Vol. 17 - Num. 67
Original Papers
Collection of urine in febrile infants for diagnosis of urinary tract infection in the Emergencies’ room
María Pilar Roncalés Samanesa, Pilar Caudevilla Lafuentea, Elena Sancho Graciaa, Virginia Gómez Barrenab, Raquel Pérez Delgadoc, Carmen Campos Callejab
aServicio de Pediatría. Hospital Universitario Miguel Servet. Zaragoza. España.
bUnidad de Urgencias de Pediatría. Hospital Universitario Miguel Servet. Zaragoza. España.
cServicio de Pediatría. Hospital Infantil Miguel Servet. Zaragoza. España.
Correspondence: MP Roncalés. E-mail: pilar.roncales@gmail.com
Reference of this article: Roncalés Samanes MP, Caudevilla Lafuente P, Sancho Gracia E, Gómez Barrena V, Pérez Delgado R, Campos Calleja C. Collection of urine in febrile infants for diagnosis of urinary tract infection in the Emergencies’ room. Rev Pediatr Aten Primaria. 2015;17:205-11.
Published in Internet: 03-09-2015 - Visits: 29754
Abstract
Introduction: urinary tract infection (UTI) in children is a common process. It is essential to find an adequate method to collect urine, to avoid false positives, minimizing invasive procedures. Clean catch urine (CCU) is a noninvasive technique, with low contamination rate, so it has been established as the recommended method for urine collection to update our clinical protocol.
Material and methods: a prospective longitudinal descriptive and analytical study was conducted in a tertiary hospital in the Emergencies’ room (ER) in two periods, before and after the update protocol. Age, sex, time in the ER, collection method, sediment and urine culture and diagnosis in febrile patients <3 years were analyzed.
Results: there were 140 patients in 2012 and 180 in 2011, with no differences in age and sex distribution. The mean ages were 12 and 14 months respectively. 35.7% of the samples were collected by CCU in 2012, compared to 7.8% in 2011 (p<0.001). In 2011 more confirmations of urine analysis were necessary: 20.5% vs. 10.7% in 2012. There were no significant differences between the number of suspected UTI or the contaminated samples in both years. Neither did between samples collected by catheterization or CCU in 2012. The average length of stay in the ER in 2011 was 221 minutes, while 190 in 2012 (p<0.05).
Conclusions: urine collection by CCU is a simple and noninvasive method, which usually does not require confirmation, thereby reducing the wait time in the ER. There has not been an objectified increased of false diagnosis of UTI in patients with sample collected by CCU.
Keywords
● Emergency room ● Infants ● Urine collectionINTRODUCTION
Urine is usually sterile. Urinary tract infection (UTI) is a frequent ailment in the paediatric age group defined by the presence of bacteria in the urinary tract accompanied by compatible symptoms.1
We speak of a UTI when there are clinical signs and symptoms associated to a bacterial count in urine that is clinically relevant based on the urine collection method employed to obtain the specimen for culture. The clinical features of this disease vary widely, and depend to a great extent on the age at presentation and the localization of the UTI.1
To avoid false-positive results, it is key that urine specimens are collected correctly using the most sterile technique possible and avoiding invasive procedures.
The best technique for obtaining uncontaminated urine samples is direct bladder aspiration by suprapubic puncture, as this avoids the passage of urine through the urethra. It is a simple procedure, but it is invasive and has a variable success rate (23%–90%). It is followed by urinary catheterization, which has a sensitivity of up to 95% and a specificity of 99%. However, the psychological impact in patients older than one year and even the occasional need for sedation must be taken into consideration. There are other methods, such as the urine collection bag and midstream urine collection (clean-catch).2
According to the most recent clinical practice guidelines,1 bag collection is associated with a higher rate of contamination compared to other methods such as catheterization or suprapubic aspiration. However, we must find the method that is the least invasive while simultaneously having the lowest risk of contamination.
Midstream urine collection has been accepted as an appropriate method to obtain urine specimens in continent children. Collection of spontaneous urine is the equivalent method in infants lacking bladder control.
The protocol in our emergency department was updated in 2011, and among other measures, collection of spontaneous urine was introduced as the preferred technique for children lacking bladder control.
MATERIALS AND METHODS
We conducted a prospective longitudinal descriptive and analytical study in a tertiary hospital (Hospital Universitario Infantil Miguel Servet, Zaragoza, Spain), between October 12 and December 20 of 2012. The population under study consisted of febrile patients aged less than 3 years that received emergency care at our hospital and underwent urine testing. We then compared the results obtained with the results of the same period in the preceding year.
As specified in our hospital’s protocol, urinalysis was performed in all patients aged less than 3 months with a fever of unknown source of more than 38 °C, and all patients aged 3 to 36 months with a fever of unknown source of more than 38.5 °C, or with a temperature of more than 38 °C and clinical manifestations compatible with a UT I. We excluded patients with compatible symptoms that had no fever.
We considered the results of basic urinalysis abnormal when the specimen was positive for nitrites or leukocyturia, the latter of which was defined as follows depending on the collection method: for samples collected in a bag, as more than 20 white blood cells per high power field (WBC/HPF) in males and more than 50 in females, with the results being inconclusive between 10 and 20 and between 30 and 50 WBC/HPF respectively; for spontaneous urine samples, as 10 WBC/HPF for both sexes; and for samples collected by catheterization, as more than 3 to 5 WBC/HPF.
We collected the following data for all patients: epidemiological data (age, sex, renal and urological history), length of stay in emergency department, time of urine collection, method of collection, results of basic urinalysis and urine culture, final diagnosis, requiring/not requiring hospital admission, and treatment after discharge.
RESULTS
A total of 140 samples were collected in 2012 (1.5% of the total number of cases seen at the emergency department of the hospital), and 180 in 2011 (1.3% of the patients seen in the same department during the corresponding period).
In 2012, 55% of the samples corresponded to males and 45% to females, and in the previous year the proportions were reversed. The mean age was 12 months in 2012 (range, 36 days—35.6 months; median, 13 months) and in 2011 the mean age was 14 months (range, 9 days—35.5 months; median, 11 months). We did not find significant differences by sex and age group between the 2011 and the 2012 samples.
We did find statistically significant differences between both periods in the number of spontaneous or on-command midstream urine samples and the number of samples collected in a bag: 35.7% in 2012 were spontaneous urine or midstream urine samples, compared to 7.8% in 2011 (P < .001). Furthermore, in 2011 a higher number of confirmatory tests were needed, a difference that reached statistical significance (20.5% in 2011 and 10.7% in 2012), and the most frequent method used for confirmation was catheterization (19.4% versus 7.1%, respectively; P < .001).
In 2011 there were 48 cases of suspected UTI (26.6%), 119 cases of fever without a source (66.1%) and 13 patients received other diagnoses (7.2%). In 2012, 36 patients were discharged from the emergency department with a diagnosis of suspected UTI (25.7%, a percentage similar to that of the previous year), 80 cases with fever without a source (57.14%) and 24 with other diagnoses (17.14%). We did not find statistically significant differences in the number of suspected cases of UTI between the two years.
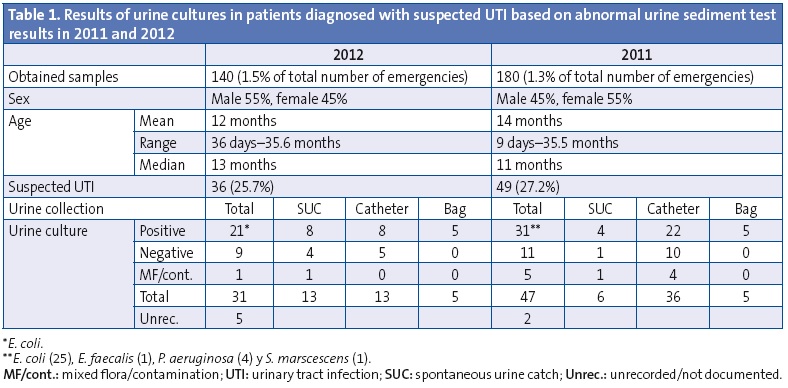
Table 1 summarises the urine culture results for both years. We did not find statistically significant differences in the number of contaminated samples between the two groups. For 2012, the year in which more samples were obtained by the spontaneous urine catch method, we compared the results of urine cultures from spontaneous urine catch samples and catheterization samples. Of the total number of suspected UTIs in the spontaneous urine group, 30.1% corresponded to negative cultures and 7.6% to a mixed flora, while in the catheterization group 38.4% corresponded to negative cultures, with no statistically significant differences found between both groups.
When it came to the previous renal and urological history, in 2011 six patients had a previous history of UTI (3.3%) and ten had received a diagnosis of pyelectasis (5.5%). We ought to note that not all cases with a positive history had abnormal urine sediment test results (75% abnormal, 25% normal). In 2012, of the seven patients with a previous history of at least one UTI (3.6%), three had received a diagnosis of pyelectasis (2.1%) and five were being followed up for vesicoureteral reflux (5.6%). During this period, too, not all patients with a personal history of UTI received a new UTI diagnosis, with abnormal results found in the urine sediment tests in 40%.
In terms of the time spent in the emergency department, the mean length in 2011 was 221 minutes, while in 2012 it was 190 (the difference was statistically significant, P < .05). As for the mean wait time by collection method, in 2012 it was 73 minutes for patients in which the sample was collected in a bag compared to 41 minutes in those with spontaneous urine catch samples. In patients in whom the sample was collected by the midstream or spontaneous urine catch methods in 2011, the mean wait time was 63 minutes, markedly shorter than the time spent by patients in whom it was collected in a bag (97 minutes).
In 2012, there was a significant decline in the number of patients with UTI admitted to the hospital (P < .05), 50% of patients compared to 79.2% in 2011, which was associated to changes to the admission criteria and treatment protocol for patients with a diagnosis of febrile UTI that had been approved in our hospital.
DISCUSSION
Urinary tract infections are a frequent cause of fever in childhood, accounting for 5% to 8% of cases of fever without a source in infants.3,4 In our series, the percentage of suspected UTI among the latter approximated 25%, with urine culture results being positive in 58.3% in 2012 (14.9% of the total of patients in our sample had confirmed diagnoses) and 64.6% in 2011 (17.2%).
A delay in the diagnosis of acute pyelonephritis can lead to lesions in the renal parenchyma, while misdiagnosis can lead to diagnostic and treatment approaches that are useless, dangerous and costly for both the patient and the community.5
Urine culture is the gold standard for the diagnosis of UTI, but obtaining an uncontaminated sample is difficult in younger children. The urine collection methods that are commonly used are the urine collection bag, urinary catheterization, suprapubic aspiration and spontaneous urine collection. Urinary catheterization and suprapubic aspiration are recommended as the best techniques to minimise false-positive results, but they are painful and more invasive. They are more aggressive and carry risks, as they may lead to pain after the procedure, urinary tract lesions and potential infections secondary to the procedure. Bag collection is noninvasive and an easy-to-use alternative, but is associated to a high rate of contamination.6,7 Hernangómez et al carried out a study on 124 patients with fever or suspected UTI in which they analysed the complications in patients subjected to single urinary catheterization. They communicated with 116 of the patients, finding that three of them had pain in the genital region, one case of unconfirmed haematuria and one case of UTI diagnosed 12 days after urinary catheterization, leading to the conclusion that this method is effective and safe, but nevertheless an invasive technique that requires quality control.8
In 2012, Karacan et al conducted a study on 1067 patients in which they compared bag collection, urinary catheterization, suprapubic aspiration and spontaneous urine collection. Noteworthy among their results was a contamination rate of 14.3% for spontaneous urine samples, similar to the rate found in samples obtained by catheterization. The contamination rate was 43.9% for samples collected in a bag, and 9.1% for samples collected by suprapubic aspiration. The authors of this study noted that the spontaneous urine catch was their preferred method of collection, but also underscored the difficulty in obtaining such samples.9 In our experience, we have found that if the family and the unit staff cooperate and collection is performed in an appropriate location, the spontaneous urine catch is a relatively simple technique. It is also the least aggressive towards the patient.
Most studies comparing urine collection methods do not include midstream urine collection in children without bladder control. A study performed at the Institute of Maternal and Child Health of Pernambuco (IMIP, Recife, Brazil) compared urine samples collected in children younger than 3 years with no previous history of UTI. In this study, contamination was found in 14.7% of the spontaneous urine catch samples, a significantly lower rate than the one corresponding to samples obtained with a bag (26.6%).10 Another study that compared different urine sample collection methods in children younger than 2 years found a contamination rate of 26% in spontaneous urine catch samples, which was significantly higher than that in samples collected by catheterization (12%) or suprapubic aspiration (1%). They attributed the high rate of contamination of spontaneous urine catch samples to the lack of standards for sample collection, and recommended additional studies given the wide variability in the rates of contamination reported in the literature.11 In our experience, the rates of contamination in samples obtained by spontaneous urine collection and urinary catheterization were similar, based on which we consider the spontaneous urine catch a valid technique for obtaining urine samples. However, our study found contamination rates higher than those described in the references of up to 42.8%. Therefore, improvement of this parameter should be an objective to consider, so that sterility can be optimised for both methods. We believe that the reason for this is that families are given insufficient information when this technique is explained to them, and this could improve by proper training of the health care staff.
According to the 2014 protocols of the Asociación Española de Pediatría (Spanish Association of Pediatrics), the collection method used in children lacking bladder control must be all the more reliable (with a lower risk of contamination) the more urgent it is to establish the diagnosis and to initiate treatment, and spontaneous urine catch is accepted as a reliable collection method, the yield of which can be increased by the previous use of abdominal and lumbosacral stimulation manouvres.12
According to our study, spontaneous urine collection is a method that reduces wait times compared to the bag collection method, although the fastest and most reliable method is urinary catheterization. However, spontaneous urine collection is a noninvasive method compared to catheterization, and in our experience parents prefer to attempt a spontaneous urine catch to postpone and, if possible, avoid urinary catheterization
The recommendations of the Conferencia de Consenso “Manejo Diagnóstico y Terapéutico de las Infecciones del Tracto Urinario en la Infancia” (Consensus Conference for the Diagnostic and Therapeutic Management of Urinary Tract Infections in Childhood) designated midstream urine collection as the preferred method in continent children with a grade B strength of recommendation, but they did not address children with no bladder control.13
The British National Institute for Health and Care Excellence (NICE) guidance recommends a clean midstream urine catch for all age groups both for urine testing and microscopy as well as culture.14 In our experience, the spontaneous urine catch in infants and children younger than 3 years is an equivalent method to midstream urine collection in patients with bladder control.
Recently, a new technique to stimulate urination in children without bladder control (in the neonatal period) has been published that involves percussion of the suprapubic and lumbar regions and was shown to be successful in up to 86.3% of patients. An additional goal of the study was to achieve the collection of a urine sample in less than five minutes. The median time elapsed to sample collection was 45 seconds.15
Our study did not find significant differences in the rate of contamination between samples from a spontaneous urine catch and samples obtained by catheterization. However, we must take into account that of the 36 cases of suspected UTI in 2012, 4 corresponded to negative cultures (31%) in the subset of spontaneous urine catch samples (13 of the 36), and a mixed flora or contamination was found in the sample of one patient (7.7%). Similarly, among the samples collected by urinary catheterization (13 of the 36 suspected UTIs), culture results were negative in five cases (38.5%), and a mixed flora was found in none. There were also five patients in whom the urine sample was collected in a bag, and culture was positive in all. As spontaneous urine catch samples in children lacking bladder control are equivalent to midstream urine samples in adults, the contamination rate in this population is around the same. A multicentric study conducted by Bekeris et al that analysed the rate of contamination in 127 laboratories, reported rates of up to 41.7%.16 Cabedo García et al succeeded in reducing the rate of contamination from 56% to 41% by improving the midstream urine collection technique.17
CONCLUSIONS
It is essential that paediatric emergency departments have a sensitive, specific, simple and low-invasiveness method of urine collection for patients lacking bladder control.
The spontaneous urine catch is a painless and easy method in this group of patients, although the need for the family’s cooperation and of using a standardised collection technique must be taken into account. Furthermore, collection of spontaneous urine reduces the time spent waiting in the emergency department, as it is more reliable than collection by means of a bag.
The urine bag collection method requires confirmation in positive cases, often by means of urinary catheterization. Spontaneous urine collection does not require confirmation, thereby preventing catheterization and its associated risks.
There is no evidence of an increase in false-positive UTI diagnoses in patients in whom samples were collected by the spontaneous urine catch method compared to patients in whom samples were collected in a bag, with or without confirmation by urinary catheterization.
Thus, the spontaneous urine catch is an alternative equivalent to midstream urine collection in continent patients that allows for the easy, painless and quick collection of samples that do not require confirmation in patients lacking bladder control with fever of unknown source or suspected UTI.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
ABBREVIATIONS: IMIP: Institute of Maternal and Child Health of Pernambuco • UTI: urinary tract infection • WBC/HPF: white blood cells per high power field.
REFERENCES
- Grupo de trabajo de la Guía de Práctica Clínica sobre Infección del Tracto Urinario en la Población Pediátrica. Guía de Práctica Clínica sobre Infección del Tracto Urinario en la Población Pediátrica. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad, Política Social e Igualdad. Instituto Aragonés de Ciencias de la Salud; 2011. Guías de Práctica Clínica en el SNS: I+CS No 2009/01. Available at www.guiasalud.es/egpc/ITU/completa/index.html
- Romero FJ, Barrio AR. Punción suprapúbica y sondaje vesical. An Pediatr Contin. 2003;1:97-100.
- Craig JC. Urinary tract infection: new perspectives on a common disease. Curr Opin Infect Dis. 2001;14:309-13.
- American Academy of Pediatrics. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128:595-610.
- Dubos F, Raymond J. Pyélonéphrite aiguë du nourrisson: stratégies diagnostiques. Archiv Pédiatr. 2012;19:S101-8.
- Al-Orifi F, McGillivray D, Tange S, KramerMS. Urine culture from bag specimens in young children: are the risks too high? J Pediatr. 2000;137:221-6.
- Grisaru-Soen G, Goldman R, Barzilai A, Lotan D, Keller N. False-positive urine cultures using bag collection. Clin Pediatr (Philadelphia). 2000;39:499-500.
- Hernangómez Vázquez S, Oñoro G, de la Torre Espí M, Martín Díaz MJ, Novoa-Carballal R, Molina Cabañero JC. Complicaciones del cateterismo vesical realizado en un servicio de urgencias para obtener una muestra de orina. An Pediatr (Barc). 2011;75:253-8.
- Karacan C, Erkek N, Senel S, Akin Gunduz S, Catli G, Tavil B. Evaluation of Urine Collection Methods for the Diagnosis of Urinary Tract Infection in Children. Med Princ Pract. 2010;19:188-91.
- Alam MT, Coulter JB, Pacheco J, Correia JB, Ribeiro MG, Coelho MF, et al. Comparison of urine contamination rates using three different methods of collection: clean-catch, cotton wool pad and urine bag. Ann Trop Paediatr. 2005;25:29-34.
- Tosif S, Baker A, Oakley E, Donath S, Babl FE. Contamination rates of different urine collection methods for the diagnosis of urinary tract infections in young children: an observational cohort study. J Paediatr Child Health. 2012;48:659-64.
- González Rodríguez JD, Rodríguez Fernández LM. Infección de vías urinarias en la infancia. Protoc Diagn Ter Pediatr. 2014;1:91-108.
- Ochoa Sangrador C, Málaga Guerrero S; Panel de Expertos de la Conferencia de Consenso; Grupo Investigador de la Conferencia de Consenso. Recomendaciones de la Conferencia de Consenso “Manejo Diagnóstico y Terapéutico de las Infecciones del Tracto Urinario en la Infancia”. An Pediatr (Barc). 2007;67:517-25.
- Urinary tract infection in children Diagnosis, treatment and long-term management. En: NICE [en línea] [consultado el 28/08/2015]. Disponible en www.nice.org.uk/guidance/cg54/resources/guidance-urinary-tract-infection-in-children-pdf
- Herreros Fernández ML, González Merino N, Tagarro García A, Pérez Seoane B, de la Serna Martínez M, Contreras Abad MT, et al. A new technique for fast and safe collection of urine in newborns. Arch Dis Child. 2013;98:27-9.
- Bekeris LG, Jones BA, Walsh MK, Wagar EA. Urine culture contamination. A College of American Pathologists Q-Probes study of 127 laboratories. Arch Pathol Lab Med. 2008;132:913-7.
- Cabedo García VR, Novoa Gómez C, Tirado Balaguer MD, Rodríguez Morquecho N, Rodríguez Bailo MT, Solá Sandtner A. ¿Es importante la técnica de recogida de la orina para evitar la contaminación de las muestras? Aten Primaria. 2004;33:140-4.





