Vol. 14 - Num. 54
Original Papers
Analysis of the theoretical knowledge and clinical management of fever by paediatricians and medical residents in relation to an established care protocol
José Manuel García Pugaa, Francisco Javier Garrido Torrecillasb, MD Hernández Morillasc, L Castillo Díazc, JL Santos Pérezd, José Emilio Callejas Pozoe, Eduardo Ortega Páezf, T Jiménez Romerog, M Expósito Ruizh, A Ruiz Extremerai
aPediatra. CS Salvador Caballero. Granada. España.
bPediatra. EBAP-UCG Churriana de la Vega. Granada. España.
cPeditra. Unidad de Gestión Clínica de La Zubia. Granada. España.
dPeditra. Servicio de Pediatría. Hospital Universitario Virgen de las Nieves. Granada. España.
ePediatra. CS La Zubia. Distrito Granada-Metropolitano. Granada. España.
fPediatra. CS Maracena. Distrito Granada-Metropolitano. Granada. España.
gPeditra. Unidad de Gestión Clínica Salvador Caballero. Granada. España.
hTécnica de Apoyo a la Investigación de la Unidad de Investigación del Hospital Virgen de las Nieves. Granada. España.
iUnidad de Cuidados Intensivos Neonatales. Hospital Clínico San Cecilio. Granada. España.
Correspondence: JM García. E-mail: jmgpuga@telefonica.net
Reference of this article: García Puga JM, Garrido Torrecillas FJ, Hernández Morillas MD, Castillo Díaz L, Santos Pérez JL, Callejas Pozo JE, et al. Analysis of the theoretical knowledge and clinical management of fever by paediatricians and medical residents in relation to an established care protocol. Rev Pediatr Aten Primaria. 2012;14:115-26.
Published in Internet: 06-07-2012 - Visits: 34887
Abstract
Objective: to evaluate the recommendations given to parents by providers in regards to fever, and learn the estimated incidence of fever without source (FWS) in healthcare visits, the accessibility of complementary tests (CT) and the implementation of a fever protocol (FP).
Methods: questionnaire surveying a total of 151 primary care paediatricians (PCP), hospital paediatricians (HP) and paediatric residents (R). The statistical software package SPSS® 15.0 was used. For qualitative variables, we used the chi-square test, with a p-value of p < 0.05.
Results: we analysed the data from 109 questionnaires: 65.4% of respondents were female and 34.6% males. 44.9% defined fever as an axillary temperature of at least 37.5 °C and a rectal temperature of 38 °C and up. 78.9% recommend using the digital thermometer; 93.6% recommend physical measures; 79.8% paracetamol; and 76.1% alternating antipyretics in specific cases. 56.2% diagnose 10% of their weekly patients with FWS, 19.3% always codify it in the chart; 31.2% codify only sometimes, and 45.9% never do. For children younger than six months, 91.7% request a urine strip test, and 41.3% a urine culture; for patients ages 6 to12 months, 96.3% request a urine strip test and 11.9% a urine culture. Among PCP, only 3% receive the results of complete blood counts, and 68.6% the requested x-rays, within the day. 38.7% of PCP get the results of urine cultures within 72 hours. HP and R receive the following test results within the day: complete blood count (88.3%) and x-rays (85.7%); 85.7% of them receive the results of urine cultures within 72 hours. 74.6% of PCP refer children younger than 3 months for hospitalisation, 64.7% of HP and 83.3% of R request CT. 78.9% of respondents are aware of the FP, of which 69.8% believe that it applies to daily clinical practice, and 65.4% actually implement it.
Conclusions: most providers recommended the use of the digital thermometer, physical measures, and paracetamol. They recommended alternating for specific cases. FWS is underdiagnosed and codified infrequently in medical charts. PCP have limited access to complementary tests. The FP was known widely but its implementation rate was low.
Keywords
● Child ● Fever ● Fever without source ● Internship and Residency ● QuestionnairesINTRODUCTION
Normal body temperature is variable in healthy individuals and follows a circadian rhythm that is maintained during disease.
Fever is defined as a rise in temperature above the normal daily range. In general, it is a mechanism triggered by the body in response to a potential attack, and in children it is usually due to infection; however, since the same physiopathological processes can be the result of a wide variety of aetiologies, fever is a completely non-specific symptom1.
Measuring devices are used to determine body temperature. The most widely used thermometer used to be the mercury thermometer. Since the European Union2 banned the use of mercury in clinical devices in 2006, the use of other types has become widespread.
When it comes to where to take the temperature, it is known that the value of the temperature will vary depending on the body site where it is measured. The underarm is an easy-to-access site, but provides less accurate measurements except in children younger than one month of age3,4. Broadly speaking, the values considered normal in children range between 35.6 and 38.2 °C. Body temperatures above the 99th percentile (> 37.7 °C) can be considered fever; however, there is no universally accepted definition5.
Fever is a very frequent reason for healthcare visits, since it is very common in young children and causes great concern and uncertainty. Finding its source can be complicated, a difficulty compounded at times by assistance being sought very early on (short evolution time). Different circumstances contribute to this difficulty: lack of knowledge, inaccurate beliefs, the crowding of healthcare services, and the disparities in its management and treatment, all of which contribute to a situation that has been labelled “fever phobia”6,7 referring to the “panic” that fever causes in its environment.
Like many other clinical profiles, fever shows great variability and different clinical expressions, which is further complicated by the fact that in infants and young children the presentation may be very similar for just an ordinary infection or a potentially serious infection, when the prognosis is completely different8.
Fever without source (FWS)9, is relatively frequent, since no source for the fever is found in 20% of the children attending healthcare services with it10-12. A good portion of FWS cases resolve spontaneously13, although as it evolves there is always the possibility that it may be due to occult bacteraemia or potentially severe bacterial infections14. The introduction of new vaccines15 and the recommendation of others by scientific associations16,17 has resulted in a decrease of the incidence of occult bacteraemia and sepsis from 3-5% in children 3-6 months of age and 10% in children younger than 3 months18,19 to figures below 1%20,21. These changes signal intervention strategies that will change current protocols.
At present, the development of better evidence-based guidelines is being promoted for the purpose of reducing the variability of clinical practices. Their implementation is expected to be advantageous to both patient and physician. There are guidelines and protocols4,10 that are meant to become an important tool in the correct treatment of children who present with FWS, but they are not always followed. Such guidelines are often unwelcome or ignored, although their implementation is being introduced gradually in healthcare practises 22-24.
In Andalusia, there are working tools known as “integrated healthcare protocols”, one of which is the one for what they term “fever syndrome” in children25. Although this protocol has been around for seven years, there is no documentation regarding the extent to which providers know or implement it.
The objectives of our study were to evaluate what is considered as fever and what recommendations are made to caregivers by primary care paediatricians (PCP), hospital paediatricians (HP) and paediatric residents (R), to learn the estimated incidence of FWS in their practices, the accessibility of complementary tests from their practices, and the knowledge and implementation of the childhood fever syndrome protocol (FP).
MATERIALS AND METHODS
The study was based on 109 questionnaires, answered by 68 (65.4%) women and 36 (34.6%) men, whose distribution by occupation was: 67 (61.5%) PCP, 43 (64.2%) female and 24 (35.8%) male; 18 (16.5%) HP, 9 (52.9%) female and 8 (47.1%) male; and 24 (22%) paediatric R, 16 (80%) female and (20%) male. The surveyed HP are physicians who provide emergency room care as part of their regular duties.
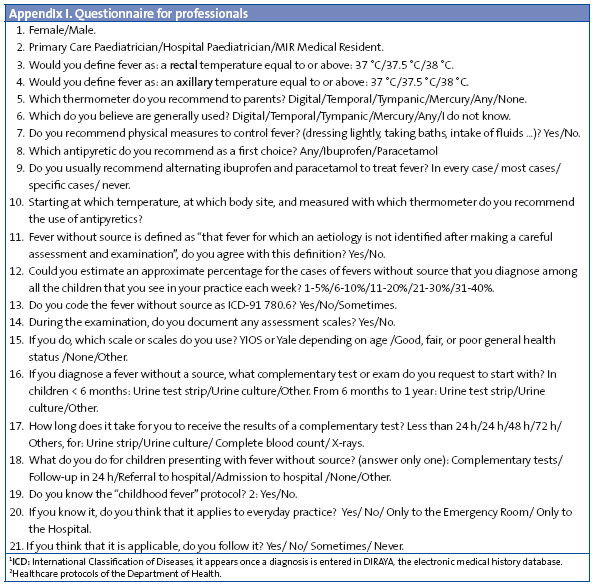
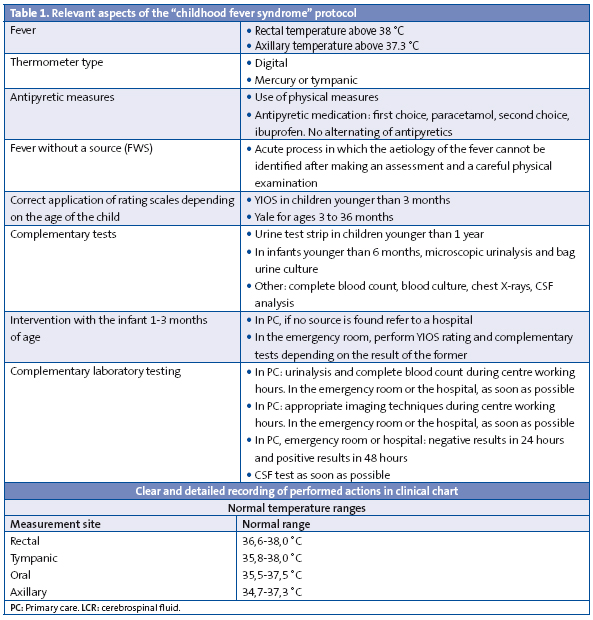
The participants were given a survey of 17 questions (Appendix I), in which the dependent variables were the recommendations, documentation and activities performed by providers in relation to FWS, with the sex and professional category of the participant as the independent variables. Table 1 summarises the most relevant aspects of the FP and the temperature ranges considered normal.
The questionnaire was sent by mail to every single PCP in two healthcare districts, and the answers were received by the same medium. It was also distributed to the HP and R of the two reference hospitals, and in both cases the responses were collected in person. The survey was carried out between May and September 2009.
Sample size calculation
Starting with the total population of providers in the included centres, 151, and assuming that the proportion knowledgeable of the protocol would be around 73%, to make a ratio estimation for the finite population with a 95% confidence interval, the resulting sample size was 101; in the end, 109 subjects were surveyed. The obtained sample was stratified in proportion to the number of professionals in each category.
Statistical data analysis
We started by doing a descriptive analysis of the cases, calculating averages and standard deviations for quantitative variables and absolute and relative frequencies for qualitative ones. Descriptive statistics were done for the entire sample and for each professional category. Later on, we analysed potential differences in answering the questions of the survey as a function of sex and professional category. To study the relationship between qualitative variables, we applied the chi square test, correcting for continuity in 2x2 tables. For numerical and quantitative variables we applied Student’s t-test or analysis of variance (ANOVA). The critical p-value was set to p < 0.05. The analysis of data was done using the statistical software package SPSS® 15.0.
Ethical considerations
The study protocol was approved by the Committee for Clinical Ethics and Research of the healthcare districts involved, which participated in the definition and design of the study, the analysis and interpretation of data, and the drafting and editing of the text. There is no prior agreement with the companies whose products are mentioned in this work. There is no conflict of interest in relation to this project. This work was not funded by any subsidies or grants.
RESULTS
Knowledge of what is considered as fever and recommendations given to caregivers by PCP, HP and R
Some of the answers to the required questions about the definition of fever, thermometer use, recommendations of antipyretic measures, and their frequency are summarised in Table 2.
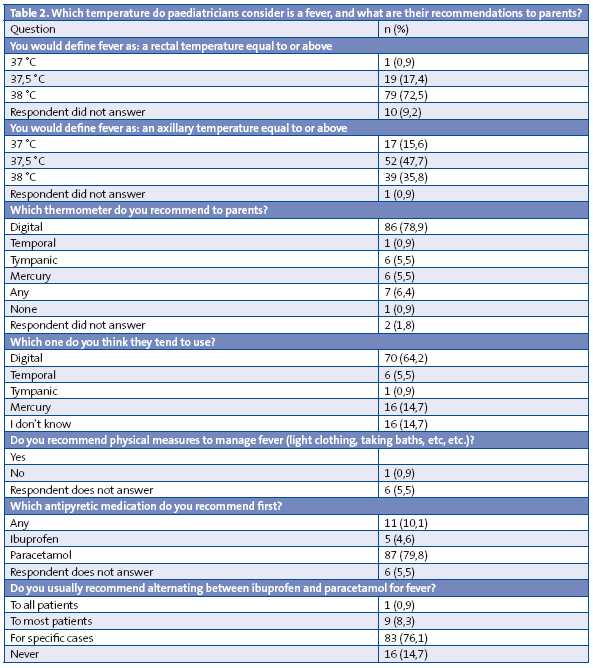
Most of the surveyed providers had adequate knowledge of the rectal and axillary temperatures that are considered to be fevers, although 39 of them (35.8%) consider that an axillary temperature of 38 °C in the patient constitutes a fever.
The correct definition of 37.5 °C axillary temperature and 38 °C rectal temperature was chosen by 49 of the surveyed participants (44.9%): 29 female (42.6%) and 17 (47.2%) male, with no statistically significant differences found between providers of different sexes or job titles.
The recommendation of thermometer type and antipyretic measures adhered to what was indicated in the FP.
A single site is recommended for the purposes of taking the temperature by 62 of the respondents (56.9%), out of which 32 are PCP (47.8%), 9 HP (50%) and 21 R (87.5%), while 37 (33.9%) recommend two sites, of which 31 are PCP (46.3%), 4 HP (22.2%) and 2 R (8.3%); there are statistically significant differences between the different professionals (p < 0.05).
Starting treatment with antipyretics when there is an axillary temperature of 38 °C or higher was recommended by 67.8% of PCP, 66.7% of HP and 91.7% of R, and most HP (83.4%) and R (91.7%) did not answer in regards to the rectal temperature. A higher proportion of PCP answer this question (50.7%), and are divided between those who administer antipyretics starting at 38 °C (52.9%) and those who start at 38.5 °C (38.2%). When it comes to the recommendations for treatment with antipyretics depending on the temperature, the site where the temperature is to be measured and the type of thermometer to be used, there are no significant differences between sex groups or professional groups.
Incidence of the FWS diagnosis
A hundred respondents (91.7%) agree with the definition of FWS given in the questionnaire.
When it comes to estimating the number of FWS diagnoses in comparison to other diagnoses, 32 respondents (33.3%) estimate that they amount to 5% of the diagnoses, 22 (22.9%) that they are between 6 and 10%, 16 (16.7%) between 11 and 20%, 20 (20.8%), between 21 and 30%, and 6 (6.2%) make estimates over 30%. Thirteen respondents (11.9%) did not answer this question.
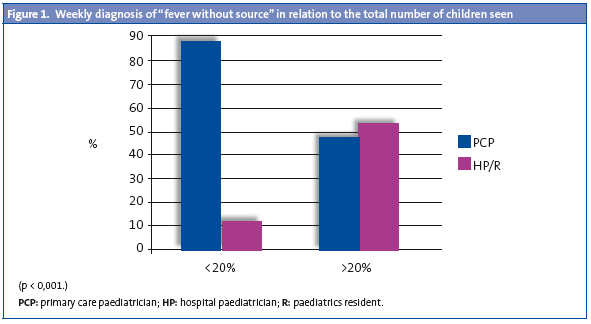
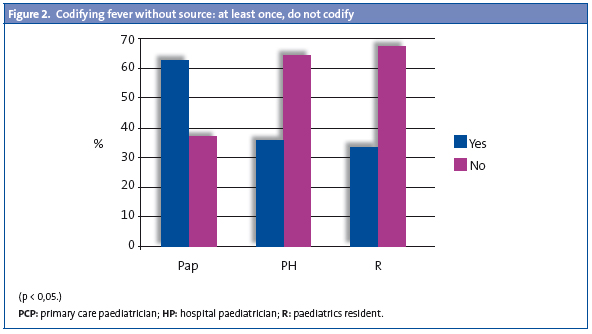
There were no statistically significant differences between both sexes, but there were between professional categories (Fig. 1): HP and R diagnose FWS more frequently than PCP, and the difference is statistically significant (p < 0.001). When asked whether they codify FWS according to the ICD-9, 21 (19.3%) answer yes, 34 (31.2%) sometimes, and 50 (45.9%) never; there are no statistically significant differences based on sex, but there are among professional categories (Fig. 2), with HP and R codifying it least frequently.
Documentation of the clinical examination and accessibility of complementary tests
Out of all the respondents, 106 (97.2%) report documenting the assessment of fever in the clinical chart, with 67 of them (61.5%) using the Young Infant Observation Scale (YIOS) or the Yale Observation Scale, of which 30 are PCP (44.8%), 14 HP (77.8%) and 23 R (95.8%). HP and R use these scales more than PCP, a difference that is statistically significant (p < 0.001). Also, 59 respondents (54.1%) reported using the traditional rating scale (good, fair, and poor general health status), out of which 48 are PCP (71.6%), 6 HP (33.3%), and 5 R (20.8%); the PCP use it more often than the HP and the R and the difference is statistically significant (p < 0.001).
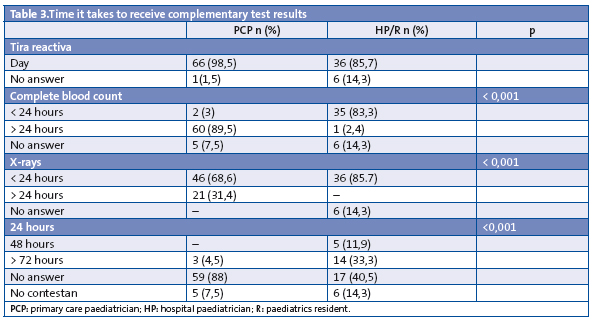
The availability of complementary tests (CT) to the different providers in terms of the time it takes to get the results back is shown in Table 3, which all of them can get immediately.
Knowledge and application of the “childhood fever syndrome” protocol
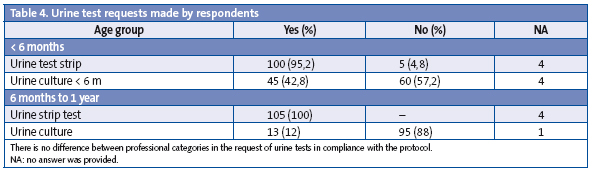
The CT requested for children younger than six months out of the urine tests available for the first year of life were:
- Urine test strip: requested by 100 (95.2%) of the participants, out of which 60 are PCP (89.5%), 16 HP (88.9%), and 24 R.
- Urine culture: requested by 45 (42.8%) of the respondents, of which 28 are PCP (41.8%), 9 HP (50%) and 8 R (33.3%).
The requested tests for the 6 to 12 month age group are:
- Urine test strip: requested by 105 (100%) of the respondents, of which 66 are PCP (98.5%), 16 HP (88.9%) and 23 R (95.8%).
- Urine culture: requested by 13 (12%) of which 4 are PCP (22.2%), 1 HP (4.2%) and 8 R (11.9%).
There are no statistically significant differences between professional categories for the tests noted above (Table 4).
In addition to urine tests, 14 of the respondents (12.8%) request other CT: 6 women and 8 men, of which 9 are PCP (13.4%), 2 HP (11.1%) and 3 R (12.5%). These tests are: complete blood count (4), blood chemistry test (2), blood culture (1), x-rays (Rx) (2) and clinical x-rays (1), serology (1), unspecified (2) and depending on the general health status of the child (1).
In the opinion of 50 PCP (74.7%), the adequate intervention for an infant 1 to 3 months of age presenting with FWS would be referral to the hospital, and 12 of these PCP (17.9%) would either do CT or follow up 24 hours later; four (6%) would not take any of the suggested actions, and one (1.5%) did not answer this; 11 HP (64.7%) and 20 R (83.3%) would request CT, one HP (5.5%) would follow up within 24 hours, and six HP (33.3%) and four R (16.7%) would admit the child to the hospital. One HP did not answer.
Eighty-six of the respondents (78.9%) know the FP, of which 52 are PCP (77.6%), 16 HP (88.9%) and 18 R (75%). There were no statistically significant differences between different sexes or types of provider.
Out of the 86 respondents (78.9% of the total) who know the FP, 77 (89.5%) believe that it is applicable to clinical practice to various extents; thus, 60 (77.9%) believe that it applies to all clinical practice, 14 (18.2%) that it only applies to the emergency room, and 3 (3.9%) that it applies only to the hospital; 9 respondents (10.6%) believed that it did not apply at all. There are no statistically significant differences based on sex or professional category.
Of the 60 that believe that the protocol is applicable, 37 (61.7%) implement it without exception, 19 (31.7%) sometimes, and 2 (3.3%) never do. Two of the respondents did not answer. There are no significant differences between sexes or professional categories.
DISCUSSION
This work has evaluated the various responses of paediatricians in both healthcare environments (primary care and hospital care) and also of paediatric residents R, working in two healthcare districts, and has used the FP as a basis for comparison.
There is a higher degree of agreement on the definition of fever based on the rectal temperature (72.5%) than on the axillary temperature (47.7%), if we put together the data of respondents choosing both temperatures, 37.5 °C in the underarm and 38 °C in the rectum, the percentage of those answers is close to those that pick an axillary temperature of 37.5 °C (44.9%). There is ample agreement in regard to recommending the use of the digital thermometer (79.8%), and when it comes to the recommended site for measuring body temperature, PCP indicate more than one, although most of them recommend the underarm, in contrast to HP and R, who recommend a single site, the underarm.
Despite the controversy that they cause and the scant evidence supporting their effectiveness, physical measures26-28 are recommended by a vast majority of respondents (93.6%), and in terms of the use of antipyretics, they recommend paracetamol first (78.9%) in both in agreement with the FP25, a fact that does not fit marketing statistics or published research, which document an equal or even higher consumption of ibuprofen26,27,29,30.
The answer choice marked most frequently and by a high percentage of providers is the recommendation of alternating antipyretics in specific cases (76.1%) even though this is a contested practise27,30,31, one, however, that appears to be widespread; in fact, our data seem to confirm this fact.
When it comes to recommending antipyretics depending on the temperature, there is a disparity in the use of these medications, and prescription starts at an axillary temperature of 38 °C; the PCP who recommend two temperature-taking sites prescribe antypiretic medication at an axillary temperature of 38 °C and a rectal temperature of 38.5 °C. Only three respondents state that the general health status of the child is a criterion in the prescription of antipyretics.
The points we have presented this far (definition of fever, recommendations) are particularly important, since they reflect the information conveyed to parents.
There is widespread agreement with the stated definition for FWS (91.7%), yet there is a great variability when it comes to diagnosing it. HP and R diagnose more FWS cases on a weekly basis than PCP. At any rate, it would be difficult to get to know the actual number of diagnoses, since only 19.3% codify it, sometimes up to 31.2%, with PCP codifying it most frequently.
There is frequent documentation of assessments (97.2%) and the level of use of rating scales is acceptable (61.5%), although the PCP use the YIOS or Yale scales less often than the traditional one (71.6%), the use of each of the scales depending on the child’s age is low (23.5%).
The use of CT on top of the clinical history and examination is fundamental for making decisions regarding FWS. The accessibility of these examinations poses a clear hurdle to the implementation of the FP, since with the exception of the urine test strip, PC have limited access to the CT. For tests that may be decisive in making a diagnosis, only 3% of PCP receives complete blood count results within the day, and only 4.5% report getting the urine culture in 48 hours, 31.4% of PCP do not even get a simple Rx within the day.
A considerable majority of providers know the FP, since 78.9% of the respondents answered in the affirmative. This fact is at odds with the implementation of the protocol if we take into account the answers to some of the other questions, for instance, 49 (44.9%) of those reporting knowledge of the protocol give a correct definition of fever. As for the CT, we evaluated requests for the earliest and most accessible tests by the three types of providers involved in the study, as is the case of urine tests: the urine culture is requested more often in children younger than six months, but only about 42.8% do so (it should be 100%), and this rate drops for children between 6 and 12 months of age (12%), with the urine test strip being used more often in this age group, a test that is more appropriate and that is less useful in children younger than six months, although it is used in the latter age group (95.2%) almost as often as in children 6-12 months old (100%). The request for other important CT in the FP, such as the complete blood count, is quite infrequent, as only 12.5% would request any of these other tests. The wording of the question may bias respondents toward reporting requests for urine tests rather than any other CT, although the latter option is also available as an answer. Still, it could also be argued that in addition to the child’s age, the information gathered from the clinical examination should be considered.
The response to infants 1-3 months of age depends on what is available and also tends to adhere to the FP; in fact, HP and R apply the protocol differently as would be expected from the broader resources available in the hospital or the emergency room compared to primary care settings, which poses limitations when it comes to its application in the latter setting (lower availability); thus, it could be hard to manage a presenting fever without CT and based only on the clinical evaluation without incurring in serious risks, which would account for the different attitudes of the PCP, who would tend to refer to the hospital, and of the HP and R, who would request CT.
In addition to the obstacles to the implementation of the protocol noted above, 10.6% of the respondents who know it do not believe that it applies to clinical practise, regardless of the healthcare setting, and among those who believe it is applicable, only 37 of them (61%) implement it every time, which would come down to 43.1% of those aware of it and it would be an even smaller proportion of the total (33.9%), which would be a very low rate of implementation for a protocol designed to improve clinical practise and reduce its variability.
Conclusions
There seems to be little agreement when it comes to providing a definition of fever to caregivers, as well as in implementing the protocol, although there is general agreement on the recommendations regarding thermometers and the treatment of the fever, both physical and pharmacological. There is wide variability in the estimated frequency of FWS diagnoses between providers, with higher estimates among those working in a hospital setting. PC providers have very low access to complementary tests, which does not facilitate the implementation of the protocol. Although the protocol is widely known, its implementation is infrequent.
CONFLICTS OF INTEREST
One author (MER) is employed with funding provided by the Instituto Carlos III. Part of this manuscript was presented orally during the 59 National Congress of the Spanish Association of Pediatrics in Maspalomas (Gran Canaria) in June 2010.
ACRONYMS: PC: primary care • CT: complementary tests • FWS: fever without source • PCP: Primary care paediatrician • FP: childhood fever syndrome protocol • HP: hospital paediatrician • R: paediatrics resident • Rx: x-ray • YIOS: Young Infant Observation Scale.
BIBLIOGRAFY
- Fiebre. Guías Clínicas [en línea] [consultado en 06/2009]. Disponible en www.fisterra.com/guias2/fiebre.asp
- Comunicación de la Comisión al Consejo y al Parlamento Europeo. Estrategia comunitaria sobre el mercurio, Bruselas 28.01.2005. COM (2005) 20 final [en línea] [consultado en 06/2009]. Disponible en http://europa.eu/legislation_summaries/internal_market/single_market_for_goods/chemical_products/l28155_es.htm
- Community Paediatrics Committee. Canadian Paediatrics Society. Temperature measurement in paediatrics. Reaffirmed in February 2009 [en línea] [consultado en 06/2009]. Disponible en www.cps.ca/ENGLISH/statements/CP/cp00-01.htm
- Fever illness in children. Assessment and initial management in children younger than 5 years. National Collaborative Centre for Women’s and Children’s Health, 2007 [en línea] [consultado en 06/2009]. Disponible en http://publications.nice.org.uk/feverish-illness-in-children-cg47
- Khalert CH, Nadal D. Acute fever in infants. Ther USMC. 2006;63(10):659-65.
- Bauer Izquierdo S, Díez Domínguez H, Ballester R, Ballester A. Persistencia de la fiebrefobia a pesar de la evidencia científica. Acta Pediatr Esp. 2009;67:578.
- Crocetti M, Moghbeli N, Serwint J. Fever phobia revisited: have parental misconceptions about fever changed in 20 years? Pediatrics. 2001;107:1241-6.
- Daaleman TP. Fever without source in infants and young children. Am Fam Physician. 1996;54:2503-12.
- Rodrigo Gonzalo-de-Liria C, Méndez Hernández M. Fiebre sin foco. AEP [en línea] [consultado en 08/2010]. Disponible en http://www.aeped.es/sites/default/files/documentos/fiebresinfoco.pdf
- Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med. 2000;36(6):602-14.
- Mintegi Raso S, Benito Fernández J, García González S, Corrales Fernández A, Bartolomé Albistegui JI, Trebolazabala Quirante N. Demanda y asistencia en un servicio de urgencias hospitalario. An Pediatr (Barc). 2004;61:156-61.
- Mintegi Raso S, Sánchez Echaniz J, Benito Fernández J, Vázquez Ronco MA, García Ribes A, Trebolazabala Quirante N. Utilización nocturna de una unidad de urgencias pediátrica hospitalaria. An Esp Pediatr. 2000;52:346-50.
- Alpern ER, Alessandrini EA, Bell LM, Shaw KN, McGowan KL. Occult bacteraemia from a paediatric emergency department: current prevalence, time to detection, and outcome. Paediatrics. 2000;106:505-11.
- Sur DK, Bukont EL. Evaluating fever of unidentifiable source in young children. Am Fam Physician. 2007;75:1805-11.
- Vacunas. El calendario Infantil. 40 años de cambios, 1962-2006. Sevilla: Consejería de Salud; 2006.
- Committee on Infectious Diseases. American Academy of Pediatrics. Pediatrics. 2001;107:202-4.
- Comité Asesor de Vacunas de la Asociación Española de Pediatría. Calendario vacunal de la Asociación Española de Pediatría 2003. An Pediatr. 2003;58:257-62.
- Haddon RA, Barnett PL, Grimwood K, Hogg GG. Bacteraemia in febrile children presenting to a paediatric emergency department. Med J Aust. 1999;170(10):475-8.
- Kuppermann N. Occult bacteremia in young febrile children. Pediatr Clin North Am. 1999;46(6):1073-109.
- Wilkinson M, Bulloch B, Smith M. Prevalence of Occult Bacteremia in Children Aged 3 to 36 Months Presenting to the Emergency Department with Fever in the Postpneumococcal Conjugate Vaccine Era. Acad Emerg Med. 2009;16(3):220-5.
- Pratt A, Attia MW. Duration of fever and markers of serious bacterial infection in young febrile children. Pediatr Int. 2007;49(1):31-5.
- Massin MM, Montesanti J, Lepage P. Management of fever without source in young children presenting to an emergency room. Acta Paediatr. 2006;93:1446-50.
- Seow VK, Lin AC, Lin IY, Chen CC, Chen KC, Wang TL, et al. Comparing different patterns for managing febrile children in the ED between emergency and pediatric physicians: impact on patient outcome. Am J Emerg Med. 2007;25:1004-8.
- Madsen KA, Bennett JE, Downs SM. The role of parental preferences in the management of fever without source among 3-to 36-month-old children: a decision analysis. Pediatrics. 2006;117:1067-76.
- García Puga JM. Proceso Asistencial Integrado. Síndrome Febril en el Niño [en línea] [consultado el 06/2009]. Disponible en www.juntadeandalucia.es/salud/contenidos/procesos/docs/procesos_FIEBRE_NI%2525C3%252591O%255B1%255D.pdf
- Giachetto G. Conducta de los pediatras frente a la fiebre. Arch Pediatr Urug. 2001;72(2):116-20.
- Melamud A, Suwezda A, Matamoros R, Ringuelet L. Indicación de antitérmicos por médicos pediatras, Internet como modalidad de recolección de datos. Arch Argent Pediatr. 2008;106:404-8.
- Meremikwu M, Oyo-Ita A. Drugs and other methods for managing fever in children. Cochrane Database of Systematic Reviews 2000, Issue 3. Art. No: CD002241.
- Hay AD, Costeloe C, Redmond NM, Montgomery AA, Fletcher M, Hollinghurst S, et al. Paracetamol plus ibuprofen for the treatment of fever in children (PITCH): randomised controlled trial. BMJ. 2008;337:729-33.
- Erlewyn-Lajeneuse MDS, Coppens K, Hunt LP. Randomised controlled trial of combined paracetamol and ibuprofen for fever. Arch Dis Child. 2006;91:414-6.
- Mayoral CE, Marino RV, Rosenfeld W, Greensher J. Alternating antipyretics: is this an alternative? Pediatrics. 2000;105:1009-12.