Vol. 16 - Num. 64
Original Papers
Implementation of an email consultation system to provide solutions, not to create problems
Paula Garvi Solera, Carmen Villanueva Rodríguezb, Esther Andrés Martínezc
aEnfermera. CS Utebo. Zaragoza. España.
bPediatra. CS Torrero-La Paz. Zaragoza. España.
cMIR-MFyC. Hospital Clínico Universitario. Zaragoza. España.
Correspondence: P Garvi. E-mail: pgarvi@salud.aragon.es
Reference of this article: Garvi Soler P, Villanueva Rodríguez C, Andrés Martínez E. Implementation of an email consultation system to provide solutions, not to create problems. Rev Pediatr Aten Primaria. 2014;16:311-6.
Published in Internet: 24-11-2014 - Visits: 16704
Abstract
Objective: digital technologies offer us new possibilities to promote health and management of diseases. We propose to use the e-mail in the pediatric office as a way for opening and improving the communication between the patients and the pediatrician.
Methodology: we created a specific e-mail account, offering it to the assigned families so that they can communicate with their paediatrician. We give them some recommendations and agreements about how to use it correctly.
Results: in these four years, the experiment has being satisfactory for both parts, pedriatricians and families. In an anonymous survey, 90% of the families were happy with this way of communication.
Conclusions: in paediatrics, parents and guardians of children use new technologies and they find it convenient to consult health issues that do not require face to face assessment of the child, all of this with professionals who regularly attend their children without having to make an appointment and travel to the health center. Professionals can provide them thoughtfully and select information they can save to consult at any time.
Before launching a consultation by e-mail it’s important to evaluate how you are going to use this medium, and agree on the practical aspects needed for proper use. It must be decisive for the posed problems and not a source of problems for the professional.
Keywords
● Doctor-patient communication ● e-health ● e-mailINTRODUCTION
On the Internet, patients access a vast amount of advice and recommendations that may disconcert and even confuse them. The primary care provider is the person that should be in charge of this health education process. Furthermore, in its 2001 report, the Institute of Medicine (IOM) stated that “patients should receive care whenever they need it and in many forms, not just face-to-face visits. This implies that the health care system must be responsive at all times, and access to care should be provided over the Internet, by phone and by other means in addition to in-person visits”.1 The Standing Committee of European Doctors (CPME) has specified that electronic mail is a form of telemedicine (remote healthcare delivery by means of mass media), and has provided guidelines for its appropriate use in the practise of what it considers a health care activity.2
The creation of a style manual for the appropriate use of the social networks by doctors was proposed at the I Congreso Nacional de Deontología Médica (I National Congress of Medical Ethics) held this year in Bilbao.
Electronic mail (email) is a convenient tool for patient-doctor communication as long as it is used to supplement care and not as a substitute for in-person communication. Communicating by email may have minimal costs and great benefits. It improves the productivity in the field of primary care (micromanagement).
Ninety percent of patients wish that they could communicate with their doctor by email. Parents make use of this service when it is available.
When the possibility of establishing an email consultation system is being contemplated, its risks and benefits must be taken into account.
The key issue is whether it is worth the time we devote to it. Can it help us provide better care to our patients? How does it impact clinical practice? What are its legal ramifications in relation to the patient-doctor relationship? Among the chief issues to consider are the concerns surrounding its security and threats to confidentiality, and that the patients may use it inappropriately in emergency situations.
Thus, for email to work adequately it is necessary that its correct use is clearly defined for both healthcare providers and families.
METHODS
Utebo is a town near Zaragoza (Spain) with a young population. According to the last census from 2013, 39.45% of its inhabitants are between 30 and 49 years of age. Both parents work in most families.
In June 2010 the healthcare centre of Utebo launched an email consultation system staffed by two providers: a paediatrician and a paediatric nurse.
The objective was to facilitate and expand access to health care to existing patients from the Paediatrics department caseload.
We provided interested families with the email address, which was dedicated solely to this service, along with a sheet with guidelines for its correct use. This sheet suggested situations in which email should be used and what consultations could be done through it (test results, health problems for which it is not necessary to see or examine the child, rescheduling appointments, questions about medication), with the express recommendation that it not be used for emergencies. The sheet informed of the hours and response time of the service (the hours corresponded to the centre’s hours of operation, and responses would be sent within 48 hours except for emails received over the weekend, which would be answered on Mondays). Emails would be answered by the paediatrician or the nurse depending on the type of consultation. Should the paediatrician and the nurse be on vacation at the same time, a notice would be sent to inform the users of this circumstance.
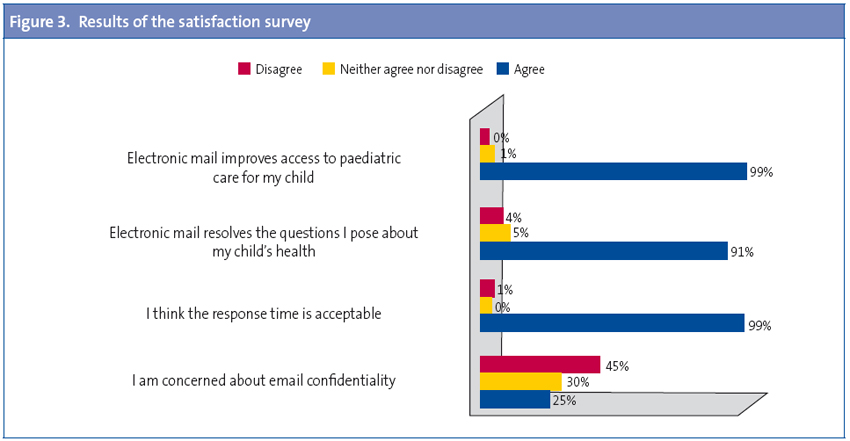
After nearly four years since its introduction, we created and sent a satisfaction survey using Google Drive®, and gave directions to the users for responding anonymously. We included four questions that asked about this means of communication: whether it was helpful, whether it improved access to the doctor, concerns regarding confidentiality and the use of email for health issues, and satisfaction with the response time.
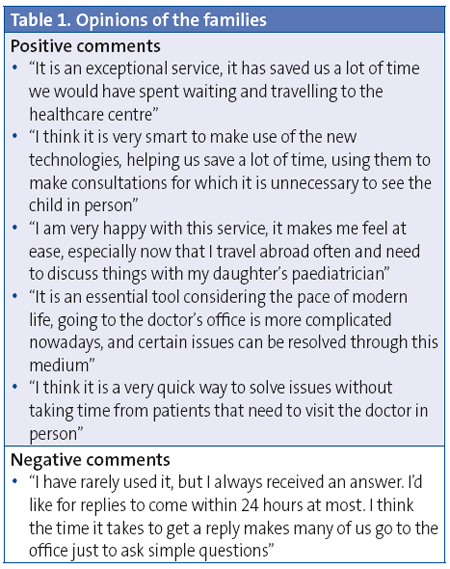
The families expressed their degree of agreement or disagreement. We also asked for their opinions and for suggestions regarding the experience.
RESULTS
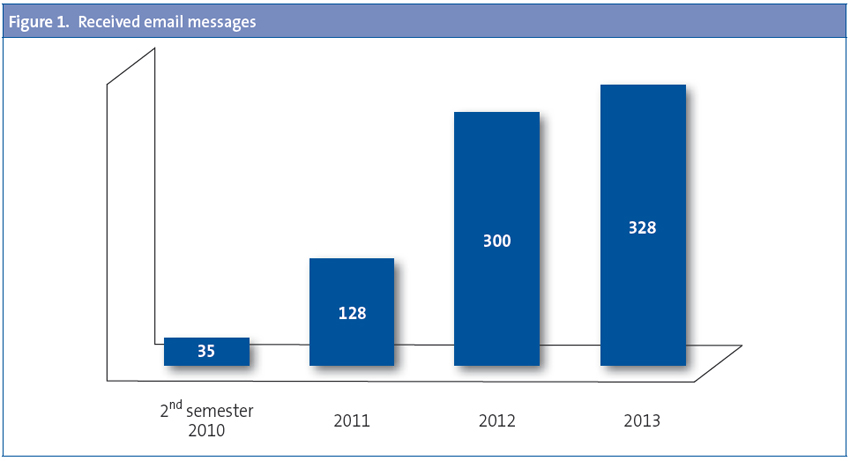
Since the introduction of the system in June 2010 to the present we have received a total of 1027 messages, which, as expected, increased in number as years went by. Figure 1 shows the data through December 2013. We received a mean 1.3 messages a day.
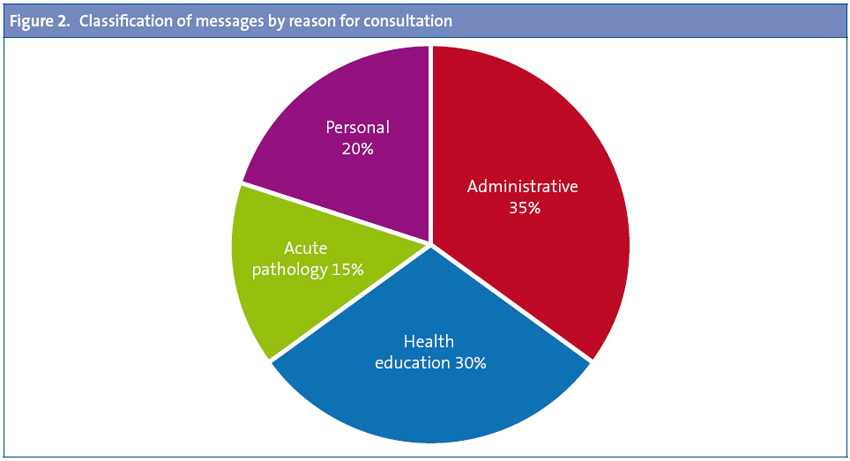
The Gmail® account allowed us to create labels to classify the messages according to the reason for consultation: health education, acute pathology, administrative inquiry, or personal message (Figure 2). Most of the messages we received pertained to administrative matters (appointments, results, prescription issuing or adjustment, etc) and health education (questions about vaccines, diet, etc).
The response time was less than 12 hours, except for messages received over the weekend, which were answered on Monday mornings. We believe that the negative comment of one of the families may be related to this.
The mean time spent by the paediatrician and/or the paediatric nurse answering each message was 3 to 4 minutes (this was a subjective estimation).
There were very few technical problems; only one message was not received by the service, and only 2 to 3 spam messages were received per year.
The satisfaction survey was answered by 58% of the families (Figure 3). Their biggest concern, as expected, was the confidentiality of the data. We also encouraged them to give their opinion in an open-ended question (Table 1).
DISCUSSION
Although technology is still largely underused, paediatricians have adopted the use of electronic mail more successfully than doctors in other specialties. Some examples of this are J. Galbe at the Torrero health care centre in Zaragoza, J. Martínez at Paracuellos del Jarama (Madrid) and the Hospital Gregorio Marañón (Madrid), which has launched a paediatric telemedicine consult that allows other specialists to perform remote visits, among many others.
The use of email can strengthen the patient-doctor relationship, especially since one of the things that patients appreciate most is having access to their doctor.
Email has much potential in terms of the contents it is used to deliver. Responses can be elaborated in greater detail than during a phone conversation. It allows more time for reflection, which makes it a good tool for giving advice or as a reminder of treatment details. Thought is given to the replies, and in fact it is preferable to use email rather than instant messaging for healthcare communications.4 The information remains written and can be re-read, and documents can be sent as attachments (recommendation sheets for parents, links to online resources, guidelines for newborn care or breastfeeding that families may find helpful). It helps patients be more actively involved in their care by providing health-related information that can be useful to the patient and consulted at any time.
The doctor keeps a copy of his or her reply. Written documents contribute to the legal protection of both parties.
Many doctors express concerns about the amount of time it may take to reply to these messages.5 In our study, only 20% of the surveyed doctors believed they would have the time needed to answer emails. But it may actually save the doctor time, especially if it is possible to share this task with another professional (paediatric nurse). Email can increase the efficiency of the doctor and improve the overall efficiency of the healthcare centre. It saves administrative staff time. A specialist clinic measured the time spent by the doctor in reading and replying to emails compared to answering phone calls, and the time spent at the phone was longer, a difference that was statistically significant.1
Doctors can reply to emails when it is most convenient for them. Providers get to control and manage their own time.
While this form of communication may seem impersonal, the families that use it are satisfied with it.
When considering the possibility of setting up an electronic mail consultation system, its advantages and disadvantages must be taken into account. Providers need to be committed if the service is to be successful. Certain rules should be followed to ensure it is an efficacious form of communication and not a source of problems:
- Guarantee the security of the communications:
- A dedicated email account should be created for electronic correspondence.
- Any messages from or to patients should be included in the medical records.
- The staff managing the email account should make sure that the computers and software are used in compliance with the system reliability, updates, and antivirus protection required to avoid the destruction of data by viruses or technical problems.
- It is advisable to use an email application that confirms message delivery, notifies when a message has been opened, and encrypts transferred data (our management of email is not this strict).
- Identification of communicating parties. It is recommended that users always provide their full name, date of birth, and adequate contact information. Reply messages must be signed by the person who writes them. The latter is even more important if the email account is managed by more than one provider.
- It is advisable to establish a protocol and to give guidelines to the patients for its appropriate use. The following information should be given in writing:
- Suggestions of matters that can be addressed through email, and situations in which email should or should not be used. It is important to warn users that email is inappropriate for emergencies or urgent matters. The possible uses of patient-doctor email consultation include the communication of test results and other objective measurements, followup of a chronic disease or a treatment regimen (prescription renewal or change), advice for subacute conditions, health promotion, and administrative matters.
- Have a set response time. It is recommended that it does not exceed 48 hours.
- A notification email must be sent informing of when and for how long the staff are going to be absent.
- As is the case of any communication with the patient, the doctor must prevent any possible misunderstandings. The use of medical terminology should be avoided. For better clarity, the reply should be written above the previous message.
- Set aside the time needed to answer messages. The email account should be checked once a day, and replies should consist of a single message. A chat-like conversation with back-and-forth messages should be avoided.
Patients should always be able to consult in person. Email communications cannot be intended as a substitute for in-person visits, but should be used to address potential concerns.
The advantage of being previously acquainted with the patients, as is the case in primary care, is very important in establishing a service of this kind.
Email consultation is meant to be a supporting tool and not a replacement for in-person visits. This channel does not seem appropriate for all situations, although it provides an invaluable complement to face-to-face communication that may improve the care and monitoring of many patients, in addition to being an ideal medium for health education.
CONFLICT OF INTEREST
The authors declare having no conflicts of interest in relation to the preparation and publication of this paper.
REFERENCES
- Rosen AP, Kwoh KC. Patient-physician e-mail: an opportunity to transform pediatric health care delivery. Pediatrics. 2007;120:701-6.
- Directrices del Comité Permanente de Médicos Europeos (CPME). Directrices del Comité Permanente para la correspondencia mediante correo electrónico en el tratamiento de los pacientes [en línea] [consultado el 23/07/2014]. Disponible en www.cgcom.es/sites/default/files/70_directrices.pdf
- Gerstle RS. E-mail communication between pediatricians and their patients. Pediatrics. 2004;114:317-21.
- Mayer Pujadas MA, Leis Machín A. El correo electrónico en la relación médico-paciente: uso y recomendaciones generales. Aten Primaria. 2006;37:7.
- Pérez Pascual JJ, Jiménez López MD. ¿Qué opinan los médicos de Atención Primaria de la comunicación médico paciente por correo electrónico? Rev Clin Med Fam. 2007;1:256-60.
- Miranda CM, Jadresic ME, Chomali GM, Miranda CE. El uso del correo electrónico en la comunicación médico-paciente. Rev Med Chile. 2013;141:814-5.





