Advice or prescription? Analysis of the pediatric recommendations in the healthy child program visits
Cristina Nunesa, Mariano Ayalab
aProfesora asociada. Centro de Investigação sobre Espaço e Organizações, Universidade do Algarve. Campus de Gambelas. Portugal.
bMédico, especialista en Salud Pública. SErvicio de Salud Pública. CS de Castro Marim. Portugal.
Correspondence: C Nunes. E-mail: csnunes@ualg.pt
Reference of this article: Nunes C, Ayala M. Advice or prescription? Analysis of the pediatric recommendations in the healthy child program visits. Rev Pediatr Aten Primaria. 2013;15:305.e135-e143.
Published in Internet: 09-01-2014 - Visits: 21716
Abstract
Introduction: reasoning the recommendations increases mothers’ adherence and satisfaction in the healthy child program visits. A recommendation can be considered an advice or a prescription according to its reasoning.
Aims: in this study we described and analyzed the use of advice and prescription in the recommendations made by pediatricians to mothers in the healthy child program visits. We analyzed the quantity and quality of recommendations, its content and its relation to the visits’ duration, and the characteristics of the child and mother.
Methods: we audio-taped 50 visits of five pediatricians and we classified, through content analysis, the recommendations in six categories: secondary prevention, primary prevention, health promotion, development, education and family relationships.
Results: pediatricians made 4.37 recommendations per visit, 69% by their own initiative and 31% by mothers’ request. Pediatricians make recommendations mainly about health promotion (32.87%), secondary prevention (17.13%) and primary prevention (10.19%). The amount of recommendations was positively associated with the visit’s length (M=16.10 minutes) and negatively related with child’s age. The pediatricians used much more advice (70%) than prescription (30%). The effect of the mothers’ educational level wasn’t observed.
Conclusions: there was a great heterogeneity between pediatricians in all observed variables; this suggests that there exist different pediatric styles whose characteristics and effects deserve further investigation in future studies in order to help pediatricians to improve their professional practice.
Keywords
● Advice ● Child program ● Pediatricians ● Prescription ● Primary care ● RecommendationsINTRODUCTION
Paediatricians are the main technical source of counselling for parents in the development and education of their children1-6, and in Andalusia they operate within the institutional framework of the well-child programme. The programme tasks paediatricians with the prevention, early detection, and treatment of diseases and abnormalities in development, but also with supporting parents in the education of their children toward the acquisition of healthy habits7. However, there is limited knowledge about the specific manner in which paediatricians make these recommendations and of their contents. Although they are hardly taken into account in paediatrics education and research, well-child visits, in which health-promoting and disease-prevention activities are carried out, constitute a central aspect of the paediatric practise8.
The paediatric agenda is organised according to a biomedical perspective in which psychosocial and educational issues are deemed secondary9-15. Still, paediatricians adhere to the general principles of health promotion9,16 and the American Academy of Pediatrics17 considers that psychosocial issues are growing in significance due to their frequency and relevance.
On the other hand, there is ample empirical evidence that mothers wish they were given more information than they actually receive5,12,14,18 and that child development and education were addressed more during visits2,19.
Interpersonal communication between mothers and paediatricians is important because it has an effect on the outcomes of paediatric healthcare. The effectiveness of such communication is correlated to the mothers’ satisfaction, compliance with paediatrician recommendations, and the discussion of psychosocial issues2,20-25. On the other hand, a lack of information, receiving erroneous information, and a lack of sensitivity towards their needs are the main complaints expressed by mothers22,23,25,26.
Efficient communication is based on the use of techniques that help express parental doubts and concerns and promote understanding of and compliance with doctor recommendations. One technique that is very important is explaining the guidelines and the reasons behind them21,22,24,27. Explaining the rationale for recommendations helps mothers integrate them in a coherent account of the enormous set of factors that determine the health, development, and education of their child.
A medical recommendation can be given as counselling or as prescription21,27. We define counselling as giving guidelines in a reasoned-out or detailed manner, and prescription as making the recommendation without explaining its purpose or the set of causal relationships into which it fits.
The validity of most studies in this field is affected by the use of self-administered questionnaires or telephone surveys. It limits the inferences that can be made regarding communication characteristics and quality, and underscores the need for studies based on the direct observation of healthcare visits.
The purpose of this study is to describe and analyse the use of counselling and prescription in the recommendations made to mothers in the context of the well-child programme by analysing integral recordings of the visits. We studied the quantity and quality of the recommendations, their content, and their relationship to the duration of the visit and the mother and child characteristics.
MATERIALS AND METHODS
Participants
We observed 50 visits with five paediatricians (one male and four females) selected from three healthcare districts in the province of Seville (Spain), with a mean age of 45.6 years (standard deviation [SD] 9.48; minimum [min.] 34; maximum [max.] 63) and 16.8 years of professional experience. The selection criteria were accessibility and having more than five years of professional experience in Primary Care. All the paediatricians we contacted agreed to participate.
The mean age of the children who came for the visits was 16.48 months (SD 18.45; min. 0.33; max. 60), the mean age of the mothers was 32.05 years (SD4.16; min. 22; max. 41) and they had completed 9.7 years of education on average (SD 2.71; min. 8; max. 15).
Procedure
After obtaining the necessary authorizations and the informed consent of the mothers, we observed and audio-recorded the first ten consecutive visits already scheduled in the appointment calendar of the healthcare centre. The recordings were fully transcribed and then analysed to make qualitative and quantitative descriptions of the recommendations given by the paediatrician and those requested by the mothers. We excluded one of the visits because the constant crying of the child made transcribing it impossible.
To quantify the recommendations, we used the significance criterion. Thus, a recommendation given by the paediatrician can consist of a single sentence: “Don’t use the walker, because it causes accidents at home and can hurt the hips” or be developed in several sequential sentences, for example to introduce the topic of psychomotor development: “The important thing right now is to stimulate her. As for her [a different sister], she does not need it, she’s doing quite well. (…) But you also should not force them to stand. Nor do anything that does not fit their age. Right now their development is exactly what is expected for their age”.
As we noted before, we differentiate between two types of recommendation: counselling and prescription. We understand counselling as giving guidelines along with a rationale for them or in a detailed manner, that is, using at least one of the following explanations: a detailed account of the proposed course of action, examples, and explaining the reasons for doing it. The counselling can address behaviours, feelings, and ways to manage problems such as diseases or discomfort. In the two following examples, they explain the rationale for avoiding a behaviour that has a causal relationship with unwanted outcomes:
“Don’t use the walker, because it causes accidents at home and can hurt the hips” (paediatrician 1, visit 4).
“Well, you see, he’s quite a restless boy, right?, and it is quite common for this kind of kid to stutter when he is three or four, you know? Because they just go really fast and they cannot articulate what they want to say properly, you see? It’s quite common and it’s perfectly fine. It’s going to go away, unless you traumatise him, nagging him and pushing him, which is what we used to do before, and then the stutter remained for life. What you need to do when you see that he is a bit overexcited and having trouble organising his words is tell him, ‘don’t worry, you can tell me later’. And later on, when he is calmer, he tells you. Don’t let anyone in the family push him” (paediatrician 3, visit 3).
By comparison, we define prescription as those recommendations given without an explanation of their purpose or the causal chain into which they fit, as happens in the following examples:
“You should control a bit what television programmes they watch” (paediatrician 1, visit 3).
“Is the child still using the pacifier or not? (...) You can start withdrawing it soon” (paediatrician 3, visit 7).
We grouped the topics of the recommendations into the following broad categories: secondary prevention, primary prevention, health promotion, development, education, and parenting and the family relationship, which are articulated around two axes: the natural history of disease and psychosocial development (Table 1).
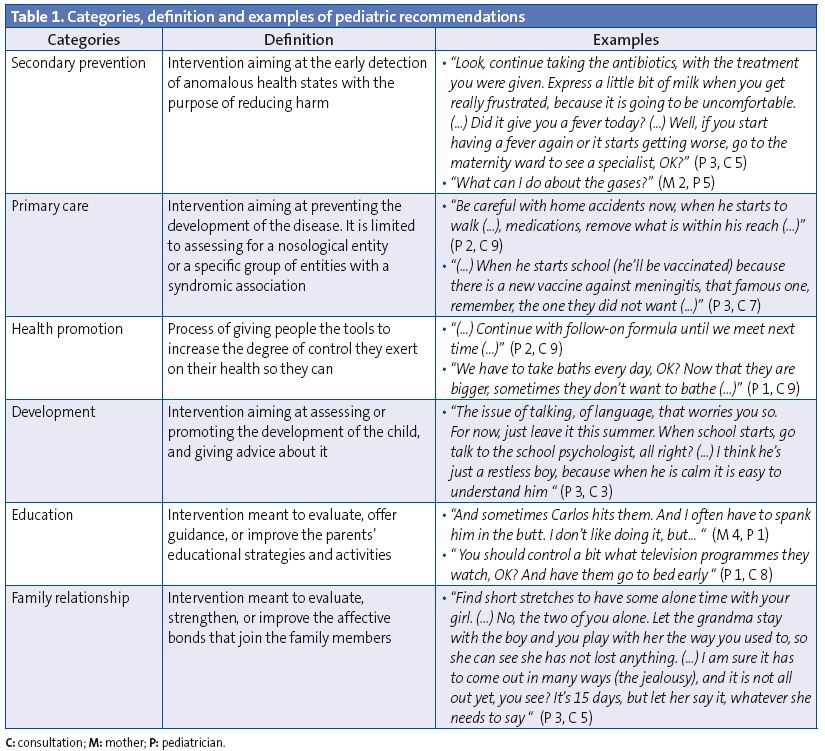
The face validity (clarity and relevance) of the list of categories can be estimated according to their definition (Table 1). The content validity was satisfactory, as all segments of the transcribed text fit into the defined categories. The principal investigator and a trained research assistant analysed and codified every visit independently. Disagreements were infrequent (<3% of observations) and were resolved by consensus.
The codification, tabulation, and graphic representation of the data were done in Excel® and the statistical analysis performed with SPSS® v.18. We used the following measures in our descriptive statistical analysis: mean (M), standard deviation (SD), coefficient of variation (CV), minimum (min.) and maximum (max.). In our inferential statistical analysis we used the chi-squared test (Χ2), ANOVA (F), Pearson’s coefficient (r) and linear regression (R2). The independent variables under study were: paediatrician, age and sex of the child, age, and mother’s educational level.
RESULTS
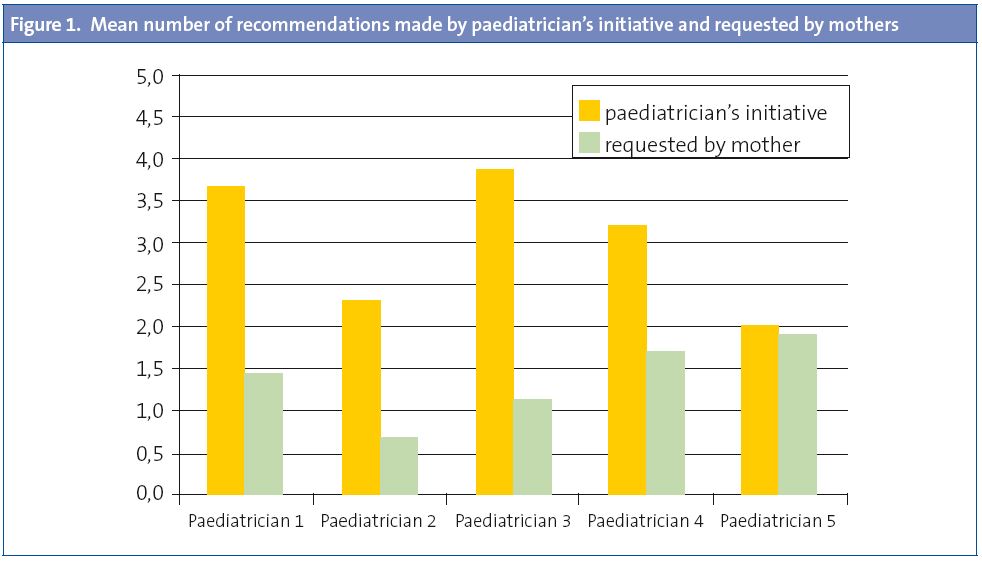
Paediatricians made some recommendations in nearly every visit (46 out of 49; 94%). Of a total of 214 recommendations, 147 (69%) were the result of the paediatrician’s initiative, while 67 (31%) were sought by the mothers. This amounts to 4.37 recommendations per visit (SD 2.83, min. 0, max. 11), three of which were given by the paediatrician’s initiative (SD 2.15, min. 0, max. 8) and 1.4 requested by the mothers (SD 1.57, min. 0, max. 8). In Fig. 1 we observe a wide variation between paediatricians in the distribution of the initiative for giving the recommendations (CV for paediatrician initiative 24%, CV for mother initiative 32%, Χ2 107.00; p=0.0009).
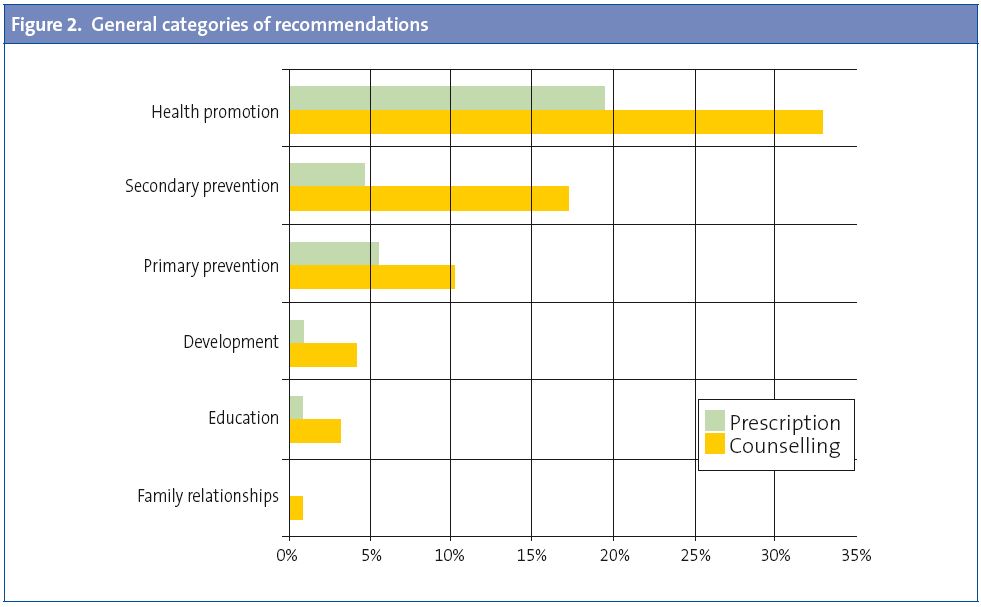
When we analysed the contents assigned to the general categories, we observed that the paediatric agenda was mostly focused on biomedical aspects (Fig. 2). Paediatricians made recommendations for the purposes of health promotion most frequently (32.87%), followed by secondary (17.13%) and primary prevention (10.19%). Development (4.17%), education (3.24%), and family relationships (0.93%) were barely the subject of occasional recommendations (Χ2 237.89; p=0.000).
The mean duration of the visits was of 16.1 minutes (SD 5.72, min. 6, max. 24). There was a significant difference between paediatricians (F 4.55; p=0.004). The duration showed a strong positive correlation to the number of recommendations, with a new recommendation occurring every three minutes (r 0.556; p=0.00003).
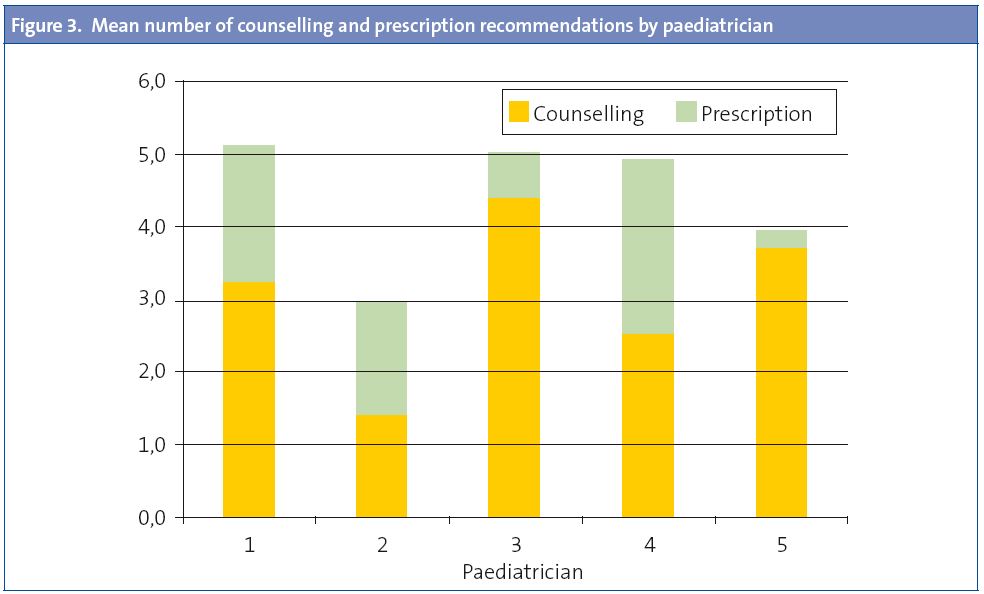
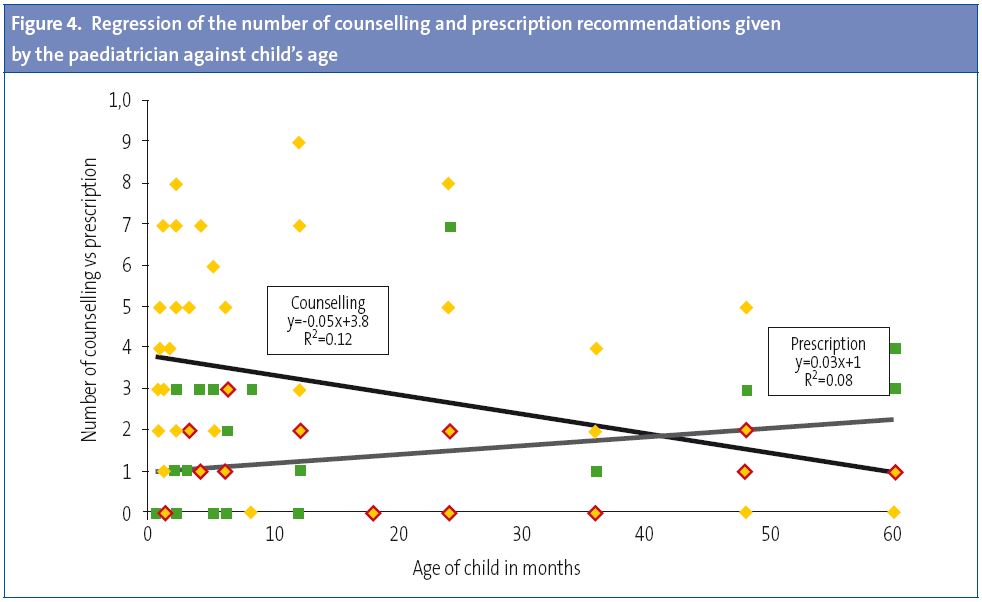
As we have said above, when it comes to recommendations it is important to distinguish between counselling and prescriptions. Paediatricians used counselling (149/214; 70%) more often than prescription (65/214; 30%) (Χ2 32.97; p=0.000). In each visit, an average of 3.04 counselling recommendations (SD 2.51, min. 0; max. 9) and of 1.33 prescriptions (SD 1.48, min. 0, max. 7) were given. The effect of visit duration is more pronounced in counselling (R2 0.24; p=0.000) than in prescription (R20.06;p=0.100).
There is great variability between paediatricians both in the mean number of recommendations given (CV 38.38%) as well as the mean number of prescriptions (CV 40.75%) (Fig. 3).
The paediatrician was more likely to explain a recommendation if it had been requested by the mother, although the difference was not statistically significant. The recommendation/prescription ratio is 3.47 when the mother takes the initiative and 1.94 when the initiative is from the paediatrician (Χ2 2.94; p=0.086).
On the other hand, the regression curves of Fig. 4 show that as the age of the child increases, prescription becomes more frequent (p=0.048) and counselling less so (p=0.015). The counselling-to-prescription ratio becomes inverted at around three and a half years of age. No other characteristic of the child or the mother is associated to the frequency of counselling or prescription recommendations.
DISCUSSION
In the observed well-child visits, paediatricians gave a considerable amount of recommendations. Only 6% of visits did not include recommendations. These data are in agreement with the observations of previous studies28,29. It is certainly a good thing that most recommendations are of the counselling as opposed to the prescription type. Accompanying the recommendations with explanations has several positive effects: it improves the understanding of their usefulness, results in increased compliance, raises the levels of satisfaction, and gives skills and confidence to women in their role as mothers2,20-24.
The fact that nearly a third of recommendations were sought by mothers, and that in these cases paediatricians gave more explanations as they answered, suggests that paediatricians adapt their discourse to the needs of mothers. In fact, giving parents the opportunity to express their doubts and concerns plays a crucial role in the efficiency and quality of children’s preventive care30,31. Having the opportunity to express doubts and to receive advice was independent from the educational level of the mother, which suggests that paediatricians are moving toward neutralising the effects of social inequality in their practices, which is a very positive aspect of their professional activity.
The duration of the visits, of 16 minutes, was within the recommended values18,28,32,33 and is positively and strongly associated to the amount of counselling, while having hardly any effect on prescriptions. This suggests that the duration of the visit is associated to its quality to a certain degree. In fact, some authors consider that the long list of actions and medical advice included in the well-child programme cannot be fulfilled in so few minutes8,31.
As children grow older, the frequency of prescriptions rises and the duration of the visit and the frequency of counselling decrease. This impoverishment of the contents of the programme has been observed in other studies9,12,14 and is probably related to the fact that the paediatric agenda is so heavily focused on biomedical aspects. Psychosocial aspects, the family relationship, and education, are areas that are addressed only sporadically when these issues grow in significance as the child grows. We believe that there is a clear opportunity for improvement here, as we know that problems in these areas are frequent and that families would like to get advice about them from their paediatricians8,16,19,35.
Medical training is very focused on the biological aspects of the health-disease process, and as a result the approach to communication with patients and families is almost exclusively based on the personal characteristics of paediatricians. The widespread view of the doctor-patient relationship as a technical area that can be subject to being learned and taught is a recent development21-25.
We found more heterogeneity than expected in a professional group with a shared technical and scientific background in the main variables that we studied: counselling, prescriptions, encouragement of maternal expression, and duration of visit. Although all paediatricians used counselling more than prescription, some seldom prescribe, that is, almost never give recommendations without explaining them, while others prescribe more often than they counsel.
The generalizability of the results of this study is limited due to the small sample size and non-random selection of paediatricians. Nevertheless, the sample of mothers served by each paediatrician can be considered representative of his or her clients. On the other hand, in a field in which most studies use questionnaires given to paediatricians or parents, the direct observation and recording of visits allowed us to study the actual content of the visits rather than the opinion of those involved in them, so we consider this a strength in our study.
Our data suggest that there are different paediatric practise styles whose characteristics and effects must be researched to set the foundations for training strategies in paediatrics adapted to professional practise in a primary care setting.
CONFLICT OF INTERESTS<
The authors declare having no conflict of interests in relation to the preparation and publication of this paper.
ABREVIATIONS: CV: coefficient of variation • SD: standard deviation • F: ANOVA • M: mean • max.: maximum • min.: minimum • r: Pearson’s coefficient • R2: linear regression • Χ2: chi-square.
BIBLIOGRAPHY
- Berkule-Silberman SB, Dreyer BR, Huberman HS, Klass PE, Mendelsohn AL. Sources of parenting information in low SES mothers. Clin Pediatr. 2010;49:560-8.
- Nunes C, Ayala A. ¿Qué piensan las madres sobre el programa de seguimiento de la salud infantil? Rev Pediatr Aten Primaria. 2007;9(35):411-25.
- Hidalgo MV, Menéndez S, López I, Sánchez J. Nacer a la vida: un programa de apoyo y formación durante la transición a la maternidad y la paternidad. Infancia y Aprendizaje. 2004;27:407-15.
- Young K, Davis K, Schoen C, Parker S. Listening to parents: a national survey of parents with young children. Arch Pediatr Adolesc Med. 1998;152:255-62.
- Schuster MA, Duan N, Regalado M, Klein DJ. Anticipatory guidance: what information do parents receive? What information do they want? Arch Pediatr Adolesc Med. 2000;154:1191-8.
- Cheng T, Savageau J, Bigelow C, Charney E, Kumar S, DeWitt T. Assessing mothers’ attitudes about the physician’s role in child health promotion. Am J Public Health. 1996;86:1809-12.
- Dirección General de Atención Primaria y Promoción de la Salud. Guía para la salud infantil. Sevilla: Junta de Andalucía e Consejería de Salud; 1990.
- Schor EL. Rethinking well-child care. Pediatrics. 2004;114:210-6.
- Nunes C. Pediatricians’ ideas about child development and education. Psicologia: Reflexão e Crítica. 2011;24(2):765-72.
- Cheng TL, DeWitt TG, Savageau JA, O’Connor KG. Determinants of counseling in primary care pediatric practice. Physicians attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999;153:629-35.
- Nunes C, Ayala M. ¿De qué hablan los pediatras y las madres en la consulta de seguimiento de la salud infantil? An Pediatr (Barc). 2011;75(4):239-46.
- Olson LM, Inkelas M, Halfon N, Schuster MA, O’Connor KG, Mistry R. Overview of the content of health supervision for young children: reports from parents and pediatricians. Pediatrics. 2004;113:1907-16.
- Wissow LS, Larson S, Anderson J, Hadjiisky E. Pediatric residents’ responses that discourage discussion of psychosocial problems in primary care. Pediatrics. 2005;115:1569-78.
- Bethell C, Reuland CH, Halfon N, Schor EL. Measuring the quality of preventive and developmental services for young children: national estimates and patterns of clinicians’ performance. Pediatrics. 2004;113:1973-83.
- Almeida PVB, Zanolli ML. O papel do pediatra no PSF-Paidéia de Campinas (SP). Cien Saude Colet. 2011;16(Supl. 1):1479-88.
- Tanner L, Stein MT, Olson LM, Radecki L, Frintner MP. Reflections on well-child care practice: a national study of pediatric clinicians. Pediatrics. 2009;124:849-57.
- American Academy of Pediatrics. The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Pediatrics. 2001;108:1227-30.
- Galuska DA, Fulton JE, Powell KE, Burgeson CR, Pratt M, Elster A, et al. Pediatrician counseling about preventive health topics: results from the Physicians’ Practices Survey, 1998-1999. Pediatrics. 2002;109:E83-3.
- Radecki L, Olson LM, Frintner MP, Tanner JL, Stein MT. What do families want from well-child care? Including parents in the rethinking discussion. Pediatrics. 2009;124:858-65.
- Hart CN, Kelleher KJ, Drotar D, Scholle SH. Parent-provider communication and parental satisfaction with care of children with psychosocial problems. Patient Educ Couns. 2007;68:179-85.
- Nunes C, Ayala A. Communication techniques used by pediatricians in the well-child program visits: A pilot study. Patient Educ Couns. 2010;78:79-84.
- Ammentorp J, Sabroe S, Kofoed P, Mainz J. The effect of training in communication skills on medical doctors’ and nurses’ self-efficacy. A randomized controlled trial. Patient Educ Couns. 2007;66:270-7.
- Worchel FF, Prevatt BC, Miner J, Allen M, Wagner L, Nation P. Pediatrician’s communication style: relationship to parent’s perceptions and behaviors. J Pediatr Psychol. 1995;20:633-44.
- Nobile C, Drotar D. Research on the quality of parent-provider communication in pediatric care: Implications and recommendations. J Dev Behav Pediatr. 2003;24(4):279-90.
- Clayman ML, Wissow LS. Pediatric residents’ response to ambiguous words about child discipline and behaviour. Patient Educ Couns. 2004;55:16-21.
- Baker LH, O’Connell D, Platt FW. What else? Setting the agenda for the clinical interview. Ann Intern Med. 2005;143:766-70.
- Borrell F. Manual de entrevista clínica. Barcelona: Doyma; 1988.
- Goldstein E, Dworkin PH, Bernstein B. Time devoted to anticipatory guidance during child health supervision visits: how are we doing? Amb Child Health. 1999;5:113-20.
- Manning KM, Ariza AJ, Massimino TK, Binns HJ. Health supervision visits of very young children: Time addressing 3 key topics. Clin Pediatr. 2009;48:931-8.
- Glascoe FP. Evidence-based approach to developmental and behavioural surveillance using parents' concerns. Child Care Health Dev. 2000;26:137-49.
- Sand N, Silverstein M, Glascoe FP, Gupta VB, Tonniges TP, O’Connor KG. Pediatricians’ reported practices regarding developmental screening: Do guidelines work? Do they help? Pediatrics. 2005;116(1):174-9.
- Cox ED, Smith MA, Brown RL, Fitzpatrick MA. Effect of gender and visit length on participation in pediatric visits. Patient Educ Couns. 2007;65:320-8.
- Halfon N, Inkelas M, Mistry R, Olson LM. Satisfaction with health care for young children. Pediatrics. 2004;113:1965-72.
- Yarnall KSH, Pollak KI, Østbye T, Krause KM, Michener JL. Primary Care: Is there enough time for prevention? Am J Public Health. 2003;93(4):635-41.
- Combs-Orme T, Nixon BH, Herrod HG. Anticipatory guidance and early child development: Pediatrician advice, parent behaviors, and unmet needs as reported by parents from different backgrounds. Clin Pediatr. 2011;50:729-37.






