for instance, and the added value contributed by other professionals. Group visits usually comprise four to five families4
In other developed countries, care delivery does not fall exclusively on primary care centres, but there are schools with varying budgets that carry out activities in areas such as nutritional advice, substance use counselling, mental and developmental health, and oral and dental health.11
“The structure and organization of health care centres must provide the time and physical space required for the team work and the separate activity of paediatricians and nurses; a model based on cooperation and complementation.”5 As the development of this collaborative model progresses, the WCC programme will be revitalised, with improvements in its quality and cost-effectiveness and providing the flexibility required to reach the most disadvantaged populations, balance out inequalities, and pursuing equity.12
Some of the limitations to the generalisation of this study have to do with the non-random sampling of the respondents, the lower representation in the sample of nurses compared to paediatricians, and the unequal distribution of the sample by province, with a lesser participation of PC centres in Alicante.
Based on the results we obtained and despite the aforementioned limitations, we consider that the basic care unit in paediatrics in every health care centre should consist of a nurse and paediatrician.
We need studies to help us identify current barriers and potential solutions to make the use of human resources in the WCC programme efficient, efficacious and effective, avoiding duplications of services.
RECOMMENDATIONS
- All care units involved in the Well Child Care Programme should be comprised of paediatricians and nurses.
- Nurse appointment schedules should be more flexible to allow for their participation, along with paediatricians, in the health checkups at 1 week and 1 month post birth.
- Continuing education programmes for nurses should include contents fitting the needs identified in this study for the development of their activity in the WCC programme. Expanding the training of nursing professionals would increase not only the acceptance of this model by paediatricians, but also the confidence of nursing staff in the performance of these tasks.
- We propose to bring to debate in the appropriate forums—professional associations, child health technical services, etc—which WCC checkups should be performed by nurses alone, and which by nurse-and-paediatrician teams.
CONFLICT OF INTERESTS
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: ACV: Autonomous Community of Valencia • CI: confidence interval • GATPap: Grupo Asesor Técnico para la Pediatría de Atención Primaria (Group for Technical Consulting in Primary Care Paediatrics) • OR: odds ratio • PC: primary care • WCC: Well Child Care
BIBLIOGRAFÍA
- Galbe Sánchez-Ventura J. ¿Son eficaces las revisiones de salud de los niños? Evid Pediatr. 2008;4:47.
- Ruiz-Canela Cáceres J. El modelo de Pediatría de Atención Primaria. Rev Pediatr Aten Primaria. 2010;12:s139-s148.
- Belamarichi PF, Gandica R, Stein RE. Drowning in a sea of advice: pediatricians and American Academy of Pediatrics Policy Statements. 2006;118:4e964-e978.
- Coker TR, Windon A, Moreno C, Schuster MA, Chung PJ. Well-child care clinical practice redesign for young children: a systematic review of strategies and tools.2013;131:S5-25.
- Sistema Nacional de Salud España 2010. Principales datos y cifras de la Sanidad Española. Anexo 4. In: Ministerio de Sanidad y Política Social [online] [consulted in 29/03/2016]. Available in gob.es/organizacion/sns/docs/sns2010/Sistema_Nacional_de_Salud_2010.pdf
- Domínguez Aurrecoechea B, Valdivia Jiménez C. La Pediatría de Atención Primaria en el sistema público de salud del siglo XXI. Informe SESPAS 2012. Gac Sanit. 2012;26:82-7.
- Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Sustitución de médicos por enfermeras en la Atención Primaria (revisión Cochrane traducida). In: La Biblioteca Cochrane Plus [online] [consulted in 29/03/2016]. Available in: bibliotecacochrane.com/BCPGetDocumentForPrint.asp?DocumentID=CD001271
- Poghosyan L, Nannini A, Stone PW, Smaldone A. Nurse practitioner organizational climate in Primary Care settings: implications for professional practice. J Prof Nurse. 2013;29:338-49.
- Esparza Olcina MJ. ¿Quién hace qué en el Programa de Salud Infantil? In: AEPap (ed.). Curso de Actualización Pediatría 2011. Madrid: Exlibris Ediciones; 2011. p. 29-33.
- Yoshida H, Fenick AM, Rosenthal MS. Group well-child care: an analysis of cost. Clin Pediatr (Phila). 2014;53:387-94.
- Yeung LF, Shapira SK, Coates RJ, Shaw FE, Moore CA, Boyle CA, et al. Rationale for periodic reporting on the use of selected clinical preventive services to improve the health of infants, children, and adolescents - United States. MMWR Suppl. 2014 Sep 12;63:3-13.
- Newhouse RP, Stanik-Hutt J, White KM, Johantgen M, Bass EB, Zangaro G,et al. Advanced practice nurse outcomes 1990-2008: a systematic review. Nurs Econ. 2011;29:230-50.





