Vol. 15 - Num. 57
Original Papers
Differences in the use of Primary Care services among native and immigrant children
Rosa M.ª Macipe Costaa, Luis Gimeno Feliua, Fernando Barrera Linaresb, Mónica Lasheras Barrioc, Angelique Charlotte Robertd, Lourdes Luzón Olivere
aPediatra. CS San Pablo. Zaragoza. España.
bMédico de familia. CS Cariñena. Zaragoza. España.
cMédico de familia. CS San Pablo. Zaragoza. España.
dMédico de familia. CS Albalate de Cinca. Huesca. España.
eMédico de familia. CS Hellín. Hellín. Albacete. España.
Correspondence: RM Macipe. E-mail: rmacipe@gmail.com
Reference of this article: Macipe Costa RM, Gimeno Feliu L, Barrera Linares F, Lasheras Barrio M, Robert AC, Luzón Oliver L. Differences in the use of Primary Care services among native and immigrant children. Rev Pediatr Aten Primaria. 2013;15:15-25.
Published in Internet: 05-12-2012 - Visits: 22532
Abstract
Introduction: the current study pretends: to analyze the use of Primary Health Care Services by the immigrant population under 15 years of age in comparison to the Spanish population of the same age group; and to analyze differences in the frequentation according to different origins of the immigrant population.
Material and methods: this is an observational retrospective study including all consultations of children under 15 years of age to 26 health centers in Zaragoza, Spain, during the year 2007. The main variable, frequentation, was defined as total number of visits/year. Secondary variables were the type of attention that was requested and region of origin of the. The information about the number and type of visits was obtained from the agenda in the electronic data base (“OMI©: oficina médica informatizada”) of the health centers. The frequentation was adjusted according to age and sex.
Results: A total of 547,524 pediatric appointments in a population of 71,114 children (of which 10.87% were immigrants) were analyzed. The adjusted annual frequency of visits in autochthonous children was 8.05 while this frequency was 5.66 in immigrant children. Among immigrant children, the highest annual frequentation (6.15) was seen among children from Sub-Saharan Africa and the lowest frequentation (4.02) was seen in children from Asia. This lower frequentation among immigrant children was seen in all types of attention (visits on request, programmed visits, emergency visits and home visits) and was independent of the opening hours of the different health centers (only morning or morning and afternoon).
Conclusions: the immigrant children’s population shows a lower use of the public primary health care than the autochthonous population of the same age group, independent of the region of origin.
Keywords
● Frequentation ● Immigrant children ● Pediatric Primary Care ● SpainNote:
Part of the data presented here were included in another publication: Gimeno-Feliu LA, Magallon-Botaya R, Macipe-Costa RM, Luzon-Oliver L, Canada-Millan JL, Lasheras-Barrio M. Differences in the Use of Primary Care Services Between Spanish National and Immigrant Patients. J Immigr Minor Health. 2012 May 22. [Epub ahead of print]. Available in: www.ncbi.nlm.nih.gov/pubmed/22618356
INTRODUCTION
In the past few years we have seen a profound transformation in Spanish society due to the substantial increase of the immigrant population, most of which comes from low-income countries1-6. Unlike what used to be the case a few decades ago, Spain could now be considered an immigration-receiving country7-12. According to the Instituto Nacional de Estadística (National Institute of Statistics, INE) (http://bit.ly/SJcW86), based on population registers (Padrón) from January 1 2010, the immigrant population in Spain comprises 12.17% of the total population. Immigrant children (0-14 years of age) comprise 11.92% of the children in our country. In Aragón, immigrants comprised 13.14% of the total population, and 13.38% of the paediatric population in 2008.
Unlike what has happened in the rest of Europe, the immigration phenomenon in Spain has been characterised by a very fast increase of the immigrant population, which has tripled in the past eight years (INE: http://bit.ly/SJdbQK). It is obvious that this increase of the immigrant population in such a short time requires that the receiving society makes efforts to adjust and reorganise certain areas. This phenomenon, which has obvious advantages for the receiving society, demands preparation on the part of the latter in many areas, including public health and healthcare services. Thus, it is of utmost interest to know the habits and needs of this segment of the population in order to allocate the resources and take the necessary steps to address them as best as possible2,5,11-19.
Meanwhile, this rapid increase has fostered the emergence of feelings of fear and rejection toward this population. In turn, these feelings have led to the generalised expression of views regarding the use that the immigrant population makes of the healthcare system, usually denouncing an excessive use of it on their part. Although these affirmations have no grounds in reality, they have gained a strong momentum and may influence our attitude towards the immigrant population. Therefore, it is important that we study these areas in detail, so we can put these notions to the test.
Along these lines, the Encuesta Nacional de Salud (National Healthcare Survey) took into account the “foreign” factor in 200615. This survey showed that the immigrant population uses healthcare services less than the native population (39.5% of the native population had used some type of healthcare service in the past few weeks, compared to 29.3% of foreigners)16. Furthermore, in the past few years other studies are confirming the falsehood of these assumptions, proving that the immigrant population uses the healthcare system less than the native population17-23.
To this day, the use of healthcare services by the immigrant population has been evaluated by means of surveys or sample studies21,23-27. Such studies are very useful but may have clear methodological limitations, such as selection biases, low response rates, and various response biases. Such limitations could be avoided by using insurance databases and electronic clinical history data available in Primary Care (PC). Two recent review studies have insisted on the need for this type of studies24,28.
The current study was designed with the objective of overcoming the methodological challenges mentioned above, which may distort the results when it comes to the actual use of PC services by the Spanish and the immigrant paediatric populations.
The objectives are: 1) to analyse the use of PC services, adjusting for age and sex, of the immigrant population younger than 15 years of age in relation to the equivalent Spanish population, and 2) to analyse the differences that exist in the frequency of use according to the geographical area of origin.
PATIENTS AND METHODS
This is an observational retrospective study of all the visits made by the paediatric population (age <15 years) throughout 2007 in 26 healthcare centres (HCC) of Zaragoza (Aragón, Spain).
The main variable, the frequency of the visits, was defined as the total number of HCC visits per year (with any type of professional). The secondary variable was the type of service that was sought (on demand, routine, emergency, or home visit). Since the frequency of the different types of visits may vary between centres that offer morning- or afternoon-only hours for on-demand visits, we also took this variable into account when we analysed the data.
The independent variable was nationality. For the purposes of this study, we defined an immigrant as a person whose nationality is not Spanish (a foreign national), regardless of economic status29.
The countries of origin of the immigrants were categorized into the following groups: Latin America (includes Central and South America), Eastern Europe (includes Romania, Bulgaria, and countries that did not join the European Union until 2007), Sub-Saharan Africa, North Africa, European Union/North America, and Asia.
The information contained in the records of all the patients entitled to healthcare services in the insurance database (tarjeta sanitaria, or healthcare card) of the Government of Aragón and the data pertaining the visits were obtained from the electronic clinical history records (OMI©) of the HCC involved in the study.
The privacy of patients was safeguarded at all times. To cross-reference the data of both registers we used the Código de Identificación Aragonés (Aragón ID code), which identifies all patients unequivocally and anonymously.
We calculated frequency rates adjusted for age and gender for the immigrant population and the native population. We also performed direct standardization, using the Spanish population as the reference population based on the January 1 2008 data from the Instituto Nacional de Estadística (www.ine.es), to avoid differences due to variations in population distribution. Since we were working with the data of the entire population, we did not need to perform statistical analysis tests.
RESULTS
We analysed a total of 547,524 paediatric visits (age 0-15 years) in a population of 71,114 children (10.87% of whom were immigrants).
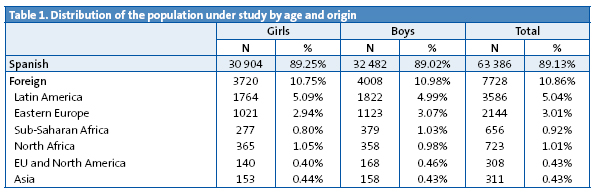
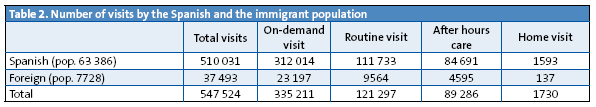
The distribution of the population under study by sex and origin is shown in Table 1. The total visits made for each type of healthcare service is shown in Table 2.
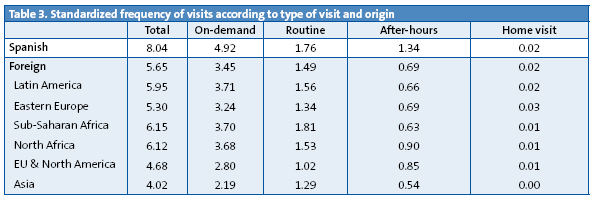
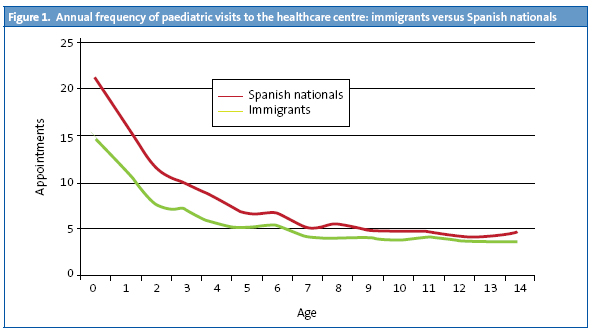
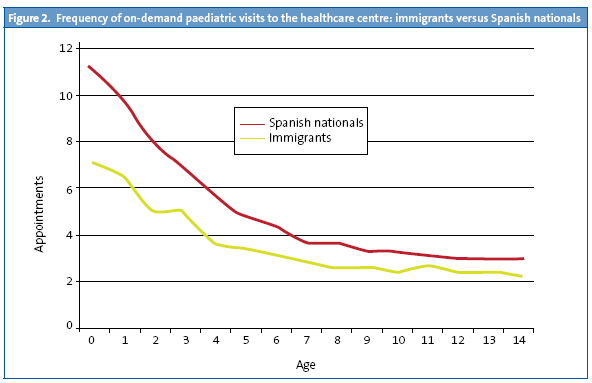
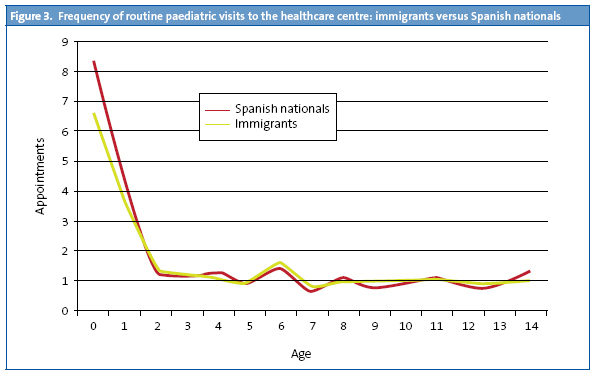
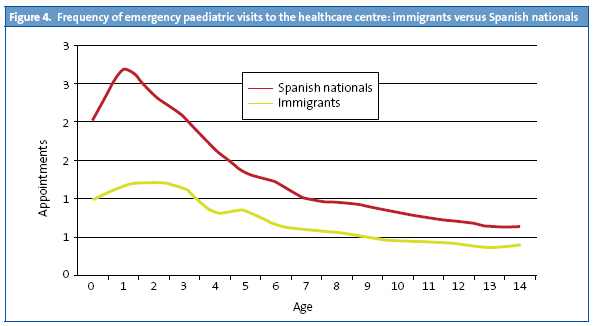
The adjusted annual frequency of visits in native children was 8.05, compared to 5.66 in immigrant children. If we analyse the frequency of visits by the origin of the immigrant children, we see that the rates are lower in all categories compared to the visit rates of Spanish children. The highest frequency of visits was seen in children from Sub-Saharan Africa (6.15), and the lowest in Asian children (4.02). The lower frequency of visits seen in immigrant children holds for every type of healthcare service. The standardized frequency of visits according to the type of visit and origin of the child is summarised in Table 3.
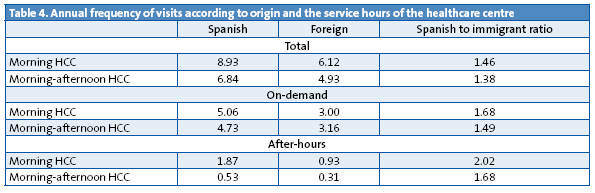
The accessibility of services can vary depending on whether the HCC are only open in the morning with after-hours care (AHC) in the afternoon, or open both in the morning and the afternoon. Spanish children use both types of centres more frequently, with the overall number of visits to morning services by Spanish children averaging 8.93, compared to 6.12 in foreign children, and 6.84 in Spanish children for morning and afternoon services, compared to 4.93 in foreign children. In the case of AHC, the frequency of use is higher in centres that offer morning hours only, however, the frequency of visits is higher in Spanish children than in foreign children both for the use of these services in centres with only morning hours and in centres with morning and afternoon hours. These data are summarised in Table 4.
The difference in the frequency of visits between Spanish and foreign children according to age, for the different types of healthcare services, is represented in Figs. 1-4.
DISCUSSION
The results of this study are conclusive: the immigrant population younger than 15 years of age uses PC services less than the native population. This was found to be true for all age intervals, and for every area of origin of the immigrant population.
The Spanish healthcare system is a universal system that, in accordance with the Organic Law 4/2000 of January 11, guarantees equal access to healthcare services to all immigrants younger than 18 years of age30. This characteristic of our healthcare system, which in principle does not pose legal or administrative barriers to minors for accessing healthcare, makes it particularly relevant to this type of study.
The availability to researchers of universal and trustworthy databases prevents the biases found in some of the preceding studies, and facilitates the assessment of the real and actual use of the public healthcare system by the entire population.
The results of this study agree with the results of similar studies on the use of hospital services31-33, consumption of pharmaceuticals18,20 and the use of PC services34 in Spain published before. The literature review done by Uiters24 found a lower rate of visits in the immigrant population, but showed wide variability between studies.
This evidence contradicts the widespread assumption that immigrant patients “overuse” healthcare services. When it comes to Spain, Esteva35 surveyed a sample of 159 primary care physicians, of which 81% agreed with the statement that “the immigrant patient comes for emergency visits more frequently than the rest of the covered population”. Our study shows that this perception is wrong, at least when it comes to the population under study.
It would be interesting to look further into the reasons why the immigrant population uses healthcare services less frequently than the native population. We could hypothesize that the native population overuses the healthcare system and that the immigrant population uses it more appropriately. A healthcare system like the one in Spain, which is universal, free, and characterised by easy access to PC visits, may carry the risk of being overused. In this regard, paediatricians believe that parents are making more consultations, and seeking them for increasingly mild pathologies, which would reflect an excessive dependency on the paediatrician and little autonomy in the management of conditions that often do not require medical attention36-38.
The other possibility is that the immigrant paediatric population underuses healthcare services, which could be due to a variety of reasons. In principle, as we commented above, there should be no barriers to access from a legal or administrative standpoint. However, other barriers to accessing healthcare have been described, such as language barriers, time barriers (due to worse and more precarious working conditions among the immigrant population), cultural barriers, a lack of understanding of the healthcare system, etc.39,40
If we were to take into consideration the presence of language barriers, we would expect that the frequency of visits of the immigrant population that came from Latin America would be similar to that of Spanish nationals. However, this is not what was seen in this study, since, as noted in Table 3, the standardised frequency of visits of the population from Latin America was 5.95, lower than that of immigrants from other regions, such as Sub-Saharan Africa (6.15), and North Africa (6.13) who face much greater communication challenges than the Latin American collective.
Another of the barriers that could exist would be associated with greater rates of precarious work, worse working conditions that would result in greater difficulty to come to the paediatrician’s office. This would entail a greater use of AHC appointments, and probably a lower rate of routine visits as well. Our study showed that the frequency of routine paediatric visits in native children is 1.76, compared to 1.49 in foreign children, a small difference that may support restricted access due to difficulties in coming to the doctor’s office for non-urgent conditions. Yet this hypothetical greater frequency of AHC visits was not confirmed, since these are also less frequent among immigrant patients (0.7 compared to 1.3).
We also saw that there was a higher use of AHC services in HCC that only had morning hours than in centres that had morning and afternoon hours, both by Spanish and immigrant children. Nevertheless, the frequency of visits was higher in Spanish children for both types of HCC. Our study did not show that the access barriers associated to fewer service hours and to the working conditions of the immigrant population resulted in a greater use of AHC services by this population.
This could lead us to conclude that immigrant children would use hospital emergency services more often than Spanish children. However, several studies on the frequency of the use of emergency hospital services by immigrants conclude that this rate is not higher than the one found among Spanish nationals31-33. Along these lines, a study of the frequency of use of paediatric emergency services in the Hospital Universitario Miguel Servet (the reference centre for many of the HCC under study, which receives most of the paediatric emergency cases in Zaragoza), shows that immigrant children use these services less frequently than native children19.
This study was based on the visits made in the public system, so a lower use of this system could also be due to a greater use of private healthcare services. However, it is likely that the immigrant population uses private healthcare services less frequently27, so the differences found in the frequency of healthcare use between the native and the immigrant populations could be even greater. In the case of children from Europe and North America, the low frequency of visits found could be due to a greater use of private healthcare services.
This lower frequency of use could also be due to immigrant children being healthier. This would contradict the hypothesis that associates a lower socio-economic status with a poorer general health status41. However, there are numerous studies that show that immigrants are generally healthier than the receiving populations, since healthier individuals are probably the ones who migrate42-48 (healthy migration effect) and migrant populations tend to have healthier lifestyles12,23,43. It seems unlikely that the differences in the health of adults due to this migration effect would influence the health of their children, most of who are born in Spain, except for genetic disorders.
Another explanation for the less frequent use of healthcare services could be based on the different conception and attitude toward health and illness of either collective. Health and illness are social constructs, and thus vary widely depending on the socio-cultural environment. This factor would be supported by the different frequencies of use associated to geographical origin found in this study, which shows some heterogeneity in the behaviour of immigrants. It is possible that in Spanish society there is a higher degree of medicalisation of mild conditions than in foreign populations. Furthermore, the native population may be more aware of prevention activities that many immigrants may not consider a priority, at least in the first few years spent in our country. This would lead to a lower frequency of routine visits, and fewer on-demand appointments, especially for the control of acute conditions.
Another factor that could be at play is the use of homemade remedies and traditional medicine approaches for mild conditions. This habit is often the result of barriers to healthcare access found in the countries of origin. Such “habits” can continue after arriving in Spain, especially during the first few years. As time passes, the immigrant may adjust and assimilate the culture of greater healthcare consumption found in our country. A few longitudinal studies would have to be done to confirm or reject the existence of such a trend. Studies involving the children of immigrants or the second generation would be very useful in this regard.
The main methodological strength of this study is that it analyses actual visits for the entire reference population (whether healthcare services were or not sought during the year under study), measuring the burden of both immigrants and Spanish nationals on the public healthcare system based on its actual use. Furthermore, as the demographic data of the patients were available, we could adjust for age and sex. This methodology contributes a completely objective and quantifiable perspective34. Studies based on surveys can have significant selection biases and less reliable data12,23,24,27,49.
Another strength is the sizeable amount of data gathered for the population under study, both for Spanish nationals and immigrants: 547,524 visits. This has allowed us to analyse the foreign population according to their different geographical origins.
Still, it would have been interesting if we had had additional data that would help assess some of the hypotheses under consideration, such as socio-economic status, number of years in Spain, data for the rural population, data regarding frequency of visits to private healthcare providers, etc. Any future studies delving into any of these aspects will be of interest.
CONCLUSIONS
The immigrant children population (regardless of geographic origin) makes less frequent use of PC services in the public healthcare system than the native population for every type of visit (on demand, routine, and after-hours). This less-frequent use may be due to an excessive use on the part of the Spanish population, an underuse on the part of the immigrant population, or both.
More studies are needed to assess whether this frequency of visits holds over time and to analyse other factors, such as the length of stay in the country, morbidity, socio-economic status, etc. which may have an influence of the results. Also, it would be advisable that qualitative studies are performed in order to identify additional factors that influence the use of the healthcare system.
CONFLICT OF INTERESTS
The authors declare that they had no conflict of interests when it came to preparing and publishing this paper.
ACRONYMS: AHC: after-hours care • PC: Primary Care • HCC: healthcare centre • INE: Instituto Nacional de Estadística.
BIBLIOGRAPHY
- Berra S, Elorza-Ricart JM, Bartomeu N, Hausmann S, Serra-Sutton V, Rajmil L. Necesidades en salud y utilización de los servicios sanitarios en la población inmigrante en Cataluña. Revisión exhaustiva de la literatura científica. Barcelona: Agència d'Avaluació de Tecnologia i Recerca Mèdiques. CatSalut. Departament de Sanitat i Seguretat Social. Generalitat de Catalunya; 2004. [on line] [consulted on 2012/10/20]. Available on http://goo.gl/d2Kvz
- Jansa JM, García de Olalla P. Salud e inmigración: nuevas realidades y nuevos retos. Gac Sanit. 2004;18 Suppl 1:207-13.
- Manzardo C, Trevino B, Gómez i Prat J, Cabezos J, Mongui E, Claveria I, et al. Communicable diseases in the immigrant population attended to in a tropical medicine unit: epidemiological aspects and public health issues. Travel Med Infect Dis. 2008;6(1-2):4-11.
- Salazar A, Navarro-Calderón E, Abad I, Alberola V, Almela F, Borras R, et al. Diagnósticos al alta hospitalaria de las personas inmigrantes en la ciudad de Valencia (2001-2002). Rev Esp Salud Pública. 2003;77(6):713-23.
- Vázquez Villegas J. Inmigración y salud: ¿un nuevo modelo de atención primaria para un nuevo modelo de sociedad? Aten Primaria. 2006;37(5):249-50.
- Gimeno Feliu LA. Aproximación sindrómica al inmigrante según procedencia: África subsahariana. In: Alonso A, Huerga H, Morera J (eds.). Guía de atención al inmigrante, 2.ª ed. Madrid: Ergón; 2006. p. 313-28.
- Cañada JL. Impacto de la inmigración sobre el Sistema Nacional de Salud. 2004 [on line] [consulted on 2012/07/25]. Available on www.fbjoseplaporte.org/rceap/articulo.php?idnum=3&art=03
- Díaz Olalla J. Situación actual de la inmigración. Desigualdades en salud. In: Alonso A, Huerga H, Morera J (eds.). Guía de atención al inmigrante. Madrid: Ergón; 2006. p. 9-24.
- Vázquez Villegas J. Asistencia al inmigrante desde el equipo de atención primaria (aspectos organizativos, formativos y de planificación). Cuadernos de Gestión. 2002;8(2):16-22.
- López Lázaro L. Inmigración, estado de salud y uso de servicios de atención primaria. Aten Primaria. 2008;40(5):232-3.
- Carrasco-Garrido P, De Miguel AG, Barrera VH, Jiménez-García R. Health profiles, lifestyles and use of health resources by the immigrant population resident in Spain. Eur J Public Health. 2007;17(5):503-7.
- Rivera B, Casal B, Cantarero D, Pascual M. Adaptación de los servicios de salud a las características específicas y de utilización de los nuevos españoles. Informe SESPAS 2008. Gac Sanit. 2008;22 Suppl 1:86-95.
- Méndez E. Políticas públicas de acomodación de los inmigrantes en el ámbito sanitario. Quadern CAPS. 2004;32:18-23.
- Jansa JM. Inmigración y envejecimiento, nuevos retos en salud pública. Gac Sanit. 2006;20(Supl 1):10-4.
- Ministerio de Sanidad y Consumo. Encuesta Nacional de Salud de España 2006 [on line] [consulted on 2012/10/20]. Available on www.msc.es/estadEstudios/estadisticas/encuestaNacional/encuestaIndice2006.htm
- Moreno Preciado M. Factores sociales y culturales en el cuidado del inmigrado. Cultura de los cuidados. 2008;23:5-6.
- Gimeno-Feliu LA, Magallón-Botaya R, Macipe-Costa RM, Luzón-Oliver L, Canadá-Millan JL, Lasheras-Barrio M. Differences in the Use of Primary Care Services Between Spanish National and Immigrant Patients. J Immigr Minor Health. 2012 May 22 [Epub ahead of print].
- Gimeno-Feliu LA, Armesto-Gómez J, Macipe-Costa R, Magallon-Botaya R. Comparative study of paediatric prescription drug utilization between the Spanish and immigrant population. BMC Health Serv Res. 2009;9:225.
- Gimeno Feliu LA, Granizo C, Sanz L, Febrel M. Inmigración y salud. Diagnóstico de la realidad. In: Gobierno de Aragón (ed.). Plan integral para la convivencia intercultural en Aragón 2008/2011. Zaragoza; 2009.
- Rue M, Serna MC, Soler-González J, Bosch A, Ruiz-Magaz MC, Galván L. Differences in pharmaceutical consumption and expenses between immigrant and Spanish-born populations in Lleida, (Spain): a 6-months prospective observational study. BMC Health Serv Res. 2008;8:35.
- Regidor E, Sanz B, Pascual C, Lostao L, Sánchez E, Díaz Olalla JM. La utilización de los servicios sanitarios por la población inmigrante en España. Gac Sanit. 2009;23 Suppl 1:4-11.
- Cots F, Xastells X, Ollé C, Manzanera R, Varela J, Vall O. Perfil de la casuística hospitalaria de la población inmigrante en Barcelona. Gac Sanit. 2002;16(5):376-84.
- Carrasco-Garrido P, Jiménez-García R, Barrera VH, de Andrés AL, de Miguel AG. Significant differences in the use of healthcare resources of native-born and foreign born in Spain. BMC Public Health. 2009;9:201.
- Uiters E, Deville W, Foets M, Spreeuwenberg P, Groenewegen PP. Differences between immigrant and non-immigrant groups in the use of primary medical care; a systematic review. BMC Health Serv Res. 2009;9:76.
- Vall-Llosera Casanovas L, Saurina Canals C, Saez Zafra M. Inmigración y salud: necesidades y utilización de los servicios de atención primaria por parte de la población inmigrante en la región sanitaria de Girona. Rev Esp Salud Publica. 2009;83(2):291-307.
- Rodríguez Álvarez E, Lanborena Elordui N, Pereda Riguera C, Rodríguez Rodríguez A. Impacto en la utilización de los servicios sanitarios de las variables sociodemográficas, estilos de vida y autovaloración de la salud por parte de los colectivos de inmigrantes del País Vasco, 2005. Rev Esp Salud Pública. 2008;82(2):209-20.
- Hernández-Quevedo C, Jiménez-Rubio D. A comparison of the health status and health care utilization patterns between foreigners and the national population in Spain: new evidence from the Spanish National Health Survey. Soc Sci Med. 2009;69(3):370-8.
- Nielsen SS, Krasnik A, Rosano A. Registry data for cross-country comparisons of migrants' healthcare utilization in the EU: a survey study of availability and content. BMC Health Serv Res. 2009;9:210.
- Malmusi D, Jansa JM, del Vallado L. Recomendaciones para la investigación e información en salud sobre definiciones y variables para el estudio de la población inmigrante de origen extranjero. Rev Esp Salud Pública. 2007;81(4):399-409.
- Vázquez Villegas J. Atención sanitaria a inmigrantes. Legislación. 2004 [on line] [consulted on 2012/07/25]. Available on www.fbjoseplaporte.org/rceap/articulo.php?idnum=3&art=04
- Hernando Arizaleta L, Palomar Rodríguez J, Márquez Cid M, Monteagudo Piqueras O. Impacto de la inmigración sobre la asistencia hospitalaria: frecuentación, casuística y repercusión económica. Gac Sanit. 2009;23(3):208-15.
- López Nicolás A, Ramos Parreno JM. Utilización de servicios sanitarios por parte de las poblaciones inmigrante y nativa en la Comunidad Autónoma de la Región de Murcia. Gac Sanit. 2009;23 Suppl 1:12-8.
- Buron A, Cots F, García O, Vall O, Castells X. Hospital emergency department utilisation rates among the immigrant population in Barcelona, Spain. BMC Health Serv Res. 2008;8:51.
- Soler-González J, Serna Arnáiz C, Rue Monne M, Bosch Gaya A, Ruiz Magaz MC, Gervilla Cano J. Utilización de recursos de atención primaria por parte de inmigrantes y autóctonos que han contactado con los servicios asistenciales de la ciudad de Lleida. Aten Primaria. 2008;40(5):225-31.
- Esteva M, Cabrera S, Remartínez D, Díaz A, March S. Percepción de las dificultades en la atención sanitaria al inmigrante económico en medicina de familia. Aten Primaria. 2006;37(3):154-9.
- Bras J. Dar peces y enseñar a pescar ¡Cuánto trabajo, madre mía! Aten Primaria. 2005;36(2):69-70.
- Starfield B, van den Berg BJ, Steinwachs DM, Katz HP, Horn SD. Variations in utilization of health services by children. Pediatrics. 1979;63:633-41.
- Orueta JF, López de Muniain J. ¿Es necesario que algunos pacientes nos visiten tan a menudo? Factores asociados con la utilización en pediatría de atención primaria. Gac Sanit. 2000;14:195-202.
- Berra S, Elorza-Ricart JM. Salud y uso de servicios en los sistemas sanitarios en población autóctona e inmigrante de España. Madrid: Plan de Calidad para el Sistema Nacional de Salud. Ministerio de Ciencia e Innovación. Agència d'Avaluació de Tecnologia i Recerca Mèdiques de Cataluña; 2009. Informes de Evaluación de Tecnologías Sanitarias, AATRM Núm. 2007/20082009.
- Ramos M, García R, Prieto M, March J. Problemas y propuestas de mejora en la atención sanitaria a los inmigrantes económicos. Gac Sanit. 2001;15(4):320-6.
- Razum O, Twardella D. Time travel with Oliver Twist-towards an explanation for a paradoxically low mortality among recent immigrants. Trop Med Int Health. 2002;7(1):4-10.
- Gushulak B. Healthier on arrival? Further insight into the "healthy immigrant effect". CMAJ. 2007;176(10):1439-40.
- Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979-2003. Int J Epidemiol. 2006;35(4):903-19.
- Khlat M, Darmon N. Is there a Mediterranean migrants mortality paradox in Europe? Int J Epidemiol. 2003;32(6):1115-8.
- Xu KT, Borders TF. Does being an immigrant make a difference in seeking physician services? J Health Care Poor Underserved. 2008;19(2):380-90.
- Razum O. Commentary: of salmon and time travellers-musing on the mystery of migrant mortality. Int J Epidemiol. 2006;35(4):919-21.
- Razum O, Zeeb H, Rohrmann S. The 'healthy migrant effect'—not merely a fallacy of inaccurate denominator figures. Int J Epidemiol. 2000;29(1):191-2.
- DesMeules M, Gold J, Kazanjian A, Manuel D, Payne J, Vissandee B, et al. New approaches to immigrant health assessment. Can J Public Health. 2004;95(3):I22-6.
- Sanz B, Torres AM, Schumacher R. Características sociodemográficas y utilización de servicios sanitarios por la población inmigrante residente en un área de la Comunidad de Madrid. Aten Primaria. 2000;26(5):314-8.





