Vol. 17 - Num. 65
Original Papers
Prevalence of breastfeeding in a healthcare centre in Zaragoza (Spain). Social and health factors that influence it
Virgina Giménez Lópeza, Blanca Jimeno Sierrab, M.ª Dolores Valles Pintoc, Encarna Sanz de Migueld
aPediatra. CS Santa Isabel. Zaragoza. España.
bEnfermera. CS Santa Isabel. Zaragoza. España.
cEnfermera y matrona. CS Santa Isabel. Zaragoza. España.
dMatrona. CS Santa Isabel. Zaragoza. España.
Correspondence: V Giménez. E-mail: vgimenezl@salud.aragon.es
Reference of this article: Giménez López V, Jimeno Sierra B, Valles Pinto MD, Sanz de Miguel E. Prevalence of breastfeeding in a healthcare centre in Zaragoza (Spain). Social and health factors that influence it. Rev Pediatr Aten Primaria. 2015;17:17-26.
Published in Internet: 03-03-2015 - Visits: 27632
Abstract
Objective: to describe the current situation of breastfeeding (BF) in our primary care health center and analyze the socioeconomic factors conditioning its maintenance, in order to promote improvement opportunities for the upcoming years.
Materials and methods: descriptive retrospective study of the population monitored from birth date at the Santa Isabel health center (Zaragoza) for 3 years (2010-2012), and followed up until 12 months of age (N:570).
Results: the mean duration of exclusive BF is 2.5 months, and of total BF 5.1 months. The rate of BF is 86.3% at birth, 74% at the 1st month of age, 40.7% at the 6th, and 14.2% at the age of 12 months. Factors related to longer exclusive BF are: larger birth weight and gestational age, singleton pregnancy, and normal childbirth. Higher rates of BF are correlated to mothers’ attendance to childbirth and breastfeeding classes as well as to older mothers.
Conclusions: prevalence of BF in our primary care health center is higher than the previously published data for Spain, but lower than the data for Aragon. BF rates decrease at the 1st month of life as a result of problems at the beginning of BF; and at the 4th-6th month due to mothers returning to work. Factors against exclusive BF are: low weight at birth, prematurity, multiple birth and dystocia/cesarean birth. Attendance of childbirth and breastfeeding classes and older mothers are factors related to longer BF.
Keywords
● Associated factors ● Breastfeeding ● Prevalence ● Primary careINTRODUCTION
Multiple national and international health and scientific institutions recommend exclusive breastfeeding (BF) in the first six months of life, and continued BF up to two years of age, if the mother and child so desire, combined with the adequate introduction of complementary foods.1-4 The decision on how to feed the child ultimately rests with the mother, but healthcare providers must provide parents with adequate information on BF and its benefits and with the necessary support to make BF successful.
Breast milk offers many benefits:5
- Protection against infections and allergies: fewer episodes of diarrhoea, respiratory infections, otitis medias and episodes of atopic dermatitis. Maturation of the digestive tract and intestinal flora.
- Cognitive development.
- Long-term prevention against disease: sudden infant death syndrome, insulin-dependent diabetes, Crohn’s disease, ulcerative colitis, allergies and lymphomas.
- Psychological benefits: facilitates maternal bonding and attachment of the child to the mother.
- Benefits for the mother: promotes weight loss; reduces the risk of anaemia, hypertension and postpartum depression; and reduces the long-term risk of osteoporosis and breast and ovarian cancer.
- Social and environmental impact.
- Economic benefits.
Despite its well-known benefits and the institutional recommendations that promote BF, the initiation and maintenance of BF in our setting have been low in recent decades, far below the rates recommended by the World Health Organization (WHO). This situation may be due to various factors: a lack of information and prenatal and postnatal support of the family; inadequate practises and protocols in maternity wards, primary care (PC) and other care settings; low implementation of the Iniciativa para la Humanización en la Asistencia al Nacimiento y Lactancia en Hospitales y Centros de Salud (Initiative for the Humanisation of Maternity and Infant Care in Hospitals and Healthcare Centres); the lack of training on BF of healthcare providers6; inadequate social and familial support of the mother; inappropriate advertising of breast milk substitutes and distribution of formula samples, bottle nipples and pacifiers in health settings; lack of current legislation supporting breastfeeding mothers that are gainfully employed; social myths and fear of the breastfeeding mother of losing her freedom. The risk is higher in certain social groups (immigrants, parents with low educational levels or single-mother households) and when there are health problems in the newborn, such as low birth weight, preterm birth, or caesarean or multiple deliveries.7
An added problem is the lack of an appropriate official system for the nationwide surveillance and followup of BF that would allow us to know what the current situation is and how it evolves, as well as to assess the effectiveness of the various initiatives implemented to promote and support BF.
The aim of our study was to assess the current situation of BF in our setting and make it known to hospital and PC providers. Thus, identifying weaknesses will help us work together to improve our strategies for the promotion of BF in our population. Consequently, the objectives we set for our study were:
- To analyse the social, public health and healthcare data of newborns and their mothers assigned to the basic healthcare area of Santa Isabel (Zaragoza).
- To determine the prevalence of BF in our healthcare centre (HCC) during the first 12 months of life.
- To study the factors associated with initiation and duration of BF in our setting.
- To propose opportunities for improvement based on the analysis of these data.
MATERIALS AND METHODS
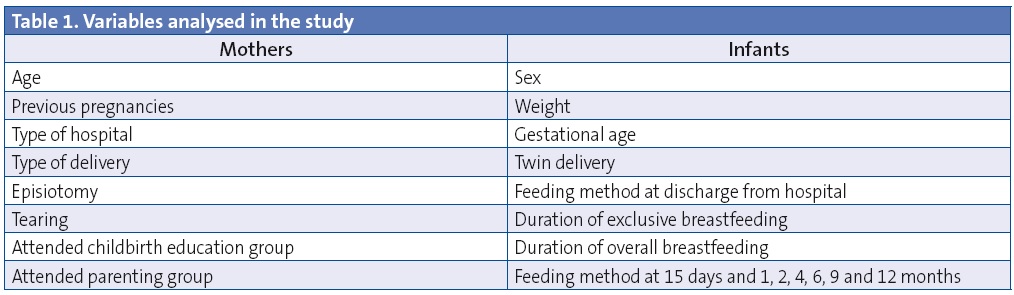
We conducted a retrospective descriptive study of all women that came to the postpartum visit with the midwife of the Santa Isabel HCC (Zaragoza, Spain) over a period of three years (January 2010–December 2012). We collected maternal data from the hospital discharge summaries received by the midwife. On the other hand, we reviewed the electronic medical records of all children born during this period for the first 12 months post birth, collecting data related to BF and the perinatal period. The variables we analysed in mothers and children are listed in Table 1.
We collected the data using the SPSS® 11.5 program, with which we performed the descriptive and statistical analyses. The Kolmogorov-Smirnov test showed that the variables did not follow a normal distribution, so we used nonparametric tests (U de Mann-Whitney) to carry out the statistical analysis.
Conforming to national and international guidelines,8 we defined exclusive breastfeeding (EBF) as feeding the child breast milk alone, mixed feeding (MF) as feeding the child artificial formula in addition to breast milk, and artificial feeding (AF) as feeding the child only artificial formula. Overall BF was calculated by adding the number of children fed by EBF and MF. All of these categories allowed for giving the child medication, infusions or other foods. Thus, infants were classified into these groups based on the type of milk they were fed.
RESULTS
During the three years of the study, a total of 550 mothers had a postpartum visit with the midwife of our HCC: 184 in 2010, 190 in 2011 and 176 in 2012. The mean maternal age was 32.7 years (standard deviation [SD], 3.96; range, 18–43 years), and 34% of the mothers were more than 35 years of age. Approximately half of them were pregnant with their first child at the time of the study. Most of the children (91%) were born in a public hospital, two were born at home, and the rest were born in different private clinics in Zaragoza (8.5%). When it came to the births, 66% were normal vaginal deliveries, 3% were assisted with forceps, 12% were vacuum extractions, and 18.5% caesarean deliveries. Episiotomies were performed in 40% of the mothers, and approximately 21% experienced vaginal tearing during delivery.
During this three-year period, the rate of attendance to the childbirth education group facilitated weekly by the midwife of our HCC was 63%. As for attendance to the parenting group, 4% of the mothers attended 1 or 2 classes, and 14% attended three or more.
The total number of children born during the three years and followed up at the HCC was 570: 193 in 2010, 195 in 2011 and 182 in 2012. The mean birth weight was 3179 g (SD, 548; range, 950–4640 g), with 9% of the newborns weighing less than 2500 g. Of all newborns, 50.7% were boys and 49.3% girls. The mean gestational age was 38.8 weeks (SD, 1.91; range, 27–42), and the rate of preterm birth was 7%. Twenty sets of twins were born during this period, amounting to 7% of the sample.
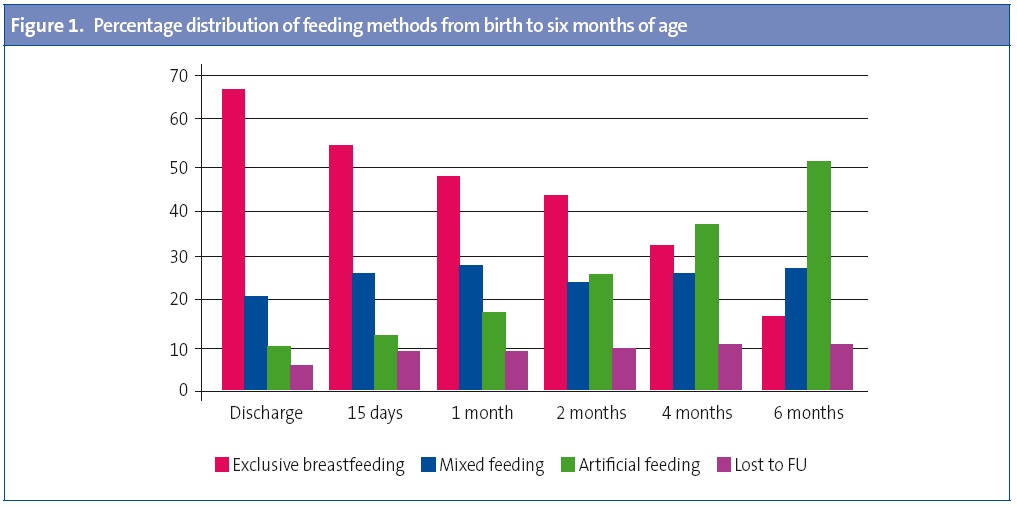
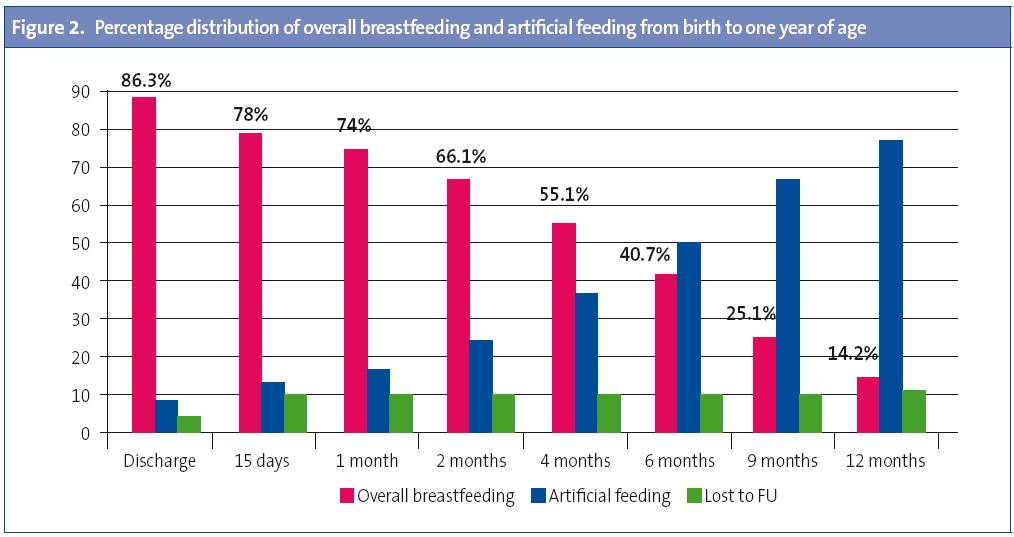
The mean duration of EBF in the first year of life was 2.5 months (SD, 3.25; range, 0–12 months). The mean duration of overall BF was five months (SD, 4.13; range, 0–12 months). Figure 1 shows the prevalence of breastfeeding during the first six months of life at each of the time points analysed. At discharge from hospital, 66.5% of the mothers were feeding their babies with EBF, 19.8% with MF, and 8.9% with AF. The EBF rates had declined to 53.3% at 15 days post birth, to 47.5% at 1 month, to 42.6% at 2 months, to 30% at 4 months and to 15.8% at six months post birth, while mixed feeding and artificial feeding increased, as shown in Figure 1. Figure 2 shows the prevalence of overall BF in the first 12 months of life. We can see that 86.3% of the mothers practised some type of BF at discharge, which had dropped to 66.1% at 2 months, 55.1% at 4 months, and 40.7% at 6 months; and was down to 14.2% at 1 year post birth. Thus, BF was the prevailing feeding method in the first 4 months of life, but starting at 6 months the rate of artificial feeding became higher.
The factors for which we observed a statistically significant association with continuation of EBF in our study were (Table 2): birth weight greater than 3 kg (P < .001), gestational age greater than 37 weeks (P < .01), singleton birth (P < .001) and normal vaginal delivery as opposed to caesarean or assisted delivery (P < .001).
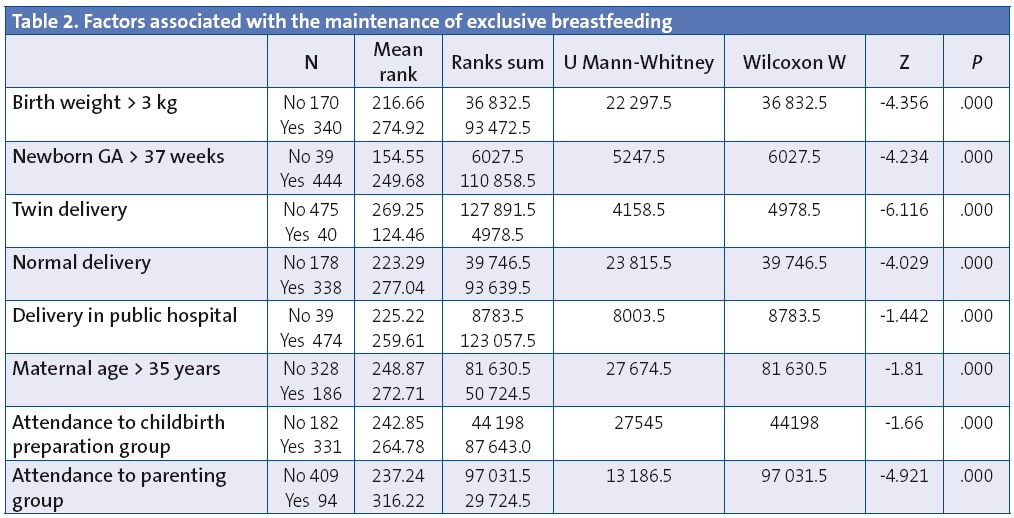
The duration of overall BF (Table 3) was not significantly associated with the factors mentioned above, and instead seemed to be associated with maternal age—with the longest durations of BF seen in mothers of more than 35 years of age (P < .01)—and with attendance to the childbirth education group (P < .05).
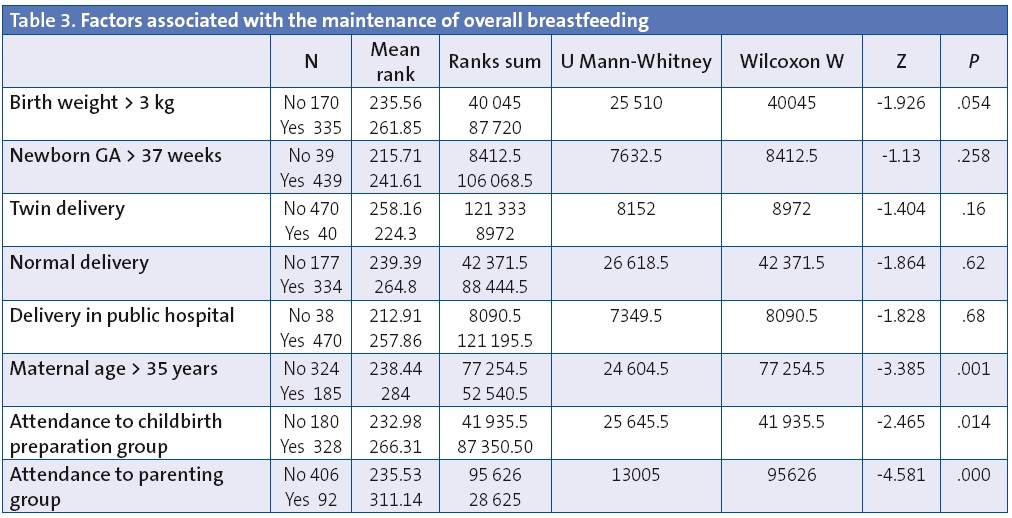
Attendance to the parenting group facilitated by the midwife of our HCC was the factor that most influenced the duration of BF over time, as it was associated with higher rates of EBF (P < .001) and overall BF (P < .001).
We found no statistically significant association between the type of hospital where the child was born and the different feeding methods in our setting.
DISCUSSION
International recommendations advocate for EBF until 6 months of age and BF with complementary foods until two years of age.
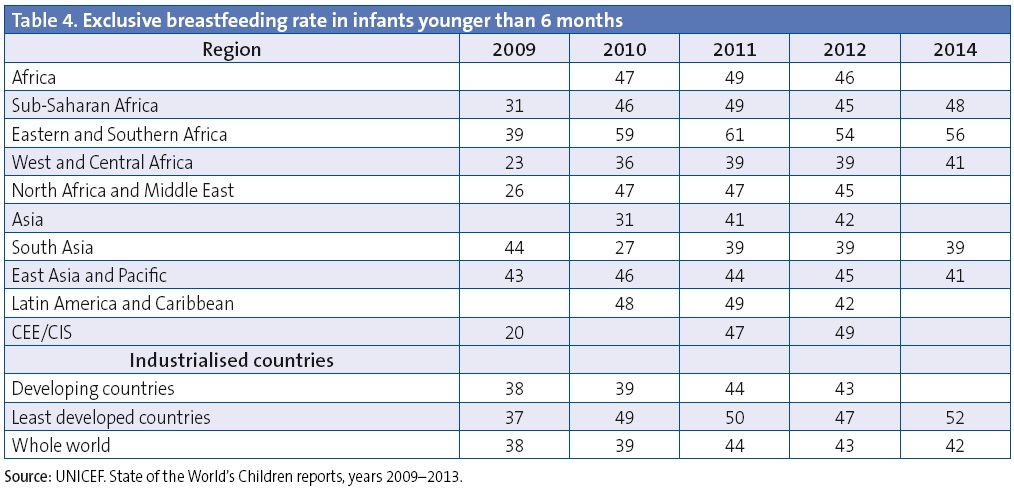
The WHO and the United Nations Children’s Fund (UNICEF) recommend the periodic collection of data on breastfeeding to learn how it is evolving, and on initiatives for the promotion and support of breastfeeding.9 Table 4 shows the prevalence of EBF in infants younger than six months according to the State of the World’s Children reports published by UNICEF10 in the past five years. We can see how the figures improve with time, especially in developing countries, with the highest rates of BF in the world found in Africa. There is very little data from Europe for these years, and a total lack of data from industrialised countries. We think this may be due to a low incidence and prevalence of breastfeeding, and a lack of interest in measures to promote it.
At present, Spain lacks an official system to follow up and monitor BF, and the data available for the country comes from studies of a local scope. The first study conducted in Spain with a large set of data was pursued by the Comité de Lactancia Materna (Committee on Breastfeeding [CLM]) of the Asociación Española de Pediatría (Spanish Association of Pediatrics [AEP]) in 1997.11 It gathered the data of 12 156 questionnaires distributed in 18 provinces. According to the published results, the prevalence of BF was 84.2% at birth, 65.8% at 2 months, 42.1% at 4 months, and dropped to 24.8% at 6 months, and the total duration of BF for the survey participants was of 3.2 months. The BF rates found in our study are higher than those, especially at 4 and 6 months, and the total duration was also two months longer in our study (5.1 months in our study versus 3.2 in the CLM-AEP study). This reflects a current increasing trend in BF compared to the data of the study published 15 years ago.
The most recently published data on BF in Spain come from the 2006 Encuesta Nacional de Salud (National Health Survey) of the Instituto Nacional de Estadística (National Institute of Statistics).12 According to this study, the BF rates would be 70.4% at 6 weeks, 63.3% at 3 months, and 38.7% at 6 months, above the rates reported in the CLM-AEP study but below those found in our study. In contrast, it reported higher rates of EBF compared to our study, nationwide and for Aragón (at 6 months, 24.7% in Spain and 27.85% in Aragón, compared to 15.8% in our study). According to the same study, the autonomous communities with the highest rates of BF both at 6 weeks and 6 months are La Rioja and the Basque Country.
Among the studies conducted in the autonomous community of Aragón, the most salient is the recently published CALINA study,13 which assessed the prevalence of BF in Aragón during the first year of life. The study analysed a cohort representative of the infant population in Aragón, born between March 2009 and March 2010 in different health facilities across the autonomous community (n = 1602). The study reported a rate of overall BF of 82.5% at 1 month of age, 71.8% at 3 months, 54.3% at six months and 27.8% at twelve months. These rates are far above the rates found in our study, and greater differences are found starting at 4 and 6 months of age, concurrent with the reincorporation of mothers to the workforce. The rate of continued BF at one year of age is also considerably higher in Aragón, according to the CALINA study,13 than in our setting.
The rates of EBF in the CALINA study13 are approximately 71% at birth, 50% at 2 months, 48% at 4 months, and have dropped to 16% at six months of age. These rates are also above the rates found in our study, but at 6 months of age there was a considerable decline that approximates the rate observed by us (16% in the CALINA study13 compared to 15.8% in our study).
From these data, we can infer that the mean duration of BF in our healthcare centre is higher than the one assessed from data published for Spain in 1997 and 2006, but it is still short and below the rates reported for our autonomous community. BF is frequently discontinued in the early weeks post partum due to problems establishing BF at the hospital and the lack of social and healthcare support in the first few days. In our healthcare centre, the first checkup for the newborn is scheduled late, at around 7 to 10 days post birth. We believe that the postnatal visit should take place within 48 to 72 hours after discharge from the maternity ward, and at the latest by one week, as this is associated to higher rates of BF and lower morbidity in the neonatal period (hypernatraemic dehydration, pathological jaundice…) according to the recently published report by the Grupo Asesor Técnico para la Pediatría de Atención Primaria (Technical Consulting Group for Primary Care Paediatrics [GATPAP]).14 Furthermore, few mothers achieve six months of EBF, as returning to work still poses a significant barrier to BF continuation and is one of the main reasons for cessation, according to various studies.15
As for the factors that contribute to BF continuation, our study found a significant association with birth weights of more than 3 kg and gestational ages above 37 weeks, findings that have been reported in several other studies.9,11,16,17 Consequently, BF rates are lower in preterm and low-birthweight newborns, the populations that research shows derive the most benefit from breastfeeding. The separation of these newborns from their mothers should be avoided, as should be the initiation of artificial feeding, which could be replaced by the extraction and storage of breast milk, and strategies like the “kangaroo care” approach should be implemented.
In our study, the rate of EBF was also associated with the type of delivery, and was higher for normal vaginal deliveries compared to dystocic and caesarean deliveries. This finding has also been reported by numerous Spanish and international studies.9,11,18,19 According to a Cochrane review published in 2000,20 there is no scientific explanation for this fact, so we should start changing certain hospital practises to improve this situation, reducing the rate of caesarean deliveries (which has increased considerably in recent years and is above the 15% rate recommended by the WHO21), facilitating early mother-child contact following dystocic or caesarean deliveries, and avoiding the administration of unnecessary medications and supplements, among others.
In our study, the duration of BF was associated with maternal age, with the highest durations of BF found in the oldest mothers (more than 35 years of age). Several studies9,22 show similar results: younger mothers have lower rates of BF initiation and durations of BF, and this is most pronounced in adolescents.
The most interesting and novel data in our study had to do with attendance to antenatal and postnatal workshops facilitated by our centre’s midwife. We found a higher rate of BF in mothers that attended the childbirth education group (63% of the sample) and a higher rate of EBF and overall BF in mothers that attended the parenting group (18%). Usually, most mothers make the decision to breastfeed during the first trimester of the pregnancy, or even before, although many make it at the end of the pregnancy or even after delivering. Different studies have shown that educational support on BF to mothers, delivered before or after birth, improves the proportion of mothers that maintain EBF in the long-term.23,24Therefore, the HCC should review the childbirth education and parenting groups in terms of their organisation, promotion, and evaluation through questionnaires to increase attendance to these groups, especially to the parenting group, for which attendance is low at the moment.
CONCLUSIONS
The low prevalence of EBF at the time of discharge and during the first month of life reflects difficulties in initiating BF at the hospital and high rates of early BF discontinuation. We observed a significant decline in EBF at around 4 to 6 months of age, coinciding with the return of mothers to the workforce. The prevalence of BF in our healthcare centre is lower than the one reported based on the most recent published data for Aragón (CALINA study, 2013)13, although it is higher compared to the most recent national data. The factors that have a negative impact on the initiation and maintenance of EBF in our setting are low birth weight, preterm birth, twin delivery and dystocic or caesarean delivery; while attendance to the childbirth education group or the parenting group and older maternal age are associated with the longest durations of BF. It is essential that we foster the involvement of all professionals in the HCC in the promotion of childbirth education and parenting groups, and that we push the neonatal visit forward to the first few days of life to achieve better BF rates in our area in upcoming years. To succeed in our objectives, we started giving educational talks on BF and related subjects in our centre a few months ago.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare in relation to the preparation and publication of this paper.
ABBREVIATIONS: AEP: Asociación Española de Pediatría (Spanish Association of Paediatrics); AF: artificial feeding; BF: breastfeeding; EBF: exclusive breastfeeding; GATPAP: Grupo Asesor Técnico para la Pediatría de Atención Primaria (Technical Consulting Group for Primary Care Paediatrics); MF: mixed breastfeeding; PC primary care; SD: standard deviation; UNICEF: United Nations Children’s Fund; WHO: World Health Organization.
REFERENCES
- Hernández MT, Aguayo J. La lactancia materna: cómo promover y apoyar la lactancia materna en la práctica pediátrica. Recomendaciones del Comité de Lactancia de la AEP. An Pediatr (Barc). 2005;63:340-56.
- Gartner BF, Morton J, Lawrence RA, Naylor AJ, O'Hare D, Schanler RJ, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496-506.
- Nutrición del lactante y del niño pequeño. Estrategia mundial para la alimentación del lactante y del niño pequeño. Informe de la Secretaría. Organización Mundial de la Salud. 55ª Asamblea Mundial de la Salud. [en línea] [consultado el 26/02/2015]. Disponible enwww.ministeriodesalud.go.cr/gestores_en_salud/lactancia/CNBF_estrategia_mundial.pdf
- Innocenti Declaration on the Protection, Promotion and Support of Breastfeeding. En: UNICEF [en línea] [consultado el 26/02/2015]. Disponible enwww.unicef.org/spanish/nutrition/index_24807.html
- Pallás Alonso CR, Grupo PrevInfad/PAPPS. Promoción de la lactancia materna. Recomendación. En: Recomendaciones PrevInfad/PAPPS [en línea] [actualizado el 5/06/2013, consultado el 26/02/2015]. Disponible en www.aepap.org/previnfad/rec_lactancia.htm
- Palomares Gimeno MJ, Labordena Barceló C, Sanantonio Valdearcos F, Agramunt Soler G, Nácher Fernández A, Palau Fuster G. Opiniones y conocimientos básicos sobre lactancia materna en el personal sanitario. Rev Pediatr Aten Primaria. 2001;3:393-402.
- Hernández Aguilar MT, Muñoz Guillén A, Lasarte Velillas JJ, García Vera C, Díaz Marijuán C, Martín Calama J. La lactancia materna en la Comunidad Valenciana. Análisis multivariante de una encuesta a 6.400 lactantes. Rev Pediatr Aten Primaria. 2004;6:19-37.
- Hernández Aguilar MT. Herramientas básicas para el diseño y lectura crítica de estudios sobre lactancia materna. En: Comité de Lactancia Materna de la Asociación Española de Pediatría, editor. Manual de Lactancia. De la teoría a la práctica. Madrid: Editorial Médica Panamericana; 2008. p. 33-9.
- Hernández Aguilar MT. Epidemiología de la lactancia materna. Prevalencia y tendencias de la lactancia materna en el mundo y en España. En: Lactancia materna: Guía para profesionales. Comité de BF de la AEP. Monografía n.º 5. Madrid: Ergon; 2004. p. 31-43.
- Informes del Estado Mundial de la Infancia, años 2009-2013. En: UNICEF [en línea] [consultado el 26/02/2015]. Disponible en www.unicef.org/spanish/sowc/
- Comité de Lactancia Materna de la Asociación Española de Pediatría. Informe técnico sobre la lactancia materna en España. An Esp Pediatr. 1999;50:333-40.
- Grupo de Trabajo CS-IHAN, Hernández Aguilar MT, González Lombide E, Bustinduy Bascarán A, Arana Argüelles-Cañedo C, Martínez-Herrera Merino B y cols. Centros de Salud IHAN (Iniciativa de Humanización de la Atención al Nacimiento y la Lactancia). Una garantía de calidad. Rev Pediatr Aten Primaria. 2009;11:513-29.
- Cuadrón Andrés L, Samper Villagrasa MP, Álvarez Sauras ML, Lasarte Velillas JJ, Rodríguez Martínez G. Grupo Colaborativo CALINA. Prevalencia de la lactancia materna durante el primer año de vida en Aragón. Estudio CALINA. An Pediatr (Barc). 2013;79:312-8.
- Asensi Monzó M, Fabregat Ferrer E, Gutiérrez Sigler MD, Soriano Faura FJ. Atención en las primeras 48 horas tras el alta de maternidad en la consulta de enfermería o Pediatría. Rev Pediatr Aten Primaria. 2014;16:117-24.
- Guerrero C, Garafulla J, Lozano D, García C, Bielsa A. Estudio lactancia en Área Hospital de Alcañiz. ¿Merece la pena poner en práctica los diez pasos de la iniciativa hospital amigo de los niños en un hospital comarcal? Bol Pediatr Arag Rioj Sor. 2006;36:20-6.
- Galbe Sánchez-Ventura J, Gracia Torralba L, Metola Loza J, Mateo Ferrando A, Sánchez-Erce M, Traver Cabrera P. Atención a los recién nacidos en 2009 y a sus madres en un centro de salud urbano de Zaragoza. Oportunidades de mejora. Rev Pediatr Aten Primaria. 2012;14:101-6.
- Palomares Gimeno MJ, Fabregat Ferrer E, Folch Manuel S, Escrig García B, Escoín Peña F, Gil Segarra C. Apoyo a la lactancia materna en una zona básica de salud; prevalencia y factores sociosanitarios relacionados. Rev Pediatr Aten Primaria. 2011;13:47-62.
- Cuestas Montañes E, Aparicio Sánchez JL. Los niños nacidos por cesárea toman menos lactancia materna. Evid Pediatr. 2011;7:15.
- Aguayo Maldonado J, Romero Escós D, Hernández Aguilar MT; Comité de Lactancia Materna de la AEP. Influencia de la atención al parto y al nacimiento sobre la lactancia, con especial atención a las cesáreas. Evid Pediatr. 2011;7:2.
- Renfrew MJ, Lang S, Woolridge MW. Early versus delayed initiation of Breastfeeding (Cocharane Review). Cochrane Database Systematic Review; 2000. CD000043.
- Instituto de Información Sanitaria. Sistema Nacional de Salud. Ministerio de Sanidad, Servicios Sociales e Igualdad [en línea] [consultado el 26/02/15]. Disponible en www.msssi.gob.es
- Estévez González MD, Martell Cebrián D, Medina Santana R, García Villanueva E, Saavedra Santana P. Factores relacionados con el abandono de la lactancia materna. An Esp Pediatr. 2002;56:144-50.
- García Vera C, Esparza Olcina MJ. Las intervenciones dirigidas a promocionar y mantener la lactancia materna son efectivas si se realizan antes y después del nacimiento y con apoyo de personal no sanitario. Evid Pediatr. 2009;5:16.
- Aparicio Rodrigo M, Balaguer Santamaría A. Con breves sesiones de educación sanitaria pueden aumentarse las tasas de lactancia materna exclusiva. Evid Pediatr. 2007;3:93.





