Prevalence and type of electroencephalographic alterations in attention deficit hyperactivity disorder
Raquel Almendral Doncela, F Peinado Postigob
aUnidad de Neuropediatría. Hospital General de Tomelloso. Ciudad Real. España.
bServicio de Neurología/Neurofisiología. Hospital Mancha Centro. Alcázar de San Juan. Ciudad Real. España.
Correspondence: R Almendral. E-mail: raquelalmendral@yahoo.es
Reference of this article: Almendral Doncel R, Peinado Postigo F. Prevalence and type of electroencephalographic alterations in attention deficit hyperactivity disorder. Rev Pediatr Aten Primaria. 2014;16:e133-e138.
Published in Internet: 23-12-2014 - Visits: 23249
Abstract
Introduction: the prevalence and clinical significance of alterations electroencephalographic (EEG) in patients with attention deficit disorder with hyperactivity (ADHD) has not been elucidated.
Objectives: estimate in pediatric patients diagnosed with ADHD and no history of seizures the prevalence and type of EEG abnormalities.
Patients and methods: we selected during 2010 all patients with ADHD seen in a reference Neuropediatric Unit. In all cases an EEG was performed with partial sleep deprivation up to 5 hours and a duration record of 30 minutes by the International System (10/20). We estimated the prevalence and confidence interval of 95% (CI 95%) with the exact method.
Results: we recruited a total of 62 cases, 45 boys (74.2%) y 6 girls (25.8%) with a mean age of 9.2 years (SD 2.6 years, range 6-14 years). Most were ADHD combined type (54.8%), followed by the type attention deficit (33.9%) and hyperactivity (11.3%).Only one case was detected with EEG abnormalities (prevalence 1.6%, CI 95%: 0.04 to 8.7%). It was a male, 7 years old, combined ADHD subtype in which there was a left temporal spike-wave center.
Conclusions: the prevalence of abnormal EEG in patients with ADHD is low in our environment, similar to that expected in the general population.
Keywords
● Attention-deficit hyperactivity disorder ● Electroencephalography ● EpilepsyINTRODUCTION
Attention deficit hyperactivity disorder (ADHD) is a medical and social problem, especially due to its high prevalence in the paediatric population, which ranges between 3% and 10%,1,2 with some studies reporting figures of up to 17.1%.3 In clinical practise, these patients are characterised by patterns of behaviour that diverge from those of the general population, with hyperactivity, impulsivity, and attention deficit. There are different subtypes of ADHD (“inattentive”, “combined” and “hyperactive/impulsive”) with a heterogeneous aetiology; the “inattentive” subtype is atypical and at times does not fit the general understanding professionals have of ADHD.4,5
Patients with ADHD frequently have comorbidities such as anxiety, depression and behavioural problems.6 Authors like Dunn have highlighted the association of specific diseases with ADHD, noting that paediatric patients with epilepsy, in whom attention problems are very prevalent, are at higher risk of ADHD, especially the inattentive subtype.7 Dopamine in the prefrontal cortex (PFC) may play a role in this association, and is considered key in explaining the mechanisms underlying the symptoms of patients with ADHD; neurochemistry studies in nonhuman primates have shown that blocking α2 adrenoreceptors (and interaction with D1 dopamine receptors) recreates the symptoms of ADHD. Current treatments with atomoxetine and methylphenidate is based on this evidence.8
While several studies have analysed the relationship between epilepsy and ADHD,9 few of them have focused on electrophysiological aspects. Generally speaking, children with ADHD, especially the inattentive subtype, have a higher frequency of electroencephalographic abnormalities that is almost double that of the general population.10,11 However, the clinical significance of encephalographic recordings in ADHD remains unclear, and some authors have associated the presence of epileptiform discharges in the electroencephalogram (EEG) with a better response to treatment with methylphenidate and better cognitive function in children with ADHD.12
The aim of this study was to estimate the prevalence and types of paroxysmal abnormalities observed in the EEGs of paediatric patients diagnosed with ADHD with no previous history or signs of epileptic seizures.
PATIENTS AND METHODS
Study health district
The study was conducted in the neuropaediatrics department of the Hospital General de Tomelloso (Ciudad Real, Spain), which serves patients in a predominantly rural area and has a referral population of 67 360 inhabitants, according to the INE estimate for 2009. The Unit of Neuropaediatrics is the only of its kind in this health district, and is the reference unit for ADHD.
Population
We included all patients aged 6 to 14 years, inclusive, that were diagnosed with ADHD based on DSM-VI criteria and the EDAH13 (Evaluación del Trastorno por Déficit de Atención/Hiperactividad) scale during 2010 in our hospital. We excluded patients with associated neurological disorders, epilepsy, or signs of developmental delay.
Methods
An EEG was performed on all patients with ADHD with a 16-channel Nihon Kohden® Neurolg ox EEG-1100 K machine (Nihon Kohden America, Inc.; Foothill Ranch, CA, United States) with partial sleep deprivation to a maximum sleep allowance of 5 hours and a recording time of 30 minutes, placing the electrodes in the positions defined by the 10-20 international system. We defined abnormality as the presence of abnormal graphoelements such as generalised or focal discharges, sharp waves, spikes, spike-wave or polyspike-wave complexes, or interhemispheric abnormalities.
Statistical analysis
We performed a descriptive analysis of the data using measures of central tendency and dispersion (mean and standard deviation [SD]) for quantitative variables, and absolute and relative frequencies, expressed as percentages, for qualitative variables. We compared age and sex between ADHD subtypes by means of the Χ2 test and ANOVA, respectively.
We calculated the prevalence of EEG abnormalities with the software application using the exact method for a 95% confidence interval (95% CI).
Calculations were performed with the software applications PASW® 18.0 (SPSS Inc) and EPIDAT® 3.1 (OPS/Xunta de Galicia).
RESULTS
The study included 62 patients diagnosed with ADHD. Of these patients, 45 (74.2%) were male and 16 (25.8%) were female. The mean age was 9.2 years (SD, 2.6 years; range, 6–14 years). Most of them (54.8%) fit into the combined ADHD subtype, followed by the purely inattentive type (33.9%) and the hyperactive type (11.3%). The male sex predominated in every subtype, although this difference was less marked in the inattentive subtype (Table 1).
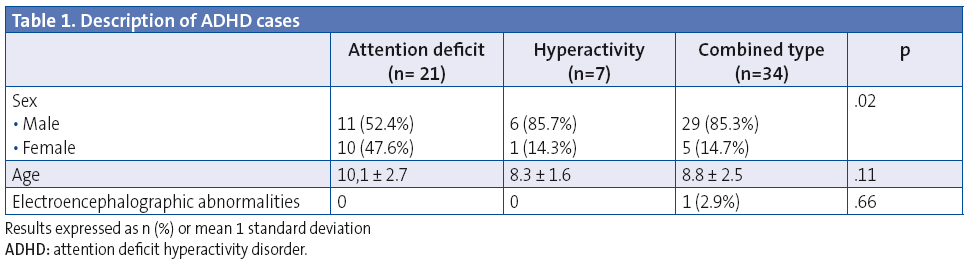
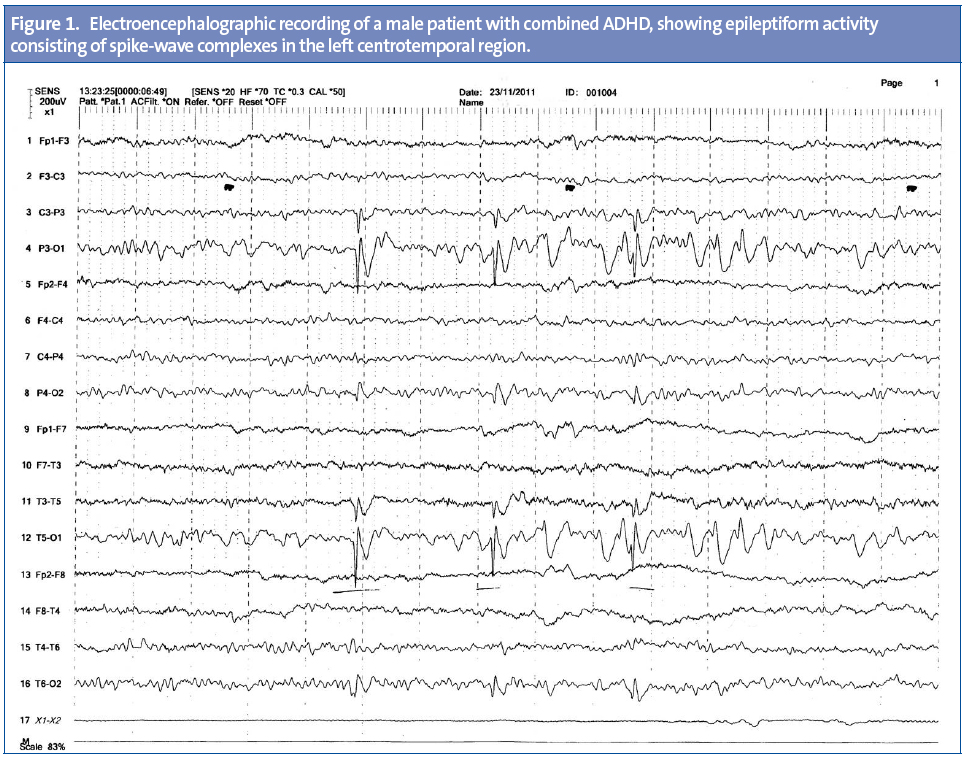
In all patients, the wake EEG showed bioelectrical brain activity consisting of a regular, symmetrical alpha rhythm with closed-open eyes reactivity over both posterior parieto-occipital and temporal regions, and beta activity in the anterior regions. Neither hyperventilation nor intermittent light stimulation provoked any significant changes in the tracing. EEG abnormalities were only observed in one patient (prevalence, 1.6%; 95% CI, 0.04–8.7%). They occurred in a male patient of the combined subtype that showed epileptiform activity consisting in spike-wave complexes in the left centrotemporal region (Figure 1).
DISCUSSION
Our study of 62 patients with no prior history of epilepsy diagnosed with ADHD and assessed by means of a sleep-deprived EEG only found one patient with an epileptiform abnormality, a male with combined type ADHD that had spike-wave complexes in the left centrotemporal region.
The latest findings concerning the aetiology of ADHD have involved genetic and familial factors; one study in particular describes family aggregation that increases the prevalence of ADHD in individuals with first-degree relatives with the disorder by a factor of five to six.14 This seems to suggest that the inheritance of ADHD is multifactorial and polygenic, which results in quantitative effects and a variable disease expression that is influenced by different environmental factors.15,16
The medical literature has reported various anatomical findings in children with ADHD, such as delayed brain development or a reduced brain volume compared to healthy children that support the likelihood of an organic aetiology.17
At the neurophysiological level, a study reported an increase in slow-wave theta activity18 and an absence of fast-wave beta activity when patients were performing tasks that required attention. All of the above showed frontal predominance. Slow-wave activity associated with a reduction in alpha activity, and rolandic, occipital, and bilateral spikes have also been reported.
Our study only found rolandic spikes in one patient (1.3%) a percentage similar to those found by other authors, although according to other studies epileptiform abnormalities are found in 7.5% of children with ADHD.19
There is agreement that patients with EEG abnormalities in whom there is no evidence of clinical seizures do not require anticonvulsant therapy20 and thus stimulant therapy is not contraindicated in them, and also evidence that the use of stimulants is safe in epileptic patients receiving anticonvulsant therapy as long as their seizures are controlled.21
One of the limitations of our study is that language was not one of the variables we studied, even though it would be worth assessing the potential pathophysiological role of these paroxysmal discharges on language and on the behavioural and learning disorders observed by some authors.18,19 We also did not find an increased prevalence of epileptiform abnormalities in children with ADHD uncomplicated by an epileptic condition. At any rate, our results could be due to chance, which suggests the need for studies with larger samples or that use polysomnography.
In conclusion, this descriptive study shows that the prevalence of electrophysiological abnormalities is relatively low.22 Bigger sample sizes in multicentre studies are needed to determine the actual prevalence of these abnormalities in ADHD patients more accurately, and to analyse their clinical significance by correlating electroencephalographic findings with relevant outcome indicators, such as response to treatment or cognitive evolution.23
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this article.
REFERENCES
- Mulas F, Télez de Meneses M, Hernández-Muela S, Mattos L, Pitarch I. Trastorno por déficit de atención e hiperactividad y epilepsia. Rev Neurol. 2004;39:192-5.
- Faraone S, Biederman J, Weber W, Russell R. Psychiatric, neuropsychological, and psychosocial features of DSM-IV subtypes of attention-deficit/hyperactivity disorder: results from a clinically referred sample. J Am Acad Child Adolesc Psychiatry. 1998;37:185-93.
- Pineda DA, Lopera F, Henao GC, Palacio JD, Castellanos F. Confirmación de la elevada prevalencia del trastorno por déficit de atención en la comunidad colombiana. Rev Neurol. 2001;32:217-22.
- Swanson JM, Kinsbourne M, Nigg J, Lanphear B, Stefanatos GA, Volkow N, et al. Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetic and environmental factors and the dopamine hypothesis. Neuropsychol Rev. 2007;17:39-59.
- Baeyens D, Roeyers H, Walle J. Subtypes of attention-deficit/hyperactivity disorder (ADHD): distinct or related disorders across measurement levels? Child Psychiatry Hum Dev. 2006;36:403-17.
- Spencer TJ. ADHD and comorbidity in childhood. J Clin Psychiatry. 2006;67:S27-31.
- Dunn D, Austin JK, Harelak J, Ambrosius WT. ADHD and epilepsy in childhood. Dev Med Child Neurol. 2003;45:50-4.
- Emond V, Joyal C, Poissant H. Neuroanatomie structurelle et fonctionnelle du trouble deficitaire d’attention avec ou sans hyperactivité(TDAH). L’Encéphale. 2009;35:107-14.
- Reilly CJ. Attention deficit hyperactivity disorder (ADHD) in childhood epilepsy. Res Dev Disabil. 2011;32:883-93.
- Richer LP, Shevell MI, Rosenblatt BR. Epileptiform activities in children with attention-defecit hyperactivity disorder. Pediatr Neurology. 2002;26:125-9.
- Socanski D, Herigstad A, Thomsen PH, Dag A, Larsen TK. Epileptiform abnormalities in children diagnosed with attention deficit-hyperactivity disorder. Epilepsy Behav. 2010;19:483-6.
- Millichap JG, Millichap JJ, Stack CV. Utility of the electroencephalogram in attention deficit hyperactivity disorder. Clin EEG Neurosci. 2011;42:180-4.
- Ferré A, Narbona J. EDAH: escala para la evaluación del trastorno por déficit de atención con hiperactividad. En: Farré A, Narbona J (eds). Trastorno por déficit de atención con hiperactividad. Madrid: TEA; 1998.
- Cornejo W, Cuartas M, Gómez-Uribe LF, Carrizosa J. Caracterización clínica y simulaciones de poder para ligamiento genético en el trastorno por déficit de atención con hiperactividad en familias antioqueñas. Rev Neurol. 2004;38:319-22.
- Thapar A, Langley K, Asherson P, Gill M. Gene-environment interplay in attention-deficit hyperactivity disorder and the importance of developmental perspective. Br J Psychiatry. 2007;190:1-3.
- Cardo E, Servera M. Trastorno por déficit de atención/ hiperactividad: estado de la cuestión y futuras líneas de investigación. Rev Neurol. 2008;46:365-72.
- Mulas F, Mattos A, de la Osa-Langreo R. Trastorno por déficit de atención/ hiperactividad: a favor del origen orgánico. Rev Neurol. 2007;44:S47-S49.
- Boutros N, Fraenkel L, Freingold A. A four-step approach for developing diagnostic test in psiquiatry: EEG in ADHD as a test case. J Neuropsychiatry Clin Neurosci. 2005;17:455-64.
- Socanski D, Herigstad A, Thomsen PH, Dag A, Larsen TK. Epileptiform abnormalities in children diagnosed with attention deficit/hyperactivity disorder. Epilepsy Behav. 2010;19:483-6.
- Mantovani J. Treat the patient, not the EEG’? Dev Med Child Neurol. 2000;42:579.
- Gross-Tsur V, Manor O, Van der Meere J, Joseph A, Shalev RS. Epilepsy and attention deficit-hyperactivity disorder: is methylphenidate safe and effectiveness? J Pediatr. 1997:130:40-4.
- Ferrando-Lucas MT. El trastorno del lenguaje como fenómeno epiléptico no paroroxístico. Rev Neurol.2001;2:86-94.
- Deonna T, Zesiger P, Davidoff V, Maeder M, Roulet E. Fenig partial epilepsy of childhood: a longitudinal neuropsychological and EEG study of cognitive function. Dev Med Child Neurol. 2000;42:595-603.






