Vol. 17 - Num. 67
Original Papers
Nocturnal enuresis. Epidemiological study in school population
Carmelo Gutiérrez Abada, M. N. San José Callejaa, M Castroviejo Espinosab, R Sánchez Gutiérrezc, E Ardela Díezd, J. A. Cordero Guevarae
aPediatra. CS Las Huelgas. Burgos. España.
bEnfermera. CS Las Huelgas. Burgos. España.
cEnfermera. HospitalHospital Universitario de Burgos. Burgos. España.
dCirujano Pediátrico. Hospital Universitario de Burgos. Burgos. España.
eTécnico de Salud. Gerencia de Atención Primaria de Burgos. Burgos. España.
Correspondence: C Gutiérrez. E-mail: cgapalencia@yahoo.es
Reference of this article: Gutiérrez Abad C, San José Calleja MN, Castroviejo Espinosa M, Sánchez Gutiérrez R, Ardela Díez E, Cordero Guevara JA. Nocturnal enuresis. Epidemiological study in school population. Rev Pediatr Aten Primaria. 2015;17:227-34.
Published in Internet: 03-09-2015 - Visits: 19831
Abstract
Introduction: nocturnal enuresis (NE) is a common childhood health condition. This problem causes personal and social repercussion. The health professionals have to make an individualized and adequate management of this problem. The aim of this study is to know the prevalence of NE in children between seven and ten years old of the city of Burgos.
Patients and methods: to this end, we have designed an observational and transversal study. We have selected a random sample of school children in Burgos between 2nd and 5th year of Obligatory Primary Education. They have completed a questionnaire.
Results: the prevalence of NE was 7.3%. NE is more frequent in males and children with familiar precedents of NE, with some type of chronic illness, with associated disorders of the sleep and behavior and with low academic performance.
Conclusions: the prevalence of NE in children in Burgos city is lower than in another child groups of similar characteristics. There is a low diagnosis rate of NE in Burgos city.
Keywords
● Children ● Epidemiology ● Nocturnal enuresis ● Risk factorINTRODUCTION
Nocturnal enuresis (NE) is a clinical entity defined by the last review of the International Children's Continence Society (ICCS) as urinary incontinence while asleep in a child aged at least 5 years.1 It is classified into different diseases depending on the onset of enuresis (primary or secondary) and on its association or lack thereof with some type of causative organic pathology (non-monosymptomatic or monosymptomatic, respectively). The age at which it can first be diagnosed remains subject to debate, although 5 years is generally considered the age at which the term NE first starts to apply.1-4
Nocturnal enuresis is a frequent complaint in primary care (PC) paediatric practice, with an estimated prevalence that ranges from 8% to 15%.4-6 The trigger or cause of NE remains unknown, and it is generally considered to be multifactorial (family aggregation, bladder dysfunction, neurohormonal abnormalities, psychological factors, socioeconomic factors, sleep pattern disturbances, etc). Thus, when we care for a patient with NE in our paediatric practise, we are facing a complex health issue the management of which must be determined on a case-to-case basis.4,5,7 Aside from potential physical features (abnormalities in the genitourinary tract, spine, etc), we must consider the psychological effects that can result from NE, which may be difficult to assess and manage.4
We designed an epidemiological study to gain a deeper understanding of the characteristics of the population of children with enuresis in the city of Burgos (Spain), and to identify the main risk factors associated with this condition.
PATIENTS AND METHODS
The reference population consisted of children aged 7 to 10 years enrolled in public, private, or subsidised private schools in the city of Burgos during the 2013–2014 academic year. Based on 2012 data from the National Institute of Statistics (Instituto Nacional de Estadística [INE]), we estimated the size of this population to be 5500 children. We calculated the sample size for an estimated prevalence of 15%, a precision of 2%, a 95% confidence interval, a 30% attrition rate and the effects of stratified randomization. The resulting sample size was 1485 children.
The Education Department of the Province of Burgos (Dirección Provincial de Educación de Burgos) provided us with a list of the schools in the city of Burgos offering compulsory primary education (Educación Primaria Obligatoria [EPO]). Of the total of 41 institutions, and after obtaining the approval of the principal of each school, we included 31 schools in the sample. Each of these schools provided information on the number of classes and number of students in each class for the second and fifth year of the EPO. We used this information to stratify by class interval, after which we performed a random selection of classrooms.
The questionnaires were given to children and their families in the schools, and were completed after the legal guardians of participants provided the informed consent. The questionnaires were anonymous and consisted of 43 items organised into four sections: personal data of the participant and family members, incontinence-related health data for the child, and incontinence-related data for the family.
After collecting the questionnaires, we discarded all that were not completed or completed incorrectly, and all that did not meet the inclusion criteria (children older than 10 years). The remaining data were entered in an electronic database and processed using the SPSS® v 17.0 application. We used the chi squared test for qualitative variables and the Student’s t test for the quantitative variables. We calculated the odds ratio for qualitative variables that had reached statistical significance, and the Pearson correlation coefficient for quantitative variables. We defined statistical significance as P < .05.
RESULTS
We collected a total number of 1468 questionnaires. The response rate was 80.1%. We discarded 95 of the questionnaires because they were not completed, were completed incorrectly, or were completed by participants older than 10 years. The final data included 1081 valid questionnaires, which amounted to 73.6% of all the collected questionnaires and 19.6% of the total population of children aged 7 to 10 years in the city of Burgos.
The sample had a symmetrical distribution in terms of sex (49.2% male and 50.8% female), with a mean age of 9.07 years. The mean number of siblings was 1.56 (18.2% did not have siblings). Most participants were Spanish nationals (94.7%), 1.1% Chinese, 1.1% Romanian and the rest (3.1%) of other nationalities. Of all parents, 90.8% were married or in a domestic partnership, 6.8% separated or divorced, and 2.4% were single parents. As for the children’s medical histories, we found a previous history of at least one urinary tract infection in 11.2% of the children, underlying renal or urinary tract disease in 1.7%, a history of preterm birth (gestational age ≤ 36 weeks) in 6.3%, some type of sleep disorder in 22.3% (frequent nightmares, night terrors, sleep apnoea, significant difficulty falling asleep), a behavioural diagnosis in 3.7% (84% of which corresponded to attention deficit hyperactivity disorder [ADHD]), while school performance was rated as poor by parents in 6.5% of children.
Ninety-nine children (9.2%) had some type of urinary incontinence, of whom 42.4% had daily episodes of wetting, 6.1% at least one a week, 24.2% two or three a month, and 27.3% one or less a month. The prevalence of NE in our sample was 7.3%: 2% corresponded to primary monosymptomatic nocturnal enuresis (PMNE), 4.1% to primary non-monosymptomatic nocturnal enuresis (PnMNE) and 1.2% to secondary nocturnal enuresis (SNE). The rest of children with urinary incontinence were distributed between diurnal urinary incontinence (0. 9%) and diurnal and nocturnal urinary incontinence (1.1%).
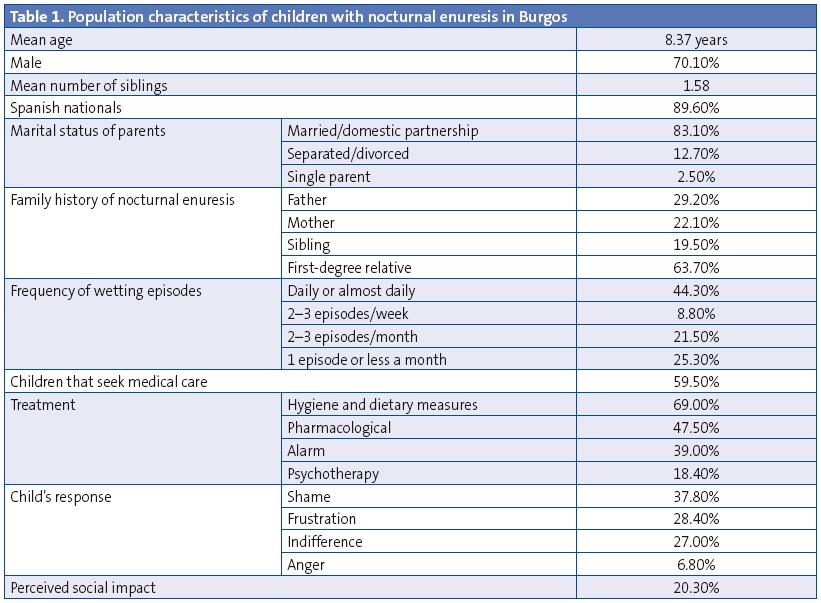
Table 1 shows the characteristics of the population of children with NE. The most salient findings in comparison to the rest of the sample were higher proportions of males, of children of separated or divorced parents, and of family history of NE. On the other hand, we found no significant differences in the mean age of children with NE compared to the rest of the sample, nor in the mean number of siblings or in nationality. Furthermore, it is worth noting that only 59.5% of children that experienced wetting had ever seen a paediatrician or paediatric nurse for that complaint. Of the children that had, 69% had received some type of treatment, with hygiene and dietary measures and desmopressin being most common. Last of all, we found it interesting that only 20.3% of children with NE reported feeling that incontinence had some form of negative impact on their personal lives (insecurity, low self-esteem, limitation of social activities etc).
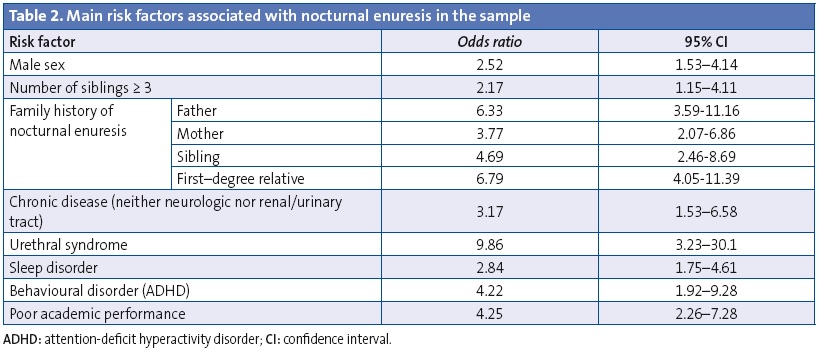
Our assessment of possible risk factors associated with NE found a statistically significant correlation with several of them. The strongest correlation corresponded to family history of NE, the presence of urethral syndrome and the presence of behavioural disorders (almost always ADHD) and poor academic performance (Table 2). We did not find an association with other factors such as constipation, obesity, preterm birth or a personal history of urinary tract infection or kidney disease (probably due to the low number of children with these conditions). We did find a statistically significant association with age, with a negative Pearson’s correlation coefficient (r, -2.53; P < .01).
As for the attitudes of parents in regard to incontinence, we assessed their reaction to wetting episodes (indifference, frustration, embarrassment, anger, or positive reinforcement). None of these attitudes predominated in either fathers or mothers, and they were irregularly distributed across the subset of children with urinary incontinence. We also found no differences in educational attainment between the parents of children with NE and the parents of the other children.
DISCUSSION
A first challenge in discussing nocturnal enuresis is its definition. Different criteria apply depending on the definition used among those proposed by the various competent institutions and societies (International Children’s Continence Society [ICCS], Diagnostic and Statistical Manual of Mental Disorders [DSM-5], International Classification of Diseases [ICD-10], etc).1-4,8 This disparity in diagnostic criteria makes it difficult to compare different studies and draw fully valid conclusions.
For the purposes of this study, we used the latest definition provided by one of these institutions, the ICCS, in 2014.1 The prevalence we found for the city of Burgos was lower than the prevalence found in populations of similar characteristics.9-19 There is an even greater difference in relation to the prevalence found in populations in rural areas or developing countries. This peculiarity highlights the fact that the prevalence of NE depends to a great extent on cultural and social factors. Such sociocultural factors play a role in starting toilet training at later ages or perceiving NE as a purely maturational or developmental process that carries no psychosocial consequences.15,20
The comparative analysis of the population characteristics of children with NE showed that there was a predominance of males (70.1%), a circumstance that has been observed frequently in other studies, especially at early ages, as the sex distribution tends to even out in older children. This seems to be related to a slower psychomotor development and skill acquisition in boys than in girls.9,11,12,16,18-20 Another factor that has been associated with NE is a greater number of siblings.12,16,17 The evidence suggests a correlation between the number of siblings and NE, consistent with our findings. Another aetiologic factor under study is the family history of NE. Our study found a high percentage of family history of NE (2/3 of children with NE had a first-degree family member with a positive history of NE, most commonly the father). This was consistent with the findings in the medical literature, although there is a wide variation in the reported percentages, with the percentage we found being among the highest.9,11-13,16,17,21 This is evidence of familial aggregation in NE, although the reason for this pattern is not clear. Some authors have proposed genetic factors as the cause for the association, but cultural factors have been proposed as well. Such cultural factors influence the way in which each family responds to NE from their own perspective and the particular relevance it attributes to NE. Thus, there is evidence that the choice to delay toilet training may influence delays in developing bladder control and lead to NE.9,21,22.
We would like to highlight the association between NE and the presence of urethral syndrome (frequent urination, vesical tenesmus, urinary urgency, urinary retention). The latter is the risk factor with the strongest association of all those we studied, which was also stronger than the association reported in other studies.10 This brings up the question of whether urethral and bladder problems may also be causes of enuresis. Children with urethral syndrome and enuresis would be categorised into the primary non-monosymptomatic enuresis and secondary enuresis groups.
Our study also found a higher prevalence of sleep and behavioural disorders in enuretic children. We considered a sleep disorder any disturbance related to sleep and affecting its quality or quantity. Thus, sleep disorders included nightmares, night terrors, heavy snoring, apnoea or significant difficulty falling asleep. In our sample, 44% of children with NE had associated sleep disorders. This percentage was higher than in the rest of the sample (22.3%) and in other studies.13,22-24
As for behavioural disorders, the diagnosis received by all enuretic children with such a disorder was ADHD. Specifically, 14 children had received an ADHD diagnosis, amounting to 18% of enuretic children, a percentage that was considerably higher than the percentage for the overall sample (3.7%). We found this striking. This finding suggests an association between NE and ADHD, consistent with the findings of other studies.13 It is unclear which of the two, NE or ADHD, is the primary disorder, but it seems reasonable to ask children that seek care for NE about the presence of symptoms of ADHD, and the other way around. We also found an association between NE and poor academic performance in our series. Academic performance was reported subjectively by the parents in response to a direct question, and we did not establish objective criteria for poor academic performance. As was the case with ADHD, we found that there was a higher proportion of enuretic children compared to non-enuretic children that performed poorly in school (21% versus 6.5%). Also, as with ADHD, it is difficult to tell which is the cause and which the effect.17,22 The two conditions are probably interrelated, with NE being the cause in some instances (by generating low self-esteem or insecurity resulting in achievement below expectations) and poor school performance in other instances being secondary to a learning disorder or psychomotor delay that is also the cause of NE.
We analysed other risk factors for which we found no statistically significant association, such as constipation, obesity, preterm birth and a previous history of urinary tract infection.
Our analysis of the response of parents of enuretic children showed that only 59% of children with NE had visited the paediatrician or nurse for this complaint. It seems that there are still circumstances that prevent enuretic children from accessing care. We believe that this is due to parents lacking information on NE and feeling somewhat reluctant or unable to bring themselves to discuss the wetting episodes with the paediatrician. Other studies have also identified this phenomenon which, combined with parental low educational attainment in some instances (which was not the case in our study) leads to underdiagnosis of NE .15,17,18,20,25 On the other hand, not all children that seek care are assessed or treated appropriately by health care professionals. Only 71% of these children undergo some type of medical testing, which sets some limitations for the appropriate management of the child and thus reduces the efficacy of the prescribed treatment.4,5 Furthermore, only 73% of enuretic children that seek paediatric care receive some type of treatment. Both of these circumstances suggest that enuretic children are not always assessed and treated appropriately.11
Another aim of this study was to assess the extent of the impact that NE had in the children of Burgos and their parents. We were surprised to find that only 20.1% of children with NE reported that this problem caused them distress or affected their social life, when only 27% expressed feeling indifferent about being incontinent. The rest of the children (73%) stated that wetting elicited some type of negative feelings in them (anger, frustration or shame). We found the assessment of this aspect to be challenging, and we could not reach a clear conclusion. This may be due to the later start of collective activities (camps, fieldtrips, etc), so that NE has not yet become socially relevant. The findings of other studies on this aspect vary widely, but they generally showed a greater impact on children than the one found in our study.11
CONCLUSIONS
In recent years, the understanding of nocturnal enuresis has grown among paediatricians and paediatric nurses. Parents are also more aware of this problem. But we are still far from considering NE a condition that is generally diagnosed early and managed appropriately, as demonstrated by the results of our study.
The prevalence of NE in the city of Burgos was lower than the prevalence reported in the literature. This may be due to a greater knowledge and monitoring of the condition in our paediatric clinics. But there is still plenty of room for improvement, as evinced by the large percentage of incontinence cases for which no medical attention was sought. The population characteristics and risk factors of patients with NE resemble those found in similar populations. The only salient difference was the higher prevalence of concomitant urethral syndrome in our study, of which the importance and impact on the patient is hard to assess. It is important that NE is well understood by health professionals that provide care for children (paediatricians, paediatric nurses and others) and also by parents and educators. For this to happen, we need to make an effort as healthcare professionals to convey adequately the importance of NE to children, parents and teachers. Furthermore, we need to break the silence and the taboo surrounding NE that persists in our society. All efforts must strive to increase the wellbeing of children suffering from NE so that it can improve or resolve early.
We should bear in mind at all times the potential personal and/or social repercussions that NE may have on the affected child. It is essential that the child feels safe and free from stigmas that may affect his or her self-esteem. In doing so, the child will not only enjoy a more comfortable childhood, but will also achieve bladder control earlier.
FUNDING
The study was funded with the grant GRS 738/B/13 as part of the funding for research projects in biomedicine given by the Gerencia Regional de Salud (Regional Department of Health) of Castilla y León in 2013.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREBIATIONS: PC: Primary Care • NE: nocturnal enuresis • PMNE: primary monosymptomatic nocturnal enuresis • PnMNE: primary non-monosymptomatic nocturnal enuresis •SNE: secondary nocturnal enuresis • EPO: compulsory primary education • ICCS: International Children's Continence Society • INE: Instituto Nacional de Estadística (National Institute of Statistics) • ADHD: attention-deficit hyperactivity disorder.
ACKNOWLEDGMENTS
We want to thank the Dirección Provincial de Educación of the province of Burgos, and the participating schools of the city of Burgos for their excellent disposition and collaboration.
REFERENCES
- Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: update report from the Standardization Committee of the International Children's Continence Society. J Urol. 2014;191:1863-1865.e13.
- American Psychiatric Association. Enuresis. Diagnostic and statistical manual of mental disorders. 5.ª edición. Washington, DC: Author; 2013.
- International Statistical Classification of Diseases and related health problems. 10th revision. En: Organización Mundial de la Salud [online] [consulted on 24/08/2015]. Available in www.who.int/classifications/icd/en/
- Van de Walle J, Rittig S, Bauer S, Eggert P, Marschall-Kehler D, Tekgul S. Practical consensus guidelines for the management of enuresis. Eur J Pediatr. 2012;171:971-83.
- Nevéus T. Nocturnal enuresis-theoretic background and practical guidelines. Pediatr Nephrol. 2011;26:1207-14.
- Ramírez-Backhaus M, Arlandis Guzmán S, García-Fadrique G, Martínez Agulló M, Martínez García R, Jiménez-Cruz JF. La enuresis nocturna. Un trastorno frecuente con una prevalencia difícil de estimar. Actas Urol Esp. 2010;34:460-6.
- Lottmann HB, Alova I. Primary monosymptomatic nocturnal enuresis in children and adolescents. Int J Clin Pract Suppl. 2007;(155):8-16.
- Schultz-Lampel D, Steuber C, Hoyer PF, Bachmann CJ, Marschall-Kehler D, Bachmann H. Urinary incontinence in children. Dtsch Arztebl Int. 2011;108:613-20.
- Lapeña López de Armentia S, Rodríguez Fernández LM, Marugán de Miguelsanz JM, Palau Benavides MT, Reguero Celada S, Gutiérrez Fernández M, et al. Enuresis nocturna primaria y secundaria. ¿Son entidades diferentes? An Esp Pediatr. 1996;44:345-50.
- Butler RJ, Golding J, Northstone K, ALSPAC Study Team. Nocturnal enuresis at 7.5 years old: prevalence and analysis of clinical signs. BJU Int. 2005;96:404-10.
- Ramírez Backhaus M, Martínez Agulló E, Arlandis Guzmán S, Gómez Pérez L, Delgado Oliva F, Martínez García R, et al. Prevalencia de la enuresis nocturna en la Comunidad Valenciana. Sección infantil del Estudio Nacional de Incontinencia. Estudio EPICC. Actas Urol Esp. 2009;33:1011-8.
- Semolic N, Ravnikar A, Meglic A, Japelj-Pavesić B, Kenda RB. The occurrence of primary nocturnal enuresis and associated factors in 5-yer-old outpatients in Slovenia. Acta Pediatr. 2009;98:1994-8.
- Sanjuan S, Pérez A, González R, Vargas I, Davara L, Luque M, et al. Enuresis primaria monosintomática. Estudio de 100 casos. Rev Pediatr Aten Primaria. 2000;2:29-45.
- Karničnik K, Koren A, Kos N, Marčun Varda N. Prevalence and quality of life of slovenian children with primary nocturnal enuresis. Int J Nephrol. 2012;2012:509012.
- Hashem M, Morteza A, Mohammad K, Ahmad-Ali N. Prevalence of nocturnal enuresis in school aged children: the role of personal and parents related socioeconomic and educational factors. Iran J Pediatr. 2013;23:59-64.
- Kanaheswari Y. Epidemiology of childhood nocturnal enuresis in Malaysia. J Paediatr Child Health. 2003;39:118-23.
- Carman KB, Ceran O, Kaya C, Nuhoglu C, Karaman MI. Nocturnal enuresis in Turkey: prevalence and accompanying factors in different socioeconomic environments.Urol Int. 2008;80:362-6.
- Lee SD, Sohn DW, Lee JZ, Park NC, Chung MK. An epidemiological study of enuresis in Korean children. BJU Int. 2000;85:869-73.
- Butler RJ, Heron J. The prevalence of infrequent bedwetting and nocturnal enuresis in childhood. A large British cohort. Scand J Urol Nephrol. 2008;42:257-64.
- Wang QW, Wen JG, Song DK, Su J, Zhu QH, Liu K, et al. Bed-wetting in Chinese children: epidemiology and predictive factors. Neurourol Urodyn. 2007;26:512-7.
- Marugán de Miguelsanz JM, Lapeña López de Armentia S, Rodríguez Fernández LM, Palau Benavides MT, Torres Hinojal MC, Menau Martín G, et al. Análisis epidemiológico de la secuencia de control vesical y prevalencia de enuresis nocturna en niños de la provincia de León. An Esp Pediatr. 1996;44:561-7.
- Rodríguez Fernández LM, Marugán de Miguelsanz JM, Lapeña López de Armentia S, Palau Benavides MT, Alvaro Iglesias E, Naveira Gómez C, et al. Estudio epidemiológico sobre enuresis nocturna en escolares: Análisis de factores asociados. An Esp Pediatr. 1997;46:252-8.
- Cohen-Zrubavel V, Kushnir B, Kushnir J, Sadeh A. Sleep and sleepiness in children with nocturnal enuresis. Sleep. 2011;34:191-4.
- Waleed Fe, Samia AF, Samar MF. Impact of sleep-disordered breathing and its treatment on children with primary nocturnal enuresis. Swiss Med Wkly. 2011;141:w13126.
- Martínez García R. Tiempo de reflexión sobre la enuresis. Actas Urol Esp. 2009;33:935-8.





