Vol. 17 - Num. 68
Original Papers
Intelectual disability of genetic cause. Observational study in an urban primary health care center
Montserrat Tirado Meleroa, ME Milagro Jiménezb, Y Romero Salasc, José Galbe Sánchez-Venturad, C Balagué Clemóse, G Zarazaga Gemesc, M Cebrián Gimenoc
aMIR-Pediatría. Hospital Miguel Servet. Zaragoza. España.
bEIR-Pediatría. Hospital Miguel Servet. Zaragoza. España.
cPediatra. CS Torrero La Paz. Sector II. Zaragoza. España.
dPediatra. CS Torrero La Paz. Zaragoza. España.
eEnfermera de Pediatría. CS Torrero La Paz. Sector II. Zaragoza. España.
Correspondence: M Tirado. E-mail: montsetiradomelero@gmail.com
Reference of this article: Tirado Melero M, Milagro Jiménez ME, Romero Salas Y, Galbe Sánchez-Ventura J, Balagué Clemós C, Zarazaga Gemes G, et al. Intelectual disability of genetic cause. Observational study in an urban primary health care center. Rev Pediatr Aten Primaria. 2015;17:309-15.
Published in Internet: 23-11-2015 - Visits: 27897
Abstract
Introduction: we review the number of neurodevelopmental disorders in the pediatric population of a primary care center in Zaragoza, in order to determine the prevalence and the growing importance of genetic diagnosis.
Material and methods: the research was carried out in the computerized medical record programme OMI6 with the following terms: “mental retardation”, “development delay”, “development disorders” and “autism spectrum disorders”.
Results: 76 cases of neurodevelopment disorders have been got, which mean 2.19% of the population of study. The main diagnoses were: 23 language disorders, 17 learning disorders, 11 mental retardation, 10 cases of autism, 8 development delay, 5 cases of dyslexia, 1 case of Asperger´s syndrome and 1 case of dyspraxia. A genetic study was requested in 21 cases, which supposed the 27.63% of children, being more frequent implementation in cases of mental retardation or autism. Genetic test provided diagnosis in 12 patients of the study, which means the 57.14% of the cases. A genetic cause was found in the 75% of the cases with an established diagnosis.
Conclusion: this study shows that neurodevelopmental disorders appear in our population with a similar frequency described in the literature. Genetic studies increasingly allow precise etiological diagnosis.
Keywords
● Autistic spectrum disorders ● Developmental disorders ● Genetic study ● Mental deficiencyINTRODUCCIÓN
Neurodevelopmental disorders are abnormalities in neuroanatomical structure or psychophysiological functioning that can be associated with impairments in intellectual, academic, behavioural, social and adaptive functioning. The term encompasses a broad range of diseases characterised by the impairment of one or more areas of neurologic functioning, causing a defective adaptation to the environment that is more or less severe depending on the disease. Two large groups can be differentiated: intellectual disabilities, and the group of pervasive developmental disorders, which includes autism spectrum disorders (ASDs), and specific developmental disorders of language, communication or learning, among others.
Intellectual disability is defined as significantly impaired intellectual functioning with onset during the developmental period that leads to deficits in adaptive functioning and limits the individual’s functioning in society. Historically, intellectual disability has been established as an intellectual quotient (IQ) of less than 70, while the mean IQ of the general population is 100 ±15 SDs. Applying this cut-off point, the prevalence of intellectual disability is 2% to 3%,1 with mild forms being much more prevalent. At present, intellectual disability is usually classified based on individual performance in the conceptual, social and practical domains2; that is, by the assessment of the child’s skills on different areas such as language, learning, reasoning, communication and social interaction, and performance of everyday activities.
The term psychomotor retardation or global developmental delay is reserved for children aged less than 5 years that do not achieve developmental milestones at the expected age. Its severity is a predictor of future cognitive or intellectual disability, so these children must be reassessed on a regular basis. Starting at 5 years, various tests can be administered to assess intelligence, and thus the term intellectual disability can be applied from this age on.
Pervasive developmental disorders first manifest in early childhood and may be defined as difficulties in adapting to the environment due to deficits in communication, social interaction, language or behaviour that are not due to an intellectual disability or other neurological, motor, or sensory abnormalities. The current incidence of these disorders ranges from between 20 to 30 cases per 10 000 inhabitants.3 The most important and prevalent disorders in this category are ASDs, which manifest with persistent deficits in communication and social interaction and restricted and repetitive behaviours and activities, resulting in a clinically significant impairment in social, academic and other areas of normal functioning. Language disorders are also frequent, and consist in persistent difficulties in any area of language acquisition and use due to impaired language comprehension or production and resulting in significant limitations in everyday functioning.
Patients with neurodevelopmental disorders must be assessed in order to make an aetiological diagnosis. Although it is not always possible, identifying the cause helps improve the management of these children at every level of care, as more information is available on the underlying mechanisms, prognosis, treatment, potential comorbidities, possible recurrences, etc. While most diagnostic tests are conducted in specialty clinics (usually Neuropaediatrics or Genetics) the primary care (PC) paediatrician must be aware of the available tests to understand the process the child is going to go through and counsel the family. An aetiological diagnosis can also address some of the questions raised in parents by diseases of these characteristics: Why did it happen? Could it have been prevented or identified earlier? Can it be treated? How is it going to unfold? Could this recur in future children? There are no easy answers to some of these questions, as knowing the underlying cause does not suffice to predict the outcome. Nevertheless, the goal is to make a specific diagnosis to understand the existing problem to the greatest possible extent. There is no consensus on the tests needed to make the diagnosis, as there is a broad range. In recent years, advances in molecular genetics have made it possible to identify several aetiologies that could not be diagnosed in the past, and further progress is expected in this field.
With the objective of determining the prevalence of these disorders, delving into their causes and in increasingly important molecular methods, we conducted a descriptive study in a PC centre of the city of Zaragoza (Spain) of the patients assigned to the caseloads of the three paediatricians in the centre. We performed an electronic search for neurodevelopmental disorder cases, collecting information on their causes and the diagnostic tests performed, to determine the frequency of aetiological and genetic diagnosis and the yield of molecular diagnostic techniques.
MATERIALS AND METHODS
We reviewed the neurodevelopmental disorder cases found in the population assigned to the three paediatricians of one PC centre in the city of Zaragoza (Spain), which amounted to 3472 children on August 1, 2014. We searched for these cases in the OMI6 database and electronic medical records of the autonomous community of Aragon using the following keywords: “intellectual disability”, “developmental delay”, “developmental disorder”, “autism”. Our search did not exclude patients referred to neuropaediatric or genetic clinics nor to early intervention programmes.
For each of the identified cases, we used the OMI6 or the electronic medical records to collect data on the sex and age of the child, whether genetic testing had or not been performed, the results of such testing if applicable, and performance of any other tests relevant to the aetiological diagnosis of a developmental disorder.
We accessed the information contained in the medical records of the patients adhering to all pertinent legal regulations and ethical principles.
RESULTS
We found 76 cases of neurodevelopmental disorders, which amounted to 2.19% of the population under study. This percentage is consistent with the published data for these disorders. Of all cases, 22 corresponded to girls and 54 to boys (28.95% and 71.05% of the total cases, respectively), which is also consistent with the higher prevalence reported in the male sex. The mean age was 8.3 years, with a minimum of 2 and a maximum of 17 years.
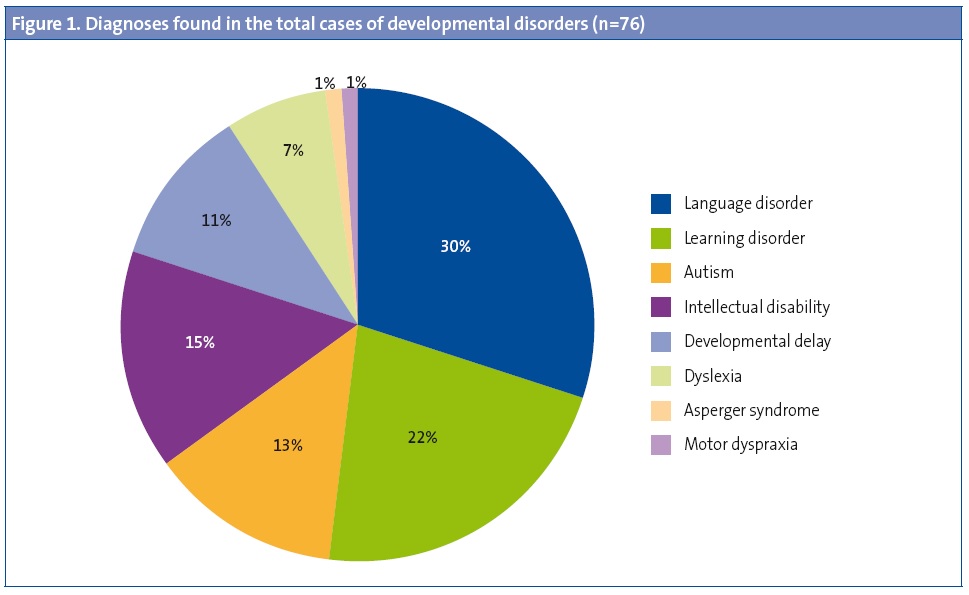
The main diagnoses observed were language disorders (23 cases), learning disorders (17 cases), intellectual disability (11 cases), ASDs (10 cases), developmental delay (8 cases), dyslexia (5 cases), Asperger syndrome (1 case) and motor dyspraxia (1 case) (Figure1).
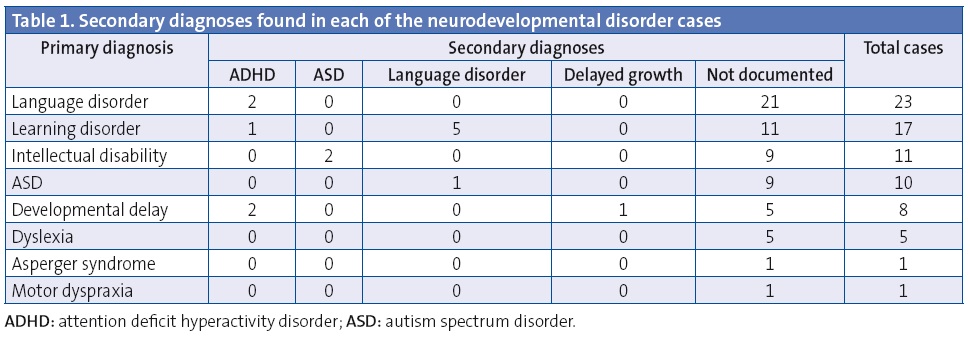
A secondary diagnosis was documented in 14 cases (18.42%): attention deficit hyperactivity disorder (ADHD), epilepsy, or delayed growth (Table 1).
Genetic testing was ordered in 21 cases (27.63% of the children) and was more frequent in cases of autism or intellectual disability than in cases of simple language or learning disorders: 90.9% of patients with intellectual disability and 70% of patients with autism, compared to only 5.45% of children with other disorders. The tests performed in every case were high-resolution karyotyping, genetic screening for fragile X syndrome and array-CGH, and screening for Dravet syndrome was also performed in the patient in which this syndrome was ultimately confirmed. The sole exception in which all of these tests were not performed corresponded to the four cases of Down syndrome, since due to the clear clinical suspicion the only required test was the high-resolution karyotype. Genetic testing led to aetiological diagnosis in 12 of the patients that underwent it, that is, 57.14% of tested patients. In our population, we found a genetic cause for 75% of cases with an established diagnosis.
DISCUSSION
We conducted a descriptive study in a PC centre in the city of Zaragoza that consisted in reviewing the data obtained from the OMI6 database and electronic medical records to determine the prevalence of developmental disorders and the proportion of cases with an aetiological diagnosis. There are some limitations to our study, chief of which is the potential to miss cases registered in the OMI6 under a code other than those included in the search. Data may also have been missed due to the difficulty involved in coding some specific diagnoses in this application.
We compared our results with those of the Neuropaediatrics Unit of the Hospital Universitario Miguel Servet in Zaragoza.4 We ought to note that cases of neurodevelopmental disorders found in our PC centre are referred to and evaluated in that unit. At this unit, an aetiological diagnosis is found for 31% of cases, compared to the percentage of 17.8% observed in our study. This can be accounted by the greater caseload of the hospital unit and to gaps in the information available through the OMI6 database. Of the cases in the hospital for which a diagnosis had been established, 46% were due to genetic causes. Our study found a genetic cause in 75% of the cases with an aetiological diagnosis. These percentages highlight the increasing importance of molecular methods in the diagnosis of neurologic diseases that could not be explained until a few years ago. Although the phenotype of some patients may suggest an underlying chromosomal abnormality associated with the developmental disorder, other patients will only have neurologic manifestations; nevertheless, genetic testing is key even in these cases, as microscopic abnormalities in chromosomes can produce an exclusively neurologic clinical picture. The PC paediatrician should be aware of this fact and be acquainted with the techniques used in genetics clinics to be able to inform families of the tests that the children may undergo. The methods applied most commonly are the following:
- Karyotyping. It is universally accepted that karyotyping should be performed routinely in all children with intellectual disability of unknown aetiology.1 High-resolution karyotyping is preferred (with at least 550 bands), as it can detect deletions or additions of as few as 5 Mb of DNA in addition to numerical chromosome abnormalities.5
- Fluorescence in situ hybridization (FISH). It consists in the binding of a known chromosomal or DNA fragment to a fluorescent probe to detect the presence or absence of that DNA fragment in the patient under study.5 This technique has the disadvantage that it requires suspicion of the abnormality that is to be screened for. This is the method used most commonly to diagnose microdeletion syndromes, such as DiGeorge, Prader-Willi or Williams syndrome.
- Analysis of subtelomeric abnormalities. These regions undergo a high rate of recombination that facilitates the development of deletions or duplications; they are also regions that contain a large number of genes, so that small changes in the genetic material can have severe consequences. These regions can be analysed by detection of chromosome ends with the FISH technique, with multiple ligation probe amplification (MLPA) to detect the number of copies of genes, or by analysis of DNA genetic polymorphism (SNP detection).
- Molecular studies: array-CGH (comparative genomic hybridization). It is the most powerful tool for the identification of submicroscopic chromosomal abnormalities. The devices have a solid surface on which thousands of DNA probes are arrayed, each of which can detect a certain DNA or RNA sequence or genetic polymorphism.6 Their main advantage is that they can detect thousands of genes simultaneously, which makes them a good tool for the investigation of neurodevelopmental disorders of unknown aetiology. Some authors suggest that this type of test should be performed as a first step in these patients rather than karyotyping, reserving the latter for cases in which classical chromosomal disorders are suspected or with a family history of chromosome rearrangements (as array-CGH does not detect balanced translocations or inversions).
The most prevalent developmental disorder in our study was language disorder. This is not an unexpected finding considering that up to 15% of preschoolers and 5% of school-aged children have speech or language disorders.7 The coding scheme used in the OMI6 software does not allow the differentiation between simple language delays, which are maturational in nature and have good outcomes, and specific language disorders, which are more severe and have a significant impact on learning, behaviour or social skills. In any case, the role of the PC paediatrician is to detect language problems early on and refer such cases for early intervention and speech therapy, also at an early stage, so that interventions can be as effective as possible. In severe cases or those with other associated symptoms, a referral to neuropaediatric services is also indicated. Most children with language disorders improve their communication skills, although some abnormalities may persist through adulthood, and these disorders have been associated with reading problems at later ages.
Overall, developmental disorders can be considered a problem found in PC paediatric clinics, and they may be severe. On many occasions, it is the child’s paediatrician that detects the warning signs during regular checkups. On others, it is the family that expresses suspicion, so it is important to pay attention to the questions and comments of parents. These disorders require early intervention with a multidisciplinary approach involving paediatricians, physical therapists, speech therapists, psychologists and social workers, among other specialists. In this sense, early intervention units are a key resource that integrate multiple types of care and provide substantial support to the families of children with these disorders. Therefore, early referral to these units is of the essence, as the outcome of these children will be partly determined by receiving stimulation and care appropriate to their condition. As patients undergo consultations and tests, the PC paediatrician can serve as a reference point for the family, providing information, identifying associated pathologies, referring to any necessary services, informing of available resources and patient associations, and above all helping the family to better understand the child in order to maximize quality of life.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABREVIATURAS: DNA: deoxyribonucleic acid • PC: Primary Care • RNA: ribonucleic acid • IQ: intellectual quotient • SD: standard deviation • FISH: fluorescence in situ hybridization • MLPA: multiple ligation probe amplification • ADHD: attention deficit hyperactivity disorder • ASD: autism spectrum disorder.
BIBLIOGRAFÍA
- Galán-Gómez E, Méndez-Pérez MP, Delgado-Rubio A. Estudios genéticos en el retraso mental inespecífico. An Pediatr Contin. 2012;10:7-15.
- Asociación Americana de Psiquiatría. Guía de Consulta de los criterios diagnósticos del DSM 5. Arlington, VA: Asociación Americana de Pediatría; 2013.
- García-Ron G. Indicadores clínicos precoces de los trastornos generalizados del desarrollo. An Pediatr (Barc). 2012;77:171-5.
- López-Pisón J. Nuestra experiencia en el diagnóstico etiológico del retraso global del desarrollo y discapacidad intelectual: 2006-2010. Neurología. 2013;29:402-7.
- Moeschler J. Genetic evaluation of intelectual disabilities. Semin Pediatr Neurol. 2008;15:2-9.
- Alonso J. Utilidad de los microarrays en Pediatría. An Pediatr Contin. 2008;6:218-22.
- Gassió-Subirachs R. Trastornos del lenguaje. An Pediatr Contin. 2006;4:140-4.
- Moeschler J, Shevell M. Clinical genetical evaluation of the child with mental retardation or development delays. Pediatrics. 2006;117:2304-13.
- López-Pisón J, Monge-Galindo L. Evaluación y manejo del niño con retraso psicomotor. Trastornos generalizados del desarrollo. Rev Pediatr Aten Primaria Supl. 2011;20:131-44.
- Gónzalez-Meneses A. Dismorfología clínica y genética I: enfoque diagnóstico del paciente dismórfico. An Pediatr Contin. 2008;6:140-6.
- Martínez Fernández ML, Bermejo E, Martínez Frías ML. Ejemplos clínicos de alteraciones crípticas del ADN y guías para sospechar que un niño pueda tener alguna alteración críptica o molecular. SEMERGEN. 2010;36:573-8.
- González-Alvaredo S, Sanz Rojo R, García Santiago J, Gaztañaga Expósito R, Bengoa A, Pérez-Yarza EG. Criterios de diagnóstico genético en casos de retraso mental y del desarrollo de origen idiopático. An Pediatr (Barc). 2008;69:446-53.





